Abstract
POEMS syndrome is a rare paraneoplastic syndrome, which includes polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes due to plasma cell (PC) neoplasm. Diagnosis of this disease is challenging because of its rarity and complex clinical manifestations. We attempted to identify the key clinical features and characteristic bone marrow (BM) findings of POEMS syndrome, by reviewing the medical records and BM analyses of 24 Korean patients. Frequent clinical manifestations included polyneuropathy (100%), monoclonal gammopathy (100%), organomegaly (92%), extravascular volume overload (79%), and endocrinopathy (63%). The BM analyses revealed mild PC hyperplasia (median PCs: 5.5%) and frequent megakaryocytic hyperplasia (88%), megakaryocyte clusters (88%), and hyperlobation (100%). Flow cytometry of BM aspirates using CD138/CD38/CD45/CD19/CD56 showed normal (67%, 4/6) or neoplastic PC immunophenotypes (33%, 2/6). A diagnosis of POEMS syndrome must be considered when a patient suspected of having PC dyscrasia shows the above clinical presentation and BM findings.
POEMS syndrome is a rare paraneoplastic syndrome caused by plasma cell (PC) neoplasm, characterized by polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes. Other important clinical features include papilledema, extravascular volume overload, sclerotic bone lesions, Castleman disease, thrombocytosis/erythrocytosis, elevated vascular endothelial growth factor (VEGF) levels, thrombotic diatheses, and abnormal pulmonary function tests [1]. This disease comprises 1–2% of PC dyscrasias [2]. Although the pathogenesis is unclear, disease activity may be related to increased VEGF levels [3].
Its diagnosis is challenging because this is a rare disease and the clinical presentation may be complex. This disease can be misdiagnosed as chronic inflammatory demyelinating polyradiculoneuropathy, monoclonal gammopathy of undetermined significance (MGUS), or neuropathy and immunoglobulin light chain amyloid neuropathy [45]. Correct diagnosis is important because the treatment regimens differ for these diseases, which can be critical for patient outcomes [6]. Although the characteristic bone marrow (BM) findings of POEMS have not been established, a recent study has reported PC rimming around lymphoid aggregates and megakaryocytic hyperplasia in BM biopsies of patients with POEMS syndrome [7]. We attempted to identify the key clinical features and characteristic BM findings of POEMS syndrome. To the best of our knowledge, this is the first comprehensive report on clinical and BM findings for such patients in Korea. This study was approved by the Institutional Review Board of Asan Medical Center, Seoul, Korea (IRB-2015-0328).
We retrospectively reviewed the medical records and BM analyses of 24 patients diagnosed as having POEMS syndrome at Asan Medical Center between December 2002 and July 2016. Their median age was 55 (range: 24–84) years, and the male-to-female ratio was 1.3:1. Clinical factors, such as polyneuropathy (peripheral and sensory or sensorimotor), extravascular volume overload (edema, ascites, or pleural effusion), organomegaly (lymphadenopathy, splenomegaly, or hepatomegaly), endocrinopathy (hypothyroidism, adrenal insufficiency, diabetes mellitus, or hypogonadism), skin changes (hyperpigmentation or hypertrichosis), and associated laboratory and imaging analyses findings were extracted from the medical records and analyzed considering the diagnostic criteria of POEMS syndrome [1]. Four patients who lacked data such as X-ray scans were included because they were highly suspicious of POEMS syndrome clinically.
BM analysis included peripheral blood smear, BM aspirate smear, touch print, clot section, and biopsy section. The peripheral blood smear, BM aspirate smear, and touch print were prepared by Wright-Giemsa stain, and the clot and biopsy sections were prepared by hematoxylin and eosin stain. Immunohistochemistry (IHC) stains were performed on the clot or biopsy sections using monoclonal antibodies specific for CD138, κ, and λ (DAKO, Glostrup, Denmark), according to routine protocols for automated IHC using Ventana Benchmark XT (Ventana Medical Systems, Tucson, AZ, USA). We performed additional IHC stains on the remaining BM biopsy or clot sections for patients without IHC findings and reviewed the BM analyses again. Visual detection of a monoclonal band following serum protein electrophoresis (PEP) was used to confirm the presence of monoclonal protein. The percentage of monoclonal protein was quantified using a densitometer, and the absolute concentrations of monoclonal protein (g/L) were calculated from total serum protein concentrations. The five color-flow cytometric BM aspirate findings using CD138/CD38/CD19/CD45/CD56 were included for six patients. Quantitative data were summarized as median (range) or count and percentage.
The clinical, laboratory, and BM findings are summarized in Tables 1 and 2. The most frequent clinical manifestations included polyneuropathy, monoclonal gammopathy with λ clonality, organomegaly, extravascular volume overload, endocrinopathy, skin changes, and osteosclerotic changes of the bone based on the X-ray or computed tomography scan. Anemia was the most common hematologic abnormality.
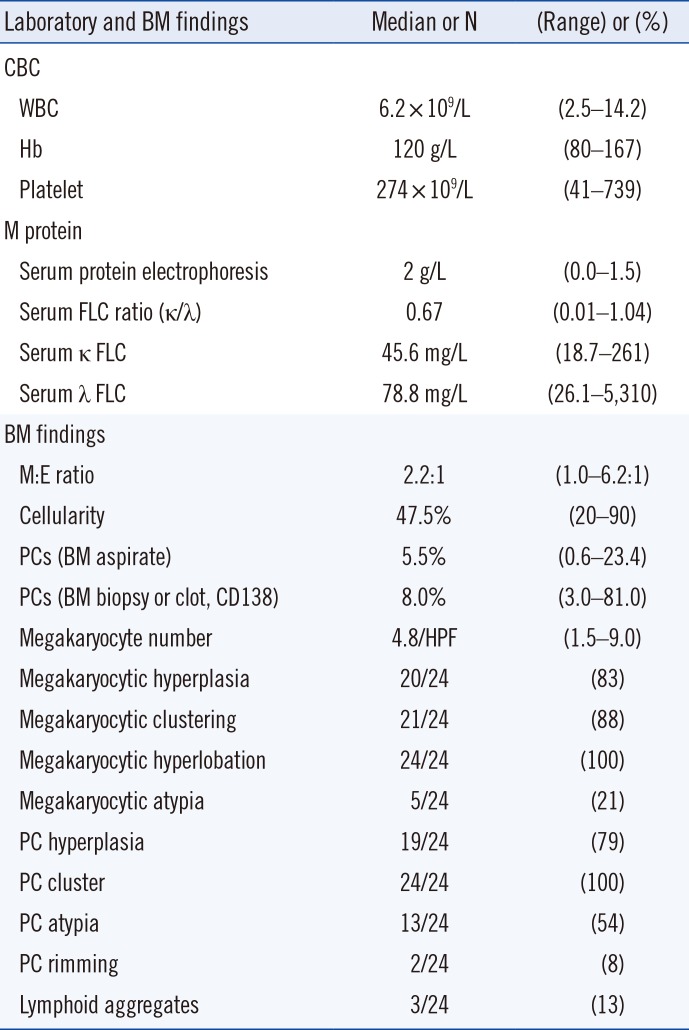
The patients showed variable complete blood counts. M-proteins on serum PEP were found in 18 patients (75%). Serum and urine immunofixation electrophoresis (IFE) revealed monoclonal gammopathy in 22 patients (IgA λ type in 10 patients, IgG λ type in eight patients, and free λ type in four patients). One of the two patients who showed no restriction in serum or urine IFE showed a λ type monoclonal band in cerebrospinal fluid immunoelectrophoresis, and the other patient showed increased serum free κ (34.8 mg/L) and λ chain (86.6 mg/L) and λ clonality in IHC of the BM biopsy. Urine PEP or IFE showed Bence-Jones proteinuria in 13 patients (54%). Serum VEGF levels were checked in four patients, with a median level of 4,070 pg/mL (3,330–6,230 pg/mL; reference range: <500 pg/mL).
In BM analyses, the median proportion of PCs was 5.5% (0.6–23.4) on BM aspirate smears and 8.0% (3.0–81.0; N=17) in the BM biopsies or clot sections (CD138). PC hyperplasia (>3% in BM nucleated cells) was found in 19 patients (79%), PC clusters (at least three PCs localized in a cluster) were found in all patients (100%), and PC atypia, such as multinucleation, was found in 13 patients (54%). Lymphoid aggregates were found in three patients (13%), and PC rimming around the lymphoid aggregate was found in two patients (8%), which did not show any restricted λ or κ clonality (Fig. 1). The myeloid:erythroid (M:E) ratio and cellularity were variable. Megakaryocytic hyperplasia (>4/high-power field [HPF]) was found in 20 patients (83%), including a slight increase (4–6/HPF) in 13 patients (54%) and an overt increase (>6/HPF) in seven patients (29%). Megakaryocyte clusters (at least three megakaryocytes localized in a cluster) were found in 21 patients (88%), megakaryocyte hyperlobation (>8 lobes in the nucleus) in all patients (100%), and megakaryocyte atypia, such as separated nuclei, in five patients (21%).
Flow cytometry of the BM aspirate from six patients revealed a neoplastic immunophenotype (CD138+/CD38+/CD19−/CD45−/CD56+) in two patients and a normal immunophenotype (CD138+/CD38+/CD19+/CD45+/CD56−) in the other four patients. The cytogenetic analyses of the BM aspirates (N=22) showed no chromosomal abnormalities, except for loss of the Y chromosome in one patient, which was probably an age-related event. A lymph node biopsy was performed in six patients:Castleman disease was found in two patients (33%), while the other patients showed reactive hyperplasia.
Management of POEMS syndrome depends on the presence of disseminated BM involvement [8]. BM analysis can be requested to evaluate the extent of POEMS syndrome, but it can also be requested when MGUS needs to be ruled out or a workup for other myeloproliferative conditions, such as erythrocytosis or thrombocytosis, needs to be conducted.
Plasmacytosis (median 5.5% in BM nucleated cells) was mild on BM aspirate smears, consistent with previous reports [79]. The PC counts on BM aspirate smears were lower than that in BM biopsies or clot sections, implying that BM aspirates can be diluted with peripheral blood during the procedure. Lymphoid aggregates (13%, 3/24) were infrequent, and PC rimming around the lymphoid aggregate was polyclonal (8%, 2/24), compared with a previous report in which approximately half of the patients showed monoclonal and polyclonal PC rimming around the lymphoid aggregates [7]. The unusual distribution of clonal PCs relative to the lymphoid aggregates may be the result of immune dysfunction or dysregulation. This finding is unique to POEMS among the PC dyscrasias; various cytokines, other than paraprotein, surrounding the clonal PCs are hypothesized to cause the characteristic distribution [31011].
VEGF appears to play a pathogenic role in this disorder by increasing vascular permeability, angiogenesis, and monocyte/macrophage migration, potentially resulting in arterial obliteration, which is responsible for several findings such as organomegaly, edema, and skin changes in patients with POEMS [10]. Platelets contain numerous proteins that regulate angiogenesis and are a major source of VEGF [12]; megakaryocytic hyperplasia might be related to increased VEGF levels.
Additional characteristic BM findings included megakaryocytic hyperlobation (100%), cluster formation (87%), and hyperplasia (83%). These findings were differentiated from myeloproliferative neoplasm (MPN) due to negative JAK2 V617F [7]. In our study, only two patients had a JAK2 analysis, and the findings were wild-type. Increased VEGF level may affect the maturation and redistribution of megakaryocytes in BM [13]. However, megakaryocytic hyperplasia did not lead to peripheral thrombocytosis in our study, as only 29% showed peripheral thrombocytosis compared with 83% with megakaryocytic hyperplasia in BM.
Our study showed 100% λ clonality, similar to the findings of Dispenzieri [8] (100%), Nakanishi, et al. [14] (95%), and Li, et al. [9] (97%). Monoclonal gammopathy is almost always restricted to λ type monoclonal protein. However, the pathognomonic relationship is yet to be elucidated.
In summary, the characteristic BM findings of POEMS syndrome are mild plasmacytosis and megakaryocytic hyperplasia, hyperlobation, and cluster formation. POEMS syndrome should be considered when a BM analysis is requested for a patient showing clinical symptoms with monoclonal gammopathy.
References
1. Dispenzieri A. POEMS syndrome. Blood Rev. 2007; 21:285–299. PMID: 17850941.
2. Swerdlow SH, Campo E, et al. WHO classification of tumors of haematopoietic and lymphoid tissues. Lyon: IARC Press;2017.
3. Soubrier M, Dubost JJ, Serre AF, Ristori JM, Sauvezie B, Cathebras P, et al. Growth factors in POEMS syndrome: evidence for a marked increase in circulating vascular endothelial growth factor. Arthritis Rheum. 1997; 40:786–787. PMID: 9125266.
4. Chacko JM, Spinner WD. Paraproteinemic neuropathies. J Clin Neuromuscul Dis. 2006; 7:185–197. PMID: 19078807.
5. Lozeron P, Adams D. Monoclonal gammopathy and neuropathy. Curr Opin Neurol. 2007; 20:536–541. PMID: 17885441.
6. Dispenzieri A. POEMS syndrome: update on diagnosis, risk-stratification, and management. Am J Hematol. 2012; 87:804–814. PMID: 22806697.
7. Dao LN, Hanson CA, Dispenzieri A, Morice WG, Kurtin PJ, Hoyer JD. Bone marrow histopathology in POEMS syndrome: a distinctive combination of plasma cell, lymphoid, and myeloid findings in 87 patients. Blood. 2011; 117:6438–6444. PMID: 21385854.
8. Dispenzieri A. POEMS syndrome: 2014 update on diagnosis, risk-stratification, and management. Am J Hematol. 2014; 89:214–223. PMID: 24532337.
9. Li J, Zhou DB, Huang Z, Jiao L, Duan MH, Zhang W, et al. Clinical characteristics and long-term outcome of patients with POEMS syndrome in China. Ann Hematol. 2011; 90:819–826. PMID: 21221584.
10. Gherardi RK, Bélec L, Fromont G, Divine M, Malapert D, Gaulard P, et al. Elevated levels of interleukin-1 beta (IL-1 beta) and IL-6 in serum and increased production of IL-1 beta mRNA in lymph nodes of patients with polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes (POEMS) syndrome. Blood. 1994; 83:2587–2593. PMID: 8167341.
11. Feinberg L, Temple D, de Marchena E, Patarca R, Mitrani A. Soluble immune mediators in POEMS syndrome with pulmonary hypertension: case report and review of the literature. Crit Rev Oncog. 1999; 10:293–302. PMID: 10654928.
12. Koga H, Tokunaga Y, Hisamoto T, Sujaku K, Mitsuyama K, Matsuo K, et al. Ratio of serum vascular endothelial growth factor to platelet count correlates with disease activity in a patient with POEMS syndrome. Eur J Intern Med. 2002; 13:70–74. PMID: 11836087.
13. Pitchford SC, Lodie T, Rankin SM. VEGFR1 stimulates a CXCR4-dependent translocation of megakaryocytes to the vascular niche, enhancing platelet production in mice. Blood. 2012; 120:2787–2795. PMID: 22653973.
14. Nakanishi T, Sobue I, Toyokura Y, Nishitani H, Kuroiwa Y, Satoyoshi E, et al. The Crow-Fukase syndrome: a study of 102 cases in Japan. Neurology. 1984; 34:712–720. PMID: 6539431.
Fig. 1
Bone marrow finding of PCs rimming around a lymphocyte aggregate. (A) The lymphocytic aggregates show a germinal center (H&E stain, ×400). PCs form a rim around the lymphocytic collection detected by immunohistochemistry of (B) CD138, (C) κ, and (D) λ.
Abbreviations: H&E, hematoxylin and eosin; PC, plasma cell.
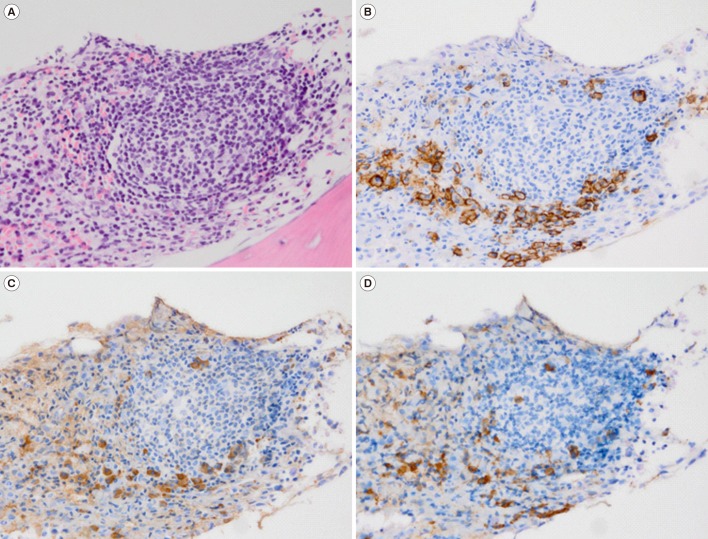
Table 1
Clinical findings of 24 Korean patients with POEMS syndrome
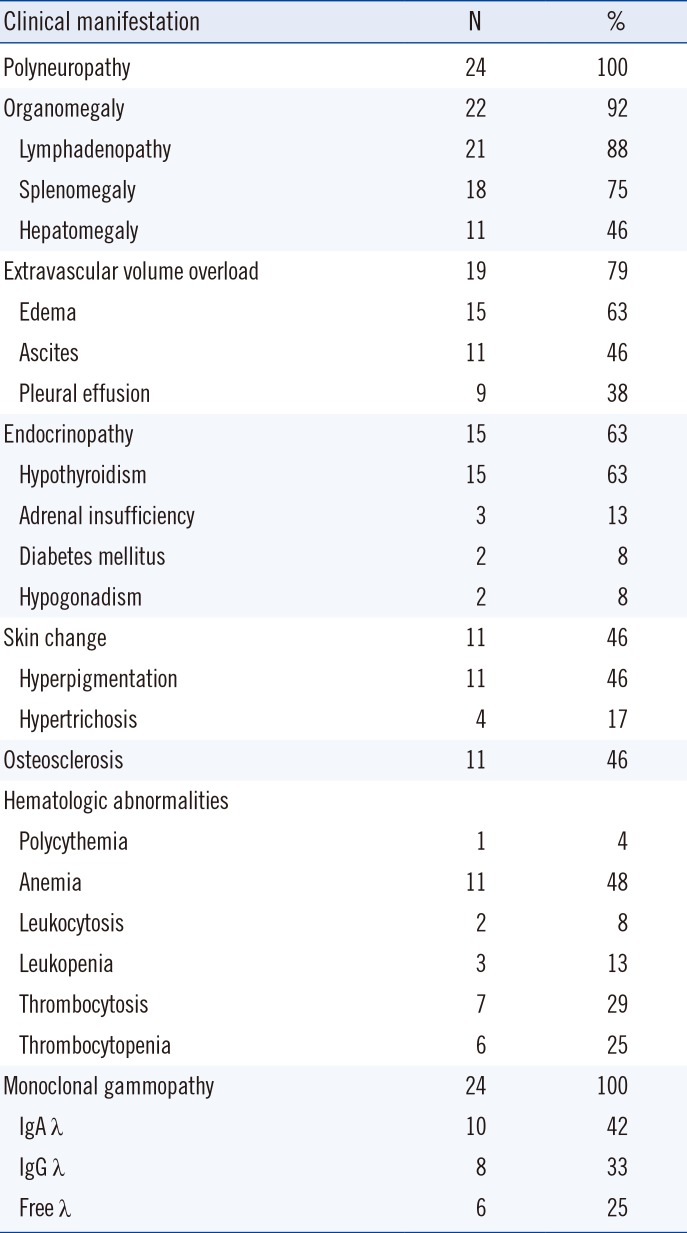
Table 2
Laboratory and BM findings of 24 Korean patients with POEMS syndrome




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download