Introduction
Hypogonadotropic hypogonadism (HH) refers to insufficient gonadal sex steroid production secondary to inadequate pituitary gonadotropin stimulation [
1]. In female patients, HH is clinically characterized by amenorrhea, infertility, and/or delayed sexual development. In addition, a low estrogen environment increases the risk of osteoporosis and bone fracture [
234].
In general, the underlying causes of HH are classified as congenital, functional, or acquired structural; the frequency of each condition is different in patients with primary and secondary amenorrhea [
567]. Functional hypothalamic amenorrhea (HA), the most prevalent form of female HH, is amenorrhea with a diagnosis of exclusion [
8]. When evaluating patients with HH, physicians should exclude the possibility of uncommon but serious structural hypothalamic-pituitary (H-P) abnormalities, such as space-occupying lesions, infiltrative diseases, infections, irradiation, or head trauma [
191011].
The most useful imaging modality to date for the diagnosis of H-P abnormalities is pituitary magnetic resonance imaging (MRI) [
12]; however, because testing is expensive and structural pituitary abnormalities occur at a low frequency, there have been debates regarding whether pituitary MRI should be performed in the routine evaluation of patients with HH [
1314]. Nonetheless, a few studies have reported the efficiency of pituitary MRI in male patients with HH [
13141516], although strategies for determining the necessity of pituitary MRI remain inconclusive. Furthermore, there has been a lack of information regarding the indications for pituitary imaging in female patients with HH.
The objectives of this study were to elucidate the association of pubertal milestones as well as hormonal features with pituitary MRI abnormalities in women with HH, and to identify predictors of abnormal pituitary lesions.
Materials and methods
1. Study samples
We retrospectively analyzed a series of 74 female cases that underwent pituitary MRI during evaluations for HH. The age range of the study population was 14–42 years (mean, 23.9 years). All patients were seen in a gynecological endocrinology clinic at CHA Bundang Medical Center, Gyeonggi-do, Korea, presenting with primary or secondary amenorrhea between July 2000 and October 2015.
All patients were clinically diagnosed with HH based on the findings of primary or secondary amenorrhea, clinical and/or biochemical hypogonadism, and low to normal follicle-stimulating hormone (FSH) levels. Patients with higher basal prolactin levels (>29.2 ng/mL, as stated by reference range) were excluded; however, one patient with a space-occupying lesion with basal prolactin level of 36.0 ng/mL was included in the study. In most cases, the indication for pituitary MRI was HH that persisted more than 6 months or which caused primary amenorrhea without apparent functional causes, including undernutrition, psychological stress, excessive exercise, or chronic illness [
7]. To avoid the high cost of pituitary MRI in undisclosed functional patients with HH, pituitary MRI was performed in patients whose symptoms did not improve after a sufficient period of observation. Accordingly, the duration of symptoms in patients with secondary amenorrhea in the present study was considerably long, with a mean duration of 39.3 months.
2. Clinical, pubertal, and laboratory characteristics
Medical charts were reviewed for body weight, height, body mass index (BMI), type of amenorrhea (primary vs. secondary), and the presence or absence of naturally occurring secondary sex characteristics. Basal serum levels of FSH, luteinizing hormone (LH), prolactin, and thyroid-stimulating hormone (TSH) were assessed in all patients. The serum estradiol level was measured in 58 of 74 patients. In 10 of these patients, an excessively high low-normal limit (>20 pg/mL) had been applied to discriminate very low serum concentrations, such that the results were unsuitable for this study. Therefore, only 48 of 74 patients were appropriately analyzed for serum levels of estradiol. Patients were classified into three groups according to the type of pubertal development: no puberty group (primary amenorrhea with no secondary sex characteristics), interrupted puberty group (primary amenorrhea with naturally occurring secondary sex characteristics), and normal puberty group (secondary amenorrhea with normal secondary sex characteristics).
3. Assessment of pituitary magnetic resonance imaging diagnoses
Patients were classified into three groups according to the pituitary MRI results: normal pituitary MRI group (no abnormal results in the H-P area), space-occupying lesion group (lesions in the H-P area with largest diameter >1.0 cm), and small pituitary gland (PG) group (height of PG <2 standard deviations (SDs) of the age mean) [
17]. As there was no consensus regarding the definition of a ‘small’ PG, we used <2 SDs of age mean for further analysis. Since we excluded patients with hyperprolactinemia, pituitary microadenomas less than 1.0 cm at the largest diameter were infrequently identified in this study. To investigate the characteristics of clinically significant pituitary space-occupying lesions greater than 1 cm in diameter, two patients with non-functioning pituitary microadenomas, with diameters of 3 and 6 mm, respectively, as well as a patient with small Rathke's cyst with a diameter of 4 mm, were included in the normal pituitary MRI group. All MRI scans were re-evaluated by an expert in neuroimaging (S.K.).
4. Statistical analysis
For multiple comparisons, analysis of variance was used, followed by Tukey's honest significant difference test or Games-Howell test. To compare 2 groups of numerical data, the Student's t-test was used. The proportions of various characteristics were compared using the χ2 test or Fisher's exact test. In all cases, P-values <0.05 were considered significant.
Discussion
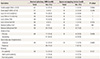
In this study, space-occupying lesions greater than 1 cm in diameter at the H-P area were present in 10.8% of female patients with HH who underwent pituitary MRI scans. In addition, we found no differences in the frequency of low gonadotropin levels, type of amenorrhea, or presence of secondary sex characteristics when comparing patients with space-occupying lesions and those with normal pituitary MRI results. To date, several studies have reported the diagnostic usefulness of pituitary MRI in patients with HH; however, all of these studies were performed in male patients with hypogonadism [
13141516]. To the best of our knowledge, this was the first study to present the frequency of pituitary MRI abnormalities and associated factors in female patients with HH.
Space-occupying lesions at the H-P area is a serious but rare cause of HH. Early diagnosis of large space-occupying lesions in the H-P area is important, because some of the lesions can lead to neurologic sequelae such as bitemporal hemianopia or unilateral optic atrophy due to the compression of the optic chiasm or optic nerve tracts. Reassuringly, however, studies performed in male patients with HH showed a low frequency of clinically significant macroadenoma in the H-P area (0–2.4%) [
13141516]. In 1996, a prospective study of 164 male patients with HH demonstrated the prevalence of total H-P imaging abnormalities and pituitary macroadenoma to be 6.7% (11/164) and 2.4% (4/164), respectively [
13]. Recently, a large retrospective case series of 281 men with HH who underwent pituitary MRIs demonstrated that the prevalence of pituitary microadenoma, macroadenoma, and craniopharyngioma were 8.5%, 1.8%, and 0.4%, respectively [
16].
It was arbitrary to simply compare the results of studies on men with the present results; however, the frequency of large space-occupying lesions in the H-P area in our study (10.7%) was meaningfully higher than expected. Considering the small number of patients and retrospective approach, it was uncertain whether the frequency identified in our study was representative of the actual prevalence of organic H-P disease in female patients with HH. Since our study analyzed only patients who underwent expensive pituitary MRIs during the diagnosis of HH, it has been suggested that the patients with HH included in this study were more likely to have severe clinical symptoms and a longer duration of disease compared to that in patients with HH not included in the study. In fact, the duration of symptoms in 41 patients with secondary amenorrhea in our study was considerably long, with a mean duration of 39.3 months (range, 5–156 months). Such a long duration of amenorrhea might exclude patients with reversible HH such as functional HA, and thereafter increase the frequency of organic brain lesions. Therefore, a large-scale, well-organized prospective study is needed to determine the actual prevalence of significant organic brain lesions in female patients with HH.
There is limited information concerning the clinical and/or biochemical factors associated with pituitary MRI abnormalities in patients with HH. A prospective study in 164 male patients with clinical hypogonadism reported that the risk of H-P imaging abnormalities increased markedly when the serum testosterone level was markedly decreased [
13]. Based on this prior study, Endocrine Society guidelines recommend pituitary imaging be used for men with significant hypogonadism (total testosterone concentrations less than 150 ng/dL) or with concerning neurologic symptoms such as headache or visual disturbance [
12]. However, a subsequent large retrospective case series of 281 male patients reported no difference in testosterone or gonadotropin levels between patients with pituitary MRI abnormalities and those with normal results [
16].
Because the frequency and related factors of pituitary MRI abnormalities have not yet been defined in female patients with HH, guidelines for pituitary imaging have also not yet been established for female patients. The present study analyzed the developmental state of puberty, menstrual state, and hormonal abnormalities between patients with pituitary MR abnormalities and patients with normal MRI results. Therefore, we found no differences in gonadotropin levels, type of amenorrhea, or presence of secondary sex characteristics between patients with space-occupying lesions and those with normal pituitary MRI results. However, the frequency of space-occupying lesions was higher in patients with interrupted puberty (25.0%) compared to that in patients with did not go through puberty (4.8%) or patients with normal puberty (9.8%), although this was not statistically significant.
There is little known clinical significance or diagnostic criteria for small PGs in patients with HH. A case series of 51 men with hypogonadism reported a 17.6% prevalence of small PGs; however, the report did not present the criteria for small PGs used in the study [
14]. With regards to the vertical height of a normal PG, a retrospective study performed in 60 healthy subjects (ages ranging from 8 days to 21 years) reported a pituitary vertical height reference value of 3–7 mm [
18]. However, a large-scale case series of 1,020 subjects (age from 10 to 78 years) found age-related changes in the vertical height of the PG [
17]. In that study, the pituitary vertical height peaked in the 20-to-29-year-old age group, and tended to decline with age. Because there has been no consensus regarding the criteria for small PGs, we used <2 SDs of the age mean for our analysis [
17]. With this criteria, we found small PGs in 18 of 74 female patients with HH, which was similar to a previous study [
14].
The clinical implications of small PGs are still largely unknown; however, several studies have suggested that changes in hormone secretion are reflected in the size of the PG [
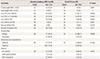
1719]. Furthermore, small PGs in our study were associated with low gonadotropin levels and primary amenorrhea when compared to that in the normal pituitary MRI group (
Table 5). Regardless, no assumptions of causal inference can be drawn from this study. Furthermore, congenital HH, which is a rare genetic condition characterized by inappropriately low gonadotropins, as well as primary amenorrhea [
20] and failure of secondary sexual development were found in 25% of patients in the normal-sized pituitary MRI group in our study (data not shown). Therefore, further studies are needed to determine the relationship between pituitary hormone secretion and pituitary size.
In this study, serum estradiol measurements were not uniformly performed in study subjects. The mean level of serum estradiol in patients who were tested was 21.3±15.5 pg/mL (range, 1.0–63.5 pg/mL), which was consistent with hypogonadism. However, low levels of estrogen milieu were not biochemically confirmed in the 16 patients who were not tested. Although low gonadotropin levels and clinically evident hypogonadism provide a substantial degree of diagnostic accuracy, we could not completely exclude the possibility that these limitations may have affected the accuracy of HH diagnoses in patients who were not tested.
In conclusion, this was the first study to report the frequency of pituitary MRI abnormalities and associated factors in female patients with HH. In our study, no significant clinical, hormonal, or pubertal factors were found to effectively predict space-occupying lesions in patients with HH. However, the frequency of space-occupying lesions was higher in patients with interrupted puberty compared than in no puberty or normal puberty groups. Considering the potential limitations such as the small number of study subjects as well as the retrospective approach, the prevalence of pituitary MRI abnormalities in our study should be verified by further large-scale prospective studies.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download