Abstract
Objectives
To explore changes in self-reported oral health in middle-aged Koreans over a period of 9 years.
Methods
This study design was a cross-sectional analysis. This study analyzed the data of 18,845 middle-aged (45-64 years) subjects who participated in 4-6th Korea National Health and Nutrition Examination Surveys (KNHANES). A complex-sample chi-square test was used to analyze self-reported poor oral health according to sex, household income, and education. A complex-sample logistic regression analysis was used to identify the changes in the factors. SPSS 23.0 and the R ver. 3.5.1 statistical package were used for the analyses.
Results
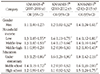
Poor oral health have been decreased by 5.3% over the 9-year period. Middle-aged men were more likely to report their oral health as worse than women. The lower income and education groups reported their oral health as poor compared to the higher income and education groups. The factors affecting self-reported poor oral health over the 9-year period were sex, income, and education.
References
1. Statistics Korea. 2016 statistics on the aged [Internet]. Seoul: Statistics Korea;2016. Cited 2018 December 15. Available from: http://kostat.go.kr/portal/korea/kor_nw/1/6/1/index.board?bmode=read&aSeq=356426.
2. Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005; 83:661–669.
3. López R, Smith PC, Göstemeyer G, Schwendicke F. Ageing, dental caries and periodontal diseases. J Clin Periodontol. 2017; 44:Suppl 18. S145–S152.

4. Jin LJ, Lamster IB, Greenspan JS, Pitts NB, Scully C, Warnakulasuriya S. Global burden of oral diseases: emerging concepts, management and interplay with systemic health. Oral Dis. 2016; 22:609–619.

5. Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005; 33:81–92.

6. Saintrain MV, de Souza EH. Impact of tooth loss on the quality of life. Gerodontology. 2012; 29:e632–e636.

7. Dahl KE, Calogiuri G, Jönsson B. Perceived oral health and its association with symptoms of psychological distress, oral status and socio-demographic characteristics among elderly in Norway. BMC oral health. 2018; 18:93–100.

8. Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J Epidemiol Community Health. 2003; 57:778–783.

9. Lewis A, Wallace J, Deutsch A, King P. Improving the oral health of frail and functionally dependent elderly. Aust Dent J. 2015; 60:Suppl 1. S95–S105.

10. Moon SH, Hong Son GR. Predictors of chewing discomfort among community-dwelling elderly. J Korean Acad Community Health Nurs. 2017; 28:302–312.

11. Locker D, Clarke M, Payne B. Self-perceived oral health status, psychological well-being, and life satisfaction in an older adult population. J Dent Res. 2000; 79:970–975.

12. Vigu AL, Stanciu D, Lotrean LM, Campian RS. Complex interrelations between self-reported oral health attitudes and behaviors, the oral health status, and oral health-related quality of life. Patient Prefer Adherence. 2018; 12:539–549.

13. Klotz AL, Tauber B, Schubert AL, Hassel AJ, Schröder J, Wahl HW, et al. Oral health-related quality of life as a predictor of subjective well-being among older adults-A decade-long longitudinal cohort study. Community Dent Oral Epidemiol. 2018; 46:631–638.

14. Kim SY, Kim JE, Kim HN, Jun EJ, Lee JH, Kim JS, et al. Association of self-perceived oral health and function with clinically determined oral health status among adults aged 35-54 Years: A cross-sectional study. Int J Environ Res Public Health. 2018; 15:E1681.

15. Jang JH. The effects of oral hygiene care behavior and attitude on the number of natural teeth after middle aged people. KLAR. 2006; 3:79–90.
16. Telford C, Coulter I, Murray L. Exploring socioeconomic disparities in self-reported oral health among adolescents in California. JADA. 2011; 142:70–78.

17. Li KY, Okunseri CE, McGrath C, Wong MCM. Trends in selfreported oral health of US adults: National Health and Nutrition Examination Survey 1999-2014. Community Dent Oral Epidemiol. 2018; 46:203–211.

18. Jung MH, Kim SS, Kim YS, Ahn ES. Relationship of socioeconomic status to self-rated oral health. J Dent Hyg Sci. 2014; 14:207–213.
19. Mamai-Homata E, Koletsi-Kounari H, Margaritis V. Gender differences in oral health status and behavior of Greek dental students: A meta-analysis of 1981, 2000, and 2010 data. J Int Soc Prev Community Dent. 2016; 6:60–68.

20. Hamasha AA, Alshehri A, Alshubaiki A, Alssafi F, Alamam H, Alshunaiber R. Gender-specific oral health beliefs and behaviors among adult patients attending King Abdulaziz Medical City in Riyadh. Saudi Dent J. 2018; 30:226–231.

21. Kim CS, Han SY, Lee SE, Kang JH, Kim CW. Dental care utilization for examination and regional deprivation. J Prev Med Public Health. 2015; 48:195–202.

22. Hakeberg M, Wide Boman U. Self-reported oral and general health in relation to socioeconomic position. BMC Public Health. 2017; 18:63–70.

23. Shin HS. Social gradients in oral health status in Korea population. Arch Oral Biol. 2018; 95:89–94.

25. Kim YT, Lee JH, Kweon HI, Lee JS, Choi JK, Kim DW, et al. Evaluation of national health insurance coverage of periodontal scaling: A nationwide cohort study in Korea. J Korean Dent Assoc. 2016; 54:604–612.
26. Kim HN, Kim CB, Kim NH. Changes in factors on unmet dental scaling rate according to the national health insurance coverage. J Korean Soc Dent Hyg. 2017; 17:539–551.

27. Ministry of Health and Welfare. 2017 Outline of budget and fund management plan [internet]. 2017. Cited 2018 December 15. Available from: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download