Abstract
Background
Catheter-associated urinary tract infection is a major infection in healthcare facilities. We investigated the urinary catheter utilization ratio and incidence of catheter-associated urinary tract infections in small-sized hospitals with ≤300 beds.
Methods
We recruited hospitals via a web-based survey from July 2016 to September 2016. Infection control practitioners provided data about catheter-associated urinary tract infections on the website according to the prescribed form. The urinary catheter utilization ratio was calculated by dividing the number of device-days by the number of patient-days. The incidence of catheter-associated urinary tract infections per 1,000 device-days was calculated by dividing the number of urinary tract infections in patients with indwelling urinary catheter by the number of indwelling device-days and multiplying by 1000. The urinary catheter utilization ratio and incidence of catheter-associated urinary tract infections were compared between hospitals with >200 beds and ≤200 beds.
Results
Twenty-seven hospitals were included. The average urinary catheter utilization ratio was 0.4 (0.47 in hospitals with >200 beds and 0.38 in hospitals with ≤200 beds; P=0.1). The incidence of catheter-associated urinary tract infections was 1.59 per 1,000 device-days. There was no significant difference in the incidence of infections according to the number of beds (1.53 in hospitals with >200 beds vs 1.9 in hospitals with ≤200 beds, P=0.421).
Catheter-associated urinary tract infection (CAUTI) is one of the major infections in healthcare facilities [12]. Urinary catheter is the most common indwelling device [3]. With this device, approximately 3-10% of bacteriuria occur per day of catheterization, and among these bacteria, around 10-24% cause symptoms of urinary tract infection (UTI) [4567]. This infection leads to significant burden in morbidity and health care expenditure [12].
In South Korea, the Korean National Healthcare-associated Infections Surveillance System (KONIS) has been established to identify the actual incidence of CAUTI, and they targeted domestic hospitals that voluntarily participated and were being funded by the Korean Centers for Disease Control (KCDC) since 2006 [8]. KONIS reported that among hospitals which had over 300 beds, even urinary catheter utilization ratio (UCR) was low in smaller-sized hospital, the rate of CAUTI was not significantly different from that of larger-sized hospital [9]. This phenomenon is attributable to the limitations in infection control and surveillance of CAUTI due to the lack of knowledge, support resources, and time in small-sized hospitals. Infection control and surveillance are more challenging in small-sized hospitals, which increases the risk of CAUTI among patients.
Although the KONIS collected data from hospitals with >200 beds, the surveillance data obtained from small-sized hospitals in Korea was still limited. Thus, in this study, we further expanded the surveillance on small-sized hospitals with <200 beds. This study investigated the UCR and incidence of CAUTI in small-sized hospitals with ≤300 beds using a web-based surveillance system.
We prospectively conducted a web-based surveillance study to improve the project funded by the KCDC. Twenty-seven hospitals with ≤300 beds in Korea voluntarily participated in this study from July 2016 to September 2016.
During the study period, infection control practitioners at each hospital were trained three times about diagnostic criteria, data input method, and infection monitoring method. The infection control practitioners filled out the characteristics of the hospital (location, bed size, monitored department, and availability of microbiological examination) and data on CAUTI (use of indwelling urinary catheter; clinical symptoms, such as fever ≥38℃, urgency, frequency, dysuria, suprapubic tenderness, and costovertebral angle pain or tenderness; insertion date of urinary catheter; date of CAUTI occurrence; causative pathogen; and antimicrobial susceptibility) on the website according to the prescribed form.
Etiologic pathogens and antimicrobial susceptibility were determined according to each hospital's and entrusted institution's microbial identification methods.
The definition of CAUTI was based on the 2016 KONIS manual [10]. In all patients with urinary catheter, including those whose urinary catheters were removed within 48 hours, CAUTI was defined as follows: presence of at least one of the following signs or symptoms that could not be explained by other causes (fever ≥38℃, urgency, frequency, dysuria, suprapubic tenderness, and costovertebral angle pain or tenderness) along with a positive urine culture (≥105 CFUs/mL) with ≤2 bacterial species or at least one positive outcome in the dipstick test, presence of pyuria, and positive gram stain. Indwelling urinary catheter only included Foley catheter via the urethra.
The UCR was calculated by dividing the number of device-days by the number of patient-days. The incidence of CAUTI per 1000 device-days was calculated by dividing the number of UTIs in patients with indwelling urinary catheter by the number of indwelling device-days and multiplying by 1000. The UCR and incidence of CAUTI were compared between hospitals with >200 beds and ≤200 beds. The duration from the insertion of indwelling urinary catheter (IUC) to the occurrence of CAUTI was calculated. Based on the report that prolonged urinary catheterization, particularly >6 days, was a risk factor of CAUTI, the proportion of patients with such infection was analyzed by classifying them according to the duration of urinary catheter as ≤6 and >6 days with the day of urinary catheter insertion set as day 1 [1112131415].
Statistical significance was assessed via the chi-square test or Fisher's exact test for categorical variables. Continuous variables were analyzed using independent t-test or the Mann–Whitney U test. A P-value <0.05 was considered statistically significant. Statistical analysis was performed using the Statistical Package for the Social Sciences software version 20 (IBM SPSS Inc., Armonk, NY, the USA).
Table 1 shows the characteristics of the participating hospitals. A total of 27 hospitals were included in this study. Based on bed size, 16 (59.3%) hospitals had 201–300 beds, 10 (37.0%) had 101-200 beds, and one (3.7%) had ≤100 beds. The median bed size was 223 beds. The intensive care units (ICU) (n=26, 96.3%) were mostly monitored and one (3.7%) general ward was also monitored. The median number of monitored beds was 12 (range: 9–86). Microbiological results could be acquired by external entrustment (n=18, 66.7%) and in-hospital examination (n=9, 33.3%).
The UCR was 0.4 in this study (Table 2). The UCR in hospitals with >200 beds and ≤200 beds was 0.47 and 0.38, respectively. The result was not statistically significant (P=0.1).
During the study period, a total of 28 CAUTI were identified. The incidence of CAUTI was 1.59 per 1,000 device-days (Table 3). In hospitals with >200 beds, the incidence of CAUTI was 1.53 (n=20), and in hospitals with ≤200 beds, the incidence was 1.9 (n=8) without significance (P=0.421).
The median duration from the insertion of IUC to the occurrence of CAUTI was 12 days. In total, 21 (75.0%) CAUTI occurred after 6 days of catheterization, and 7 (25.0%) CAUTI occurred within 6 days of catheterization.
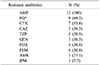
The main causative pathogens of CAUTI are shown in Table 4. Klebsiella pneumoniae (n=7, 25.0%) is the leading cause of infections, followed by Enterococcus faecium (n=6, 21.4%) and Escherichia coli (E.coli; n=4, 14.3%). Data on antimicrobial susceptibility was obtained only from 13 CAUTI, which were all caused by Enterobacteriaceae (Table 5). All Enterobacteriaceae were resistant to ampicillin. Approximately 69.2% (n=9) and 53.8% (n=7) of bacteria were resistant to fluoroquinolone and cefotaxime, respectively. One CAUTI (7.7%) was resistant to imipenem.
In this study, we examined the UCR and incidence of CAUTI in small-sized hospitals with ≤300 beds. We further compared the differences according to the number of hospital beds.
Data that focused on small-sized hospitals were limited. During the same study period, the incidence of CAUTI was 0.93 per 1,000 device-days in hospitals with 200-299 beds based on the KONIS data [16]. The present study showed that the incidence of CAUTI was 1.59 per 1,000 device-days in hospitals with ≤300 beds and in hospitals with only 201-300 beds, the incidence was 1.53 per 1,000 device- days. These findings suggested that the incidence of CAUTI in small-sized hospitals was higher than estimated with hospitals registered to the KONIS. In the United States, the overall incidence of CAUTI was 1.62 per 1,000 device-days in the ICUs of hospitals with 50–457 beds from 2010 to 2011 [17]. Although direct comparisons are challenging because that study included hospitals with >300 beds, this result showed that the incidence of CAUTI was lower than the United States. However, data on the incidence of CAUTI in the United States was from 2010 and 2011, and considering the decreasing trend of CAUTI via surveillance, the incidence was likely similar to that of the United States [2].
The KONIS data showed that the rate of CAUTI was not significantly different between small- and large-sized hospitals, although the UCR was low in small-sized hospitals [9]. Although the result was not statistically significant, hospitals with ≤200 beds had tendency of lower UCR (0.38 in hospitals with ≤200 beds and 0.47 in hospitals with >200, respectively) and higher incidence of CAUTI (1.9 in hospitals with ≤200 beds and 1.53 in hospitals with >200, respectively) that of hospitals with >200. Our result was consistent with that of a previous report [9].
In this study, the major pathogen that causes CAUTI was Enterobacteriaceae. Approximately 69.2% and 53.8% of bacteria were resistant to fluoroquinolone and cefotaxime, respectively. Of the Enterobacteriaceae, 38.5% were resistant to ceftazidime and 30.5% to cefepime. In hospitals with >300 beds in Korea, 64.9% and 47.4% of E.coli isolated from CAUTI were resistant to ciprofloxacin and cefotaxime in 2013, respectively [18]. Of the E.coli isolated from CAUTI that was reported by the United States National Healthcare Safety Network in 2014, 35% and 16% were resistant to fluoroquinolone and anti-pseudomonal cephalosporins, respectively [19]. The rate of resistance to antibiotics in CAUTI was higher in Korea than in the United States. In addition, compared with community- onset acute pyelonephritis, which was 9.3% and 21.3% resistant to cefotaxime and fluoroquinolone, respectively, antibiotic resistance in CAUTI is considerable. Thus, efforts must be exerted in preventing CAUTI.
The prolonged use of urinary catheter is the most important risk factor of CAUTI, particularly >6 days of catheterization [1112131415]. In this study, 75% of CAUTI occurred after 6 days of catheterization. For the prevention of CAUTI, the use and duration of urinary catheterization must be reduced [20]. Medical staff often did not recognize the presence of IUC [21]. A systematic review has presented that the mean duration of catheterization decreased by 37% and that the rate of CAUTI was reduced by 52% with the use of a reminder or stop order for IUC [22]. The monitoring system used in determining whether a catheter can be removed would be efficient in reducing the incidence of CAUTI.
In small-sized hospitals, the number of infection control practitioners is low. In South Korea, one infection control doctor per 300 beds and one infection control nurse per 200 beds were recommended by appropriating the infection prevention control charge [23]. This law applies only to hospitals with >150 beds. In addition, it is difficult to obtain such personnel at small-sized hospitals due to the lack of infection control specialist. In hospitals participated in this study, 7 (63.6%) hospitals let infection control practitioner have other tasks besides infection control work and all of them were hospitals with ≤200. Furthermore, infection control practitioners monitored average 26.9 beds in hospitals with ≤200 beds and 12.8 beds with >200 beds. Even if the ward was excluded, monitored beds were higher as 19.5 in hospitals with ≤200 beds. This lack of workforce and work overload makes infection control more challenging, which likely leads to an increase in infection rates. Since CAUTI had decreased since the introduction of the infection surveillance and education program of KONIS, it is believed that the infection rate might be reduced through opportunities for active infection surveillance and education even in small-sized hospitals [9]. With the recruitment of manpower, the scope of surveillance in small-sized hospitals must be gradually expanded. To achieve this, a systematic program must be established to increase the number of infection control practitioners and strengthen their capacity.
During the study period, education about infection control targeting infection control practitioners was conducted three times. After education, we collected the opinions of infection control practitioners about education and the limitation of the infection monitoring system via an anonymous, self-administered, structured questionnaire prepared in Korean. Through education, 79.1% of infection control practitioners responded that they can learn more about UTI and apply this theorical knowledge in clinical practice. This result suggested that education program was relatively effective in improving the quality of infection control. Some pointed out that the application of their knowledge to clinical practice was challenging due to the lack of manpower and laboratory examinations and limitation in obtaining clinical data. This showed the importance of increasing educational opportunities. Moreover, without manpower and computerized system as back-up, there will be limitations in improvements.
The present study had several limitations. First, most of the departments included in this study were ICUs. However, one (3.7%) general ward was included, and it was difficult to generalize the results to all hospital departments. Second, the infection data might be missing or misidentified because all data were collected by infection control practitioners. Although the infection control practitioners were taught about the selection and input of infection cases, the infection rates might be inaccurate because not all infection control practitioners were fluent.
The incidence of CAUTI in small-sized hospitals was substantial high. Efforts must be exerted in lowering infection rates through proper infection control and monitoring. In addition, measures in improving manpower and education on infection control should be implemented.
Figures and Tables
Acknowledgements
This research was supported by a fund from the research of the Korea Centers for Disease Control and Prevention.
The authors have no potential conflicts of interest to disclose.
References
1. Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014; 370:1198–1208.

2. Nicolle LE. Catheter associated urinary tract infections. Antimicrob Resist Infect Control. 2014; 3:23.

3. Centers for Disease Control and Prevention. Healthcare-associated infections. Updated on 16 October 2015. https://www.cdc.gov/hai/ca_uti/uti.html.
4. Warren JW, Platt R, Thomas RJ, Rosner B, Kass EH. Antibiotic irrigation and catheter-associated urinary-tract infections. N Engl J Med. 1978; 299:570–573.

5. Leuck AM, Wright D, Ellingson L, Kraemer L, Kuskowski MA, Johnson JR. Complications of Foley catheters--is infection the greatest risk? J Urol. 2012; 187:1662–1666.

6. Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000; 28:68–75.

7. Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1,497 catheterized patients. Arch Intern Med. 2000; 160:678–682.

8. Lee SO, Kim S, Lee J, Kim KM, Kim BH, Kim ES, et al. Korean Nosocomial Infections Surveillance System (KONIS) report: data summary from july through september 2006. Korean J Nosocomial Infect Control. 2006; 11:113–128.
9. Kwak YG, Choi JY, Yoo H, Lee SO, Kim HB, Han SH, et al. Korean National Healthcare-associated Infections Surveillance System, intensive care unit module report: summary of data from July 2014 through June 2015. Korean J Healthc Assoc Infect Control Prev. 2016; 21:37–49.

10. KONIS system. KONIS 2018 ICU manual. Updated on 27 July 2018. http://konis.cafe24.com/xe/index.php?mid=manual&category=251.
11. Leone M, Albanèse J, Garnier F, Sapin C, Barrau K, Bimar MC, et al. Risk factors of nosocomial catheter-associated urinary tract infection in a polyvalent intensive care unit. Intensive Care Med. 2003; 29:1077–1080.

12. Leelakrishna P, Karthik Rao B. A study of risk factors for catheter associated urinary tract infection. Int J Adv Med. 2018; 5:334–339.

13. Talaat M, Hafez S, Saied T, Elfeky R, El-Shoubary W, Pimentel G. Surveillance of catheter-associated urinary tract infection in 4 intensive care units at Alexandria university hospitals in Egypt. Am J Infect Control. 2010; 38:222–228.

14. Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997; 11:609–622.

15. Stark RP, Maki DG. Bacteriuria in the catheterized patient. What quantitative level of bacteriuria is relevant? N Engl J Med. 1984; 311:560–564.
16. KONIS system. ICU reports. Updated on 9 August 2018. http://konis.cafe24.com/xe/reports_icu_y.
17. Lewis SS, Knelson LP, Moehring RW, Chen LF, Sexton DJ, Anderson DJ. Comparison of non-intensive care unit (ICU) versus ICU rates of catheter-associated urinary tract infection in community hospitals. Infect Control Hosp Epidemiol. 2013; 34:744–747.

18. Choi JY, Kwak YG, Yoo H, Lee SO, Kim HB, Han SH, et al. Korean Nosocomial Infections Surveillance System. Trends in the distribution and antimicrobial susceptibility of causative pathogens of device-associated infection in Korean intensive care units from 2006 to 2013: results from the Korean Nosocomial Infections Surveillance System (KONIS). J Hosp Infect. 2016; 92:363–371.

19. Weiner LM, Webb AK, Limbago B, Dudeck MA, Patel J, Kallen AJ, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011-2014. Infect Control Hosp Epidemiol. 2016; 37:1288–1301.

20. Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010; 31:319–326.

21. Saint S, Wiese J, Amory JK, Bernstein ML, Patel UD, Zemencuk JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000; 109:476–480.

22. Meddings J, Rogers MA, Macy M, Saint S. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis. 2010; 51:550–560.

23. Ministry of Healthcare and Welfare. Updated on 30 March 2018. http://www.mohw.go.kr/react/index.jsp.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download