Abstract
A 68-year-old man presented at the emergency room with sudden blindness. The day before, he had eaten sashimi and eel and drank alcohol for dinner. He experienced nausea, vomiting, and dizziness afterward. His medical history included hypertension and diabetes, and the latter was treated with metformin. Initial laboratory tests revealed severe metabolic acidosis (lactic acidosis). Massive hydration and intravenous sodium bicarbonate replacement therapies were initiated, but severe metabolic acidosis (lactic acidosis) did not resolve, in turn, leading to hemodialysis, which decreased metabolic acidosis. The patient's blindness improved, and his vision gradually recovered. As it is not easy to distinguish between blindness related to metformin-associated lactic acidosis (MALA) and blindness related to other causes, rapid correction of metabolic acidosis through hemodialysis might be helpful in differentiating this from of blindness from blindness related to other causes.
Metformin is the most commonly used oral hypoglycemic agent in patients with diabetes. The frequently reported adverse effects of metformin are gastrointestinal side effects, including nausea, vomiting, and diarrhea1). Lactic acidosis may occur as a serious adverse reaction to metformin and should be considered as a factor contributing to decreased renal function in some patients2). The reported incidence of metformin-associated lactic acidosis (MALA) is 4.3 cases/100,000 patient-years, mostly in patients with predisposing factors3). In cases of lactic acidosis caused by metformin, the drug is stopped, and hemodialysis is performed when necessary4). We report a case of MALA that resulted in transient blindness.
A 68-year-old man with sudden blindness presented at our emergency room. The day before, he had eaten sashimi and eel, and drank alcohol for dinner. Afterward, he experienced nausea, vomiting, and dizziness. His medical history included diabetes and hypertension. His diabetes, diagnosed more than 20 years ago, was at the time treated with metformin 1,000mg twice a day, glimepiride 2mg once a day, and linagliptin 5mg once a day. Concurrently, his hypertension was treated with telmisartan 80mg/amlodipine 5mg once a day.
At the time of admission to the emergency room, the patient's blood pressure was 104/57mmHg, heart rate 86 beats/min, body temperature 34.3℃, and the pulse oximeter reading was 98% on room air. The patient was alert and although the light reflex was intact, the patient reported seeing no light in either eye even when a penlight was shone into the eyes. No other focal neurological deficits were observed.
Brain computed tomography (CT) and brain magnetic resonance imaging & angiography (MRI & MRA) were performed. Brain CT and MRI showed no acute lesions. No significant stenosis of the cerebral artery was seen on MRA.
The first venous blood gas analysis (VBGA) test at admission showed pH, 6.78; pCO2, 26.7mmHg; pO2, 38 mmHg; bicarbonate, 4.0mmol/L; and total CO2<5 mmol/L. The first arterial blood gas analysis (ABGA) test showed pH, 6.93; pCO2, 16mmHg; pO2, 120mmHg; bicarbonate, 3.4mmol/L; total CO2, 4mmol/L; and SaO2, 95%. The initial laboratory data revealed the following: white blood cell (WBC), 35,300/µL; hemoglobin (Hb), 15.0 g/dL; platelets, 284,000 K/µL; BUN, 36.8mg/dL; creatinine, 2.31mg/dL; sodium 141.1mEq/L; potassium, 5.80mEq/L; chloride, 99.2mEq/L; total calcium, 9.9 mg/dL; phosphorus, 11.6mg/dL. Lactic acid was measured as >11mmol/L on admission. Urinalysis showed protein 2+, glucose −, and ketone 1+, and urine microscopy showed red blood cell (RBC) 3–5/HPF and WBC 6–10/HPF.
Massive hydration and intravenous sodium bicarbonate replacement were initiated for severe metabolic acidosis (lactic acidosis), but the metabolic acidosis did not change. Nevertheless, after three hours of hydration and sodium bicarbonate supplementation, while the metabolic acidosis remained unchanged, the patient's vision gradually recovered.
After 30 minutes of visual recovery, an ophthalmologic examination was performed. Diabetic retinopathy and cataract were found. No lesions that would cause blindness were identified (Fig. 1).
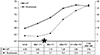
Although field of vision and visual acuity were restored, metabolic acidosis did not resolve completely (pH, 7.11; pCO2, 18mmHg; pO2, 77mmHg; bicarbonate, 5.7 mmol/L; total CO2, 6mmol/L; SaO2, 93% on ABGA). Hemodialysis (HD) was performed once, which resulted in decreased metabolic acidosis (pH, 7.49; pCO2, 30mmHg; pO2, 111mmHg; bicarbonate, 22.9mmol/L; total CO2, 23.8mmol/L; SaO2, 99% on ABGA). Figure 2 shows change in vital signs after admission. Figure 3 shows changes in metabolic acidosis and after admission.
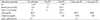
Table 1 shows the results of the tests performed during hospitalization. The patient did not undergo any further hemodialysis after admission. Metformin was discontinued, glimepiride was increased, and the patient was discharged after 6 days of hospitalization.
Metformin is the most commonly used oral hypoglycemic agent in diabetes1). However, when used in patients with renal impairment or other comorbid conditions, metformin may cause lactic acidosis, which can be a life-threatening condition 2).
The mechanism of MALA is complex. Metformin promotes the conversion of glucose to lactate in the splanchnic bed of the small intestine5). Metformin also inhibits mitochondrial respiratory chain complex 1, leading to decreased hepatic gluconeogenesis from lactate, pyruvate, and alanine. This results in additional lactate and substrate for lactate production67).
It is not easy to distinguish between blindness related to MALA and blindness related to other causes. In previous cases, reversible blindness due to lactic acidosis was reported in diabetic patients89); a case of transient blindness due to diabetic ketoacidosis (DKA) and due to alcoholic ketoacidosis have also been reported1011). The common features of these cases were severe metabolic acidosis with pH <7.0 and bicarbonate <5.0mmol/L, and restoration of visual acuity after metabolic acidosis was corrected (Table 2). Therefore, in cases of sudden blindness in patients with severe metabolic acidosis, rapid correction of metabolic acidosis through hemodialysis may be helpful in differentiating this form of blindness from blindness related to other causes.
Transient blindness due to MALA is very rare and related risk factors are difficult to assess. Patients with severe metabolic acidosis (pH <7.0 and bicarbonate <5 mmol/L) in previously reported cases were compared. Hypothermia was present in our case and in another case, and hypotension was present in some cases (Table 2). Further investigation of associated risk factors is needed.
Our patient, unlike the previously reported MALA case, recovered his vision before metabolic acidosis was corrected with dialysis (pH, 7.11; pCO2, 18mmHg; pO2, 77 mmHg; bicarbonate, 5.7 mmol/L; total CO2, 6 mmol/L; SaO2, 93% on ABGA) (Fig. 3). However, in a case of an alcoholic ketoacidosis patient, visual acuity was restored after hydration and intravenous sodium bicarbonate replacement11). This observation notwithstanding, in this case report, the degree of correction of metabolic acidosis was not reported.
In the present case, loss of vision could have resulted from two factors: hypotension and superimposed metabolic acidosis. According to previously published reports, vision loss associated with MALA improved after correction of metabolic acidosis101112). The reported cases also showed the same pattern as our case with pH <7.0. Based on animal studies, the suggested mechanism involves the following: retinal cell function may be pH-dependent; retinal horizontal cell response to light is pH-sensitive; and mammalian retinal cell function becomes disrupted at pH <7.09). These effects could extend to humans and may serve as an explanation for acidosis-associated vision loss and optic nerve ischemia13).
MALA is a common metformin-related adverse reaction. However, blindness associated with MALA has not been reported frequently. If blindness is accompanied by severe metabolic acidosis (pH <7.0, bicarbonate <5 mmol/L) associated with MALA, and if the cause of blindness is not clear, physicians should consider correcting metabolic acidosis through early hemodialysis. This approach could help distinguish blindness related to MALA from blindness related to other causes, and prevent retinal ischemia13).
Figures and Tables
Fig. 1
Fundoscopic examination. (A) Right eye, a dot-like retinal hemorrhage was observed (red circle), (B) Left eye, a dot-like retinal hemorrhage (red circle) and hard exudate (arrow) were observed, showing severe non-proliferative diabetic retinopathy.

References
1. American Diabetes Associatation. 8. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes-2018. Diabetes Care. 2018; 41:Suppl 1. S73–S85.
2. IRF. van Berlo-van de Laar IRF, Vermeij CG, Doorenbos CJ. Metformin associated lactic acidosis: incidence and clinical correlation with metformin serum concentration measurements. Journal of Clinical Pharmacy and Therapeutics. 2011; 36:376–382.

3. Salpeter SR, Greyber E, Pasternak GA, et al. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. 2010; 14(4):CD002967.

4. Lalau JD, Andrejak M, Morinier P, et al. Hemodialysis in the treatment of lactic acidosis in diabetics treated by metformin: a study of metformin elimination. Int J Clin Pharmacol Ther Toxicol. 1989; 27(6):285–288.
5. Bailey CJ, Wilcock C, Day C. Effect of metformin on glucose metabolism in the splanchnic bed. Br J Pharmacol. 1992; 105(4):1009.

6. Vecchio S, Giampreti A, Petrolini VM, et al. Metformin accumulation: lactic acidosis and high plasmatic metformin levels in a retrospective case series of 66 patients on chronic therapy. Clin Toxicol(Phila). 2014; 52(2):129–135.

7. Sirtori CR, Pasik C. Re-evaluation of a biguanide, metformin: mechanism of action and tolerability. Pharmacol Res. 1994; 30(3):187.

8. Sprensen PN. Transitory blindness during ethanol and phenethylbiguianide induced lactic acidosis in a subject with diabetes mellitus. A case report. Acta Ophthalmol (Copenh). 1977; 55(2):177–182.
9. Cicarran S, Rodriquez ML, Pousa M, et al. Transient vision loss in a patient with severe metformin-associated lactic acidosis. QJM. 2012; 105(8):781–783.

10. Deutsch G. Transient blindness associated with severe diabetic ketoacidosis. Minn Med. 1981; 64(4):401.
11. Colin F, Marin M, Stephen B, et al. Reversible blindness associated with alcoholic ketoacidosis: pseudomethanol intoxication. J Emerg Med. 1998; 16(4):597–599.

12. Kreshak AA, Clark RF. Transient vision loss in a patient with metformin associated lactic acidosis. Am J Emerg Med. 2010; 28(9):1059.e5–1059.e7.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download