This article has been
cited by other articles in ScienceCentral.
Dear Editor:
Herpes zoster (HZ) is caused by the reactivation of varicella zoster virus (VZV). Lowered VZV-specific cell-mediated immunity (CMI) causes the reactivation of VZV
1. The incidence of HZ is rapidly increasing worldwide, which may be caused by an aging population
2. The purpose of the study was to evaluate the annual incidence and seasonality of HZ in the general population in Korea.
Data of patients with HZ between January 2010 and December 2016 were collected from Health Insurance Review and Assessment Service (HIRA) database
3. Patients with at least one record of a diagnostic code (International Classification of Diseases-10, ICD-10) of B02.0 (zoster encephalitis), B02.1 (zoster encephalitis), B02.2 (Ramsay-Hunt syndrome), B02.3 (herpes zoster ophthalmicus), B02.7 (zoster with other complications), or B02.9 (herpes zoster) were included. Those who had a previous history of HZ were not excluded in this study. The study population was defined as the number of subscribers to the National Health Insurance Service (NHIS) during the study period. In addition, Google Trends data for ‘herpes zoster’ in Korean language were downloaded for further analysis of seasonality in HZ occurrence. The frequency of information-seeking behavior regarding the search term, ‘herpes zoster,’ ranged from 0 to 100. Available data from January 2012 to February 2018 were categorized into four seasons by calculating the average value in three-month periods; spring (March to May), summer (June to August), fall (September to November), and winter (December to February). This study was exempted for a review by the institutional review board of Seoul National University Bundang Hospital in accordance with the exemption criteria (IRB no. X-1407-257-902).
Of the total 4,232,576 HZ patients during the study period, 1,666,937 were male and 2,565,539 were female (male:female=0.65:1). The annual incidence of HZ steadily increased from 9.6 per 1,000 person-years (PY) in 2010 to 13.3 per 1,000 PY in 2016. While the number of medical insurance subscribers increased by 1,691,564 (3.3%) from 50,581,191 in 2010 to 52,272,755 in 2016, the number of HZ patients increased by 208,722 (43.0%) from 485,544 to 694,266. For those aged over 50 years, the number of HZ patients increased by 155,615 (57.7%) while the number of medical insurance subscribers increased by 3,875,179 (26.3%). Though the number of medical insurance subscribers aged under 50 years decreased by 2,183,615 (6.7%) during the study period, the number of HZ patients increased by 53,107 (24.6%).
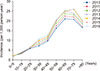
Fig. 1 demonstrates that the incidence of HZ steadily increased from 2010 to 2016 in all of the age groups. The age group of 70 to 79 years showed the most prominent increase in the incidence. The incidence of HZ increased with age, which was the highest in the age group of 60 to 69 years during the period of 2010 to 2014. In the period of 2015 to 2016, however, the peak incidence shifted to the age group of 70 to 79 years.
Fig. 2A shows the seasonality with respect to the incidence of HZ; it reached its peak in the summer season and lowest in the winter season. The number of patients in the spring, summer, fall, and winter seasons comprised of 24.0%, 27.2%, 25.8%, and 22.9%, respectively. Information-seeking behavior by analyzing Google search queries further revealed the seasonal pattern of HZ occurrence except in 2015 (
Fig. 2B).
A previous epidemiologic study analyzing the HIRA database for a 5-year period also demonstrated a steady increase in the annual incidence of HZ from 7.93 per 1,000 PY in 2003 to 12.54 per 1,000 PY in 2007
4. This value might be exaggerated since they included patients with postherpetic neuralgia. Nevertheless, the incidence results reported in Korea were considerably higher than that of other populations which were 4 to 6.24 per 1,000 PY
25. The higher incidence in Korea could be attributed to the medical service system, as it features mandatory enrollment of all citizens into NHIS with low medical cost burden and easy accessibility to medical services. Ethnic difference could also contribute to the higher incidence, although its genetic or environmental risk factor remains unknown.
Korean population is under a rapid aging, which is a wellknown risk factor for HZ. There have been several reports on the association between the rise in HZ incidence and age
2. This correlation is readily explained by the progressive decline in VZV-specific CMI with aging
1. However, an aging population solely could not explain the stead increase of the incidence of HZ in all of the age groups. Reduced chance of re-exposure to VZV is hypothesized to contribute to the lowered VZV-specific CMI in Korean population. Re-exposure to VZV might boost VZV-specific CMI to provide protection against HZ
6. Introduction of universal VZV vaccination in 2005 has dramatically lowered the number of varicella patients in Korea, which decreased from 140,359 in 2010 to 79,321 in 2016
3. A previous epidemiologic analysis revealed that the incidence of HZ was negatively associated with the incidence of varicella
5.
The relationship between seasonality and incidence of HZ has been controversial. In contrary to the analysis of 1-year HIRA data, our study investigating 7-year HIRA and Google Trend data clearly demonstrated the seasonality of HZ occurrence
7. A recent study clarified a strong association of the incidence of HZ with temperature and ultraviolet (UV) exposure
5. Sunny hours during the summer increase exposure to UV irradiation, inducing immune suppression and VZV reactivation from latency
8.
The limitation of this study is the absence of validation of the HZ diagnosis. A recent study revealed that the positive predictive value of HZ diagnosis based on ICD-10 was 86.2% by reviewing medical chart
9. Defining the HZ diagnosis as a presence of disease code for HZ with at least 5-day use of antiviral medication or acyclovir injection raised the positive predictive value to 99.5%. In addition, we could not exclude the patients who had a previous history of HZ in this study.
In conclusion, the annual incidence of HZ was increased not only in the total study population but also in all of the age groups from 2010 to 2016. The seasonality in the occurrence of HZ was demonstrated, which was the highest in summer.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download