IV. Discussion
Current anatomic studies on the location of the mandibular foramen have mostly been performed using dry mandibles
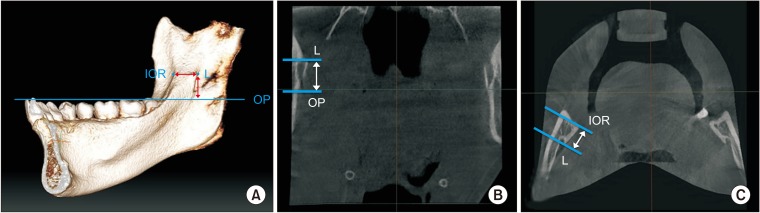
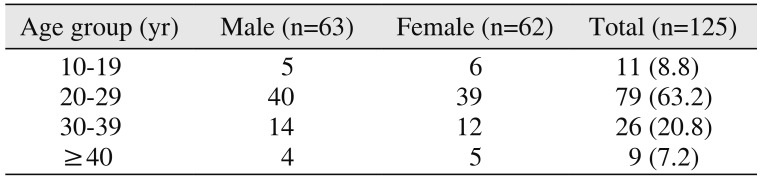
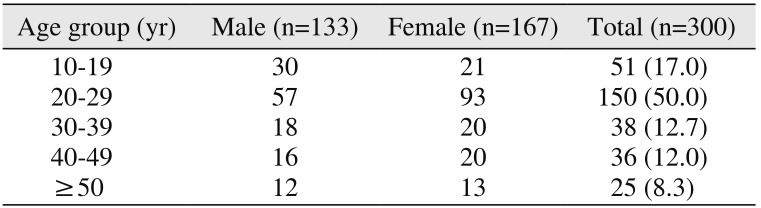
89101112131415. The results of these studies are relatively accurate because a dry mandible can be measured directly. However, information on dry mandibles regarding sex and age is limited, so comparison and analysis measuring the values is difficult. And a dry mandible, which has both intact dentition and an OP, is expensive and difficult to find. More recently, measuring a variety of anatomical measurements has become possible using computers. This is because software has been developed that can make 3D reconstructions and analyses using a patient's computed tomography (CT) images. These CT data are more convenient and inexpensive than those of a dry mandible. Also, researchers can set up various anatomic landmarks and make a virtual line in the software images. Thus, computer reconstruction allows for a complex measurement of the distance or the angle more easily than in a dry mandible studies. These data can be used in systematic and accurate analyses related to sex or age. In this study, a 3D mandibular model was made with the patient's CBCT images and then vertical and horizontal locations of the mandibular lingula were measured and analyzed.
Many authors have used different landmarks, such as the mandibular foramen or the lingula, to analyze the location of the IAN
89101112131415161718. The level of the mandibular lingula is a more useful landmark than the level of the mandibular foramen when a clinician determines the vertical target of the anesthetic needle in an IANB, because an IANB actually attempts to anesthetize the IAN around the mandibular lingula prior to it entering the mandibular foramen. Therefore, in this study, the location of the mandibular lingula was also measured as an anatomical landmark. Many results have been published about the antero-posterior location of the mandibular lingula or the mandibular foramen. According to Jansisyanont et al.
8 and Yu et al.
16, the lingula was positioned at 20.6 mm and 17.7 mm, respectively, from the anterior border of the ramus. Monnazzi et al.
9 noted a mean distance of 17.67 mm from the anterior border of the ramus to the mandibular foramen. Oguz and Bozkir
10 showed results with 16.9 mm on the right and 16.78 mm on the left. The distance from the IOR to the mandibular foramen was shorter than the distance from the anterior border of the ramus to the mandibular foramen
1112. Ennes and Medeiros
11 and Viravudth and Plakornkul
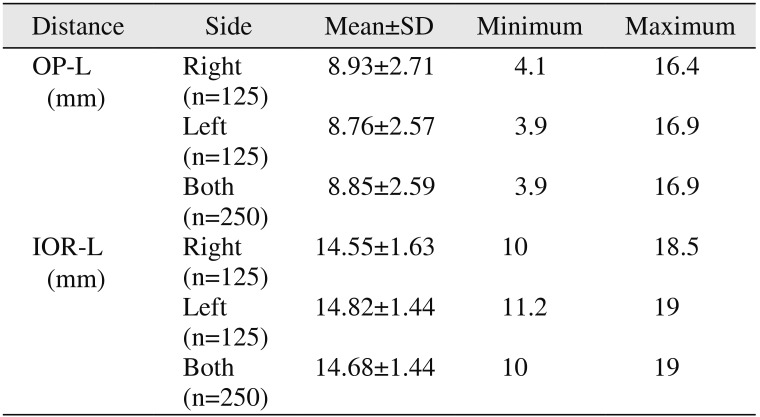
12 found 14.6 mm and 14.33 mm, respectively, as the mean distances from the IOR to the mandibular foramen. In this study, the mean distance from the IOR of the ramus to the lingula was 14.68±1.44 mm, and this distance is similar to the results of Ennes and Medeiros
11.(
Table 3)
To determine the horizontal insertion depth of the needle, the clinician should consider the thickness of the oral mucosa of the insertion point and the location of the IAN, which enters from the back of the lingula into the mandibular foramen. Many authors recommended an insertion depth of 20 to 25 mm to closely approach the mandibular foramen
1813. In this study, the insertion depth of the needle was determined to be 23 to 25 mm; this length was calculated by totaling the mean 14.68±1.44 mm of the IOR-L distance of this study, 4.7 mm of mandibular foramen width
8, and 4.12 mm of the mucosal thickness
19.
The mandibular foramen and the mandibular lingula vary in vertical location in each individual. Nicholson described that the mandibular foramen is located almost below the OP
14. However, Hwang et al.
17 and Kang et al.
18 stated that mandibular foramina are located 4.16 mm and 3.8 mm, respectively, above the OP in adults. Jansisyanont et al.8 reported that the lingula is located 4.5 mm above the OP. In this study, the mean OP-L vertical distance was measured to be 8.85±2.59 mm from the OP to the mandibular lingula.(
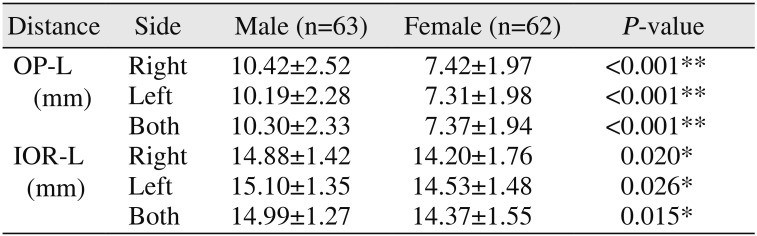
Table 3) The OP-L vertical distance has more individual variation than the IOR-L horizontal distance, and both the OP-L vertical distance and the IOR-L horizontal distance in males were relatively longer than those in females.(
Table 4) In many studies, the insertion level of the needle was recommended to be set at 8 to 10 mm above the OP
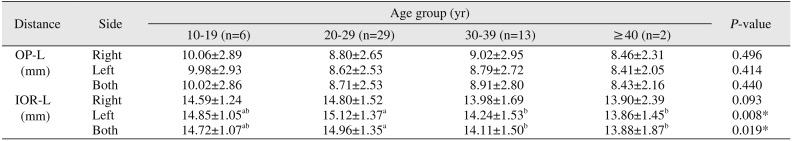
11315. If the insertion level of the needle is adjusted vertically from 8.85±2.59 mm of the mean OP-L vertical distance, taking into consideration the patient's information, such as sex, age, and panorama radiography, the success rate of the anesthesia increases.
Infiltration anesthesia is very effective in the maxilla without block anesthesia because the maxilla has a larger volume of cancellous bone. However, block anesthesia is needed for restorative and surgical procedures of a mandibular molar because the mandible is surrounded by thick compact bone, and the infiltration of the anesthetic solution is limited. Since Halstead introduced the first block anesthesia, many authors have described various techniques for the IANB
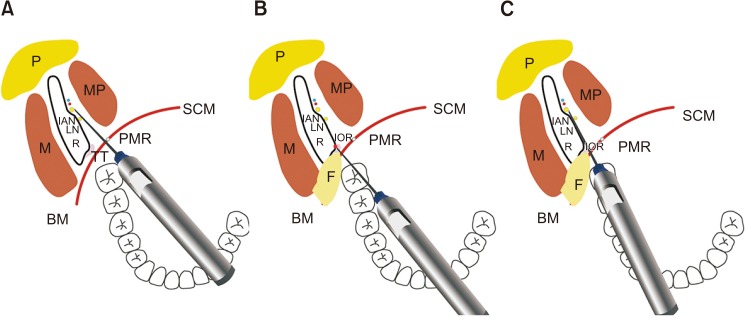
20. Among them, the conventional IANB has commonly been used to achieve IAN anesthesia. The needle is inserted parallel to the OP and from the premolars on the contralateral side. The insertion point is determined at the soft tissue lateral to the pterygomandibular raphe and above 8 to 10 mm from the OP. The needle is inserted through the mucosa and approaches near the mandibular foramen of the inner ramus and then the anesthetic solution is given after aspiration. In the IANB, the anesthetic solution should be injected near the IAN located inside the pterygomandibular space. Thus, the clinician should consider both the anatomy of the IAN and the pterygomandibular space. The boundaries of each pterygomandibular space are the medial pterygoid muscle medially, the ascending ramus of the mandible laterally, the lateral pterygoid muscle superiorly, the posterior border of the buccal space anteriorly, and the parotid gland posteriorly. The pterygomandibular space contains the IAN, the lingual nerve, the inferior alveolar vessel, and the sphenomandibular ligament. The IAN passes along the pterygomandibular space through a narrow space between the medial pterygoid muscle and the lateral pterygoid muscle; it enters into the mandibular foramen and is distributed widely throughout the mandible. The lingual nerve passes more antero-medially than the IAN in the pterygomandibular space. The lingual nerve is commonly blocked together with the IAN by an IANB.
The success rate of an IANB depends greatly on the skill and experience of clinician. It has a relatively high failure rate (15%–35%)
123. Also, clinical studies in endodontics have found a high failure rate (38%–75%) with the IANB. This is related to the inflammatory condition of the pulp
4567. Many authors have described that a variable location of the mandibular foramen raises the failure rate of an IANB
21222324. For the success of an IANB, the needle should approach as close as possible to the IAN or the mandibular foramen on the pterygomandibular space.
Many alternative techniques for the IANB have been described to achieve satisfactory success and reduce complications
25262728293031. Thangavelu et al.
25 introduced an alternative technique with a high success rate of 95%. In this technique, the first insertion point is 6 to 8 mm above the coronoid notch and 8 to 10 mm posterior from the anterior border of the ramus, and then the barrel of the syringe is adjusted toward the midline and the mandibular foramen approaches along the medial side of the ramus. This technique has a different needle insertion point than the IOR-guided technique, but both techniques are similar in needle movement along the inner periosteum of the ramus. Chakranarayan and Mukherjee
26 introduced the arched needle technique for the IANB where, after insertion, the needle is arched and inserted in a manner whereby it approaches the medial surface of the ramus at an angle almost perpendicular to it. A success rate of 98% was obtained, but this technique has the potential for needle breakage and damage to the soft tissue. Boonsiriseth et al.
27 introduced a novel injection approach in which the barrel of the syringe is placed on the occlusal surface of the posterior teeth at the same operation site. The needle insertion point is the same point as for the conventional IANB. This technique has the advantage of eliminating pain from the needle traumatizing the periosteum and bone. Suazo Galdames et al.
28 introduced an alternative technique whereby the anesthetic is applied to the IAN via the retromolar triangle. According to their study, the needle is presented between the mandibular canal and variable holes of the retromolar triangle, through which the infiltration of an anesthetic solution would be possible. Even though this technique has a high failure rate of 27.5%, it can be used to minimize the complications for patients with blood dyscrasias. Takasugi et al.
29 introduced an anterior technique in which the needle is inserted to a depth of 10 mm, and the anesthetic solution is injected into the anterior region of the pterygomandibular space. This technique was developed so that anesthesia can be delivered to the IAN with a lower risk of inferior alveolar neural and vascular complications; however, the success rate of this technique is relatively low (75%). The Gow-Gates technique
30 and Akinosi technique
31 block the mandibular nerve trunk directly in the more upper position than the conventional IANB. Despite the fact that both techniques are very useful in some patients when the clinician cannot use the conventional IANB, most clinicians do not often use either technique because separate skillsets are required and the anesthetic latency is too late.
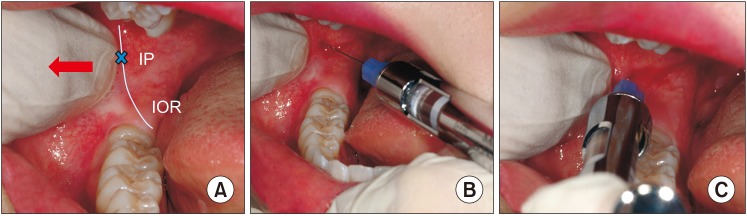
In conventional IANB, many clinicians have difficulty determining the insertion point and depth of the needle. This is due to the mobilization of the soft tissue during needle insertion and because penetration is through multiple layers of anatomic structure. For a successful IANB, a definite point of reference is required at the needle insertion. Alternative IANBs using the IOR as the reference point were performed in this study. After detection of the IOR, located 8 to 10 mm above the OP, the needle is inserted to a 23 to 25 mm depth along the medial periosteum of the ramus; then, the anesthetic is injected around the mandibular lingula. In this alternative technique, the clinicians can more easily determine the injection point with a rigid and stable IOR. The needle can reach near to the mandibular lingula without resistance, and damage to the soft tissue can be prevented because the needle moves along the medial periosteum of the ramus.
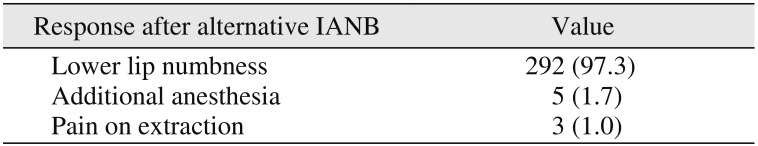
When we performed the IANB using the IOR in this study, anesthetic failure occurred in only eight patients (2.7%).(
Table 6) This is a lower failure rate than experienced using other IANB techniques. The causes of failure was not clear, but some possibilities are assumed. The needle and the anesthetic solution could not approach around the mandibular foramen because of a severe anatomical variation in the mandibular foramen or an accessory branch of the IAN
1421222324. If the needle is inserted into a malposition instead of the IAN around the mandibular foramen, various complications can occur, such as damage to the soft tissue, swelling, pain, and trismus
3233. The needle may fracture if the clinician applies excessive force
34. If the needle is positioned too posteriorly, the anesthetic may be diffused into the parotid gland, which may cause transient paralysis of the facial nerve
35. If the needle is positioned too high and deep, the auriculotemporal nerve can be anesthetized, and numbness around the ear can occur. Especially if the anesthetic solution is injected into the lateral pterygomandibular muscle, pain, trismus, and disorders of the temporomandibular joint can be induced. If the pterygomandibular vessel or the pterygoid venous plexus is damaged by needle insertion, a hematoma can occur in the pterygomandibular space
21. Most complications can be resolved in a short time, but any unexpected complication may affect the relationship between the patient and the clinician if it occurs after anesthesia. In this study, complications did not occur because a clear reference, such as the IOR, was used in the needle insertion, and the anesthetic solution was injected taking into consideration the mean location of the mandibular lingula.
In this study, all analyses were carried out using only hard tissue associated with the location of the mandibular lingula. To increase the success rate of an IANB, soft tissue also needs to be considered. Additional studies regarding the thickness of oral mucosa, where the needle is inserted, and the size of the pterygomandibular space where the anesthetic is injected, are necessary. In addition, the OP can change according to malocclusion, prosthetics, sex, or age, which can lead to measurement errors or anesthesia failure. Additional studies of these variables are needed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download