Abstract
The femoral nerve is the largest branch of the lumbar plexus. It is normally composed of the ventral rami of spinal nerves L2 to L4. The psoas major has proximal attachments onto the T12 to L5 vertebrae and related intervertebral discs, fuses with the iliacus deep to the inguinal ligament and then attaches onto the lesser trochanter of the femur. Normally, the anatomical relationship is that the femoral nerve is located between the iliacus and psoas major. Herein, we report a case of the psoas quartus muscle related to several splits of the femoral nerve within the pelvis. Although the embryology for this is unclear, surgeons and physicians should be aware of such anatomical variants in order to better understand pain and entrapment syndromes and during surgical maneuvers in this region such as lateral transpsoas approaches to the lumbar spine.
The psoas major and the iliacus form the iliopsoas muscle which flexes the hip joint. The proximal attachment of the psoas major ranges from the T12 to L5 vertebrae and the related intervertebral discs. The psoas major muscle passes under the inguinal ligament with the iliacus and attaches onto the lesser trochanter of the femur. The femoral nerve (FN) consists of the posterior divisions of the ventral rami of L2–4. Occasionally, the ventral rami of L1 and/or L5 contributes to the formation of the FN. The FN runs inferolaterally between the psoas major and iliacus to pass deep to the inguinal ligament [1]. The FN and its terminal branches traveled to the anterior and medial thigh and medial leg.
Some have studied the variants of the psoas muscles. Clarkson and Rainy [2] classified the psoas muscles into four types: psoas magnus, psoas parvus, psoas tertius, and psoas quartus. Jelev et al. [3] reported a variant psoas muscle as the “accessory psoas major.” These variant psoas muscles occasionally split the FN. Herein, we present a case of a multiply splite FN with a psoas quartus muscle.
During the routine dissection of the posterior abdominal wall of a fresh-frozen female Caucasian cadaver whose age at death was 71 years old, a variant muscle on the left side was observed to split the FN into multiple parts (Fig. 1). This muscle originated from the anteromedial surface of the quadratus lumborum and ran distally to fuse with the tendon of the psoas major at the level of the inguinal ligament. The FN on this side was formed by the ventral rami of the L2 to L4 at the level of L4 and bifurcated into four separate branches at the level of L5. The most medial branch descended posterior to the psoas quartus muscle and innervated the iliacus. The second and third branches were split by the variant muscle over 101.9 mm, reunited laterally to the variant muscle and then passed below the inguinal ligament. The most lateral branch ran downward and anterior to the variant muscle, independently passed beneath the inguinal ligament without reunion, and innervated the skin on the lateral aspect of the thigh together with the lateral femoral cutaneous nerve. The FN had direct branches that supplied the iliacus, psoas major, and psoas quartus muscles. No other musculoskeletal variants were observed in the area dissected and no signs of previous surgical intervention were found.
Anatomical variants of the iliopsoas muscle have been described [2345]. Clarkson and Rainy [2] reported a rare case with four psoas muscles: the psoas major and minor and psoas tertius and quartus. The origin of the psoas tertius is from the medial half of the twelfth rib, the distal ends of the transverse processes of the L1 to L4 vertebrae, and closely related to the insertion of the quadratus lumborum. The psoas quartus originates from the anteromedial surface of the quadratus lumborum and also from the transverse process of the L5 vertebra. These two muscles fuse with the tendons of the psoas major at the level of the inguinal ligament. Tubbs et al. [5] reported a variant of the psoas quartus where it arose from the transverse process of the third lumbar vertebra and the anteromedial aspect of the quadratus lumborum. Recently, Khalid et al. [4] reported a case of the psoas tertius piercing the FN. An “accessory psoas major muscle” [3] that is fusiform shaped and arose from the third lumbar and intertransverse ligament between the third and fourth lumbar vertebrae has been described. Based on the findings in the present case, the variant muscle was defined as the psoas quartus [2].
The FN can be split by variant muscles as described above. Vazquez et al. [6] found that 19 out of 242 specimens had a muscle slip from the iliacus and psoas major piercing the FN. In those 19 specimens, four specimens had a psoas major muscular slip piercing the FN; twelve specimens had an iliacus muscular slip piercing the FN; and two specimens had a muscular slip covering the FN. The authors concluded that these FN variations have no significant relationship with sex or side. Kirchmair et al. [7] found that the FN had two ramifications in nine out of 61 specimens, three ramifications in four out of 61 specimens, and there was no record of four ramifications. In 11 out of 13 specimens, reunification of each branch was observed proximal to the inguinal ligament, and two out of 13 cases had no reunification before exiting the pelvis. Anloague and Huijbregts [8] studied 34 lumbar plexuses in detail and revealed that 35.3% of the FN were split into two or three parts by slips of the psoas major.
Variations of the FN and psoas muscles might affect surgical approaches to the region such as lateral transpsoas interbody fusion procedures, lumbar plexus blockade, femoral artery manipulation for angiography or other pelvic region procedures [791011]. Minimal knowledge of such anatomical variations can result in FN compression or damage as well as iliacus compartment syndrome due to, for example, hematoma of the surrounding muscles [512]. In the present case, the split FN could be compressed by such a muscle variant. A knowledge of these anatomical variants might also explain pain in the hip and thigh and incomplete blockade of the FN [13].
There are many possible explanations for variation described here. For example, variations in the timing of motor and sensory axons growth, cell signaling, and muscle apoptosis could all play a role. During week four after fertilization, spinal nerves extend out to myotomes and develop associations with them. At week five, the myotomes will separate into two divisions, epimeres and hypomeres. Hypomers extend into the elongating limbs. During this elongation, muscles will bring associated nerves from the torso into the limb buds. Since motor axons develop and enter into the limb first, sensory axons enter into the limb later based on the path of the motor axons. Therefore, there is a chance for muscle slips to grow over the motor axons and for sensory axons to try to grow around the muscle slips. As a result, in our case, the FN could be divided into several parts. Additionally, the additional attachments of the psoas muscle may have originated from differences in cell signaling during development of the thoracic and lumbar myotomes, or a mutation of PAX3 and migratory peptide growth factor [14]. It is also possible that this additional muscle slip did not go through apoptosis at the end of development [14], or additional muscle slips might have failed to establish during development.
Figures and Tables
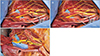 | Fig. 1(A) Photograph of the left anterior view of the case presented herein. The psoas quartus (asterisk) and split femoral nerve is shown. (B) The psoas quartus is outlined by the white dotted line. (C) After cutting and reflecting the psoas quartus (asterisks and white solid lines) and the psoas major (red solid lines) the following structures are shown. CIA, common iliac artery; I, iliacus; PM, psoas major; QL, quadratus lumborum; 1, the most medial branch of the FN; 2, the second branch of the FN; 3, the third branch of the FN; 4, the most lateral branch. |
References
1. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 41st ed. New York: Elsevier;2016. p. 1094–1095.
2. Clarkson RD, Rainy H. Unusual arrangement of the psoas muscle. J Anat Physiol. 1889; 23(Pt 3):504–506.
3. Jelev L, Shivarov V, Surchev L. Bilateral variations of the psoas major and the iliacus muscles and presence of an undescribed variant muscle: accessory iliopsoas muscle. Ann Anat. 2005; 187:281–286.
4. Khalid S, Iwanaga J, Loukas M, Tubbs RS. Split femoral nerve due to psoas tertius muscle: a review with other cases of variant muscles traversing the femoral nerve. Cureus. 2017; 9:e1555.

6. Vazquez MT, Murillo J, Maranillo E, Parkin IG, Sanudo J. Femoral nerve entrapment: a new insight. Clin Anat. 2007; 20:175–179.
7. Kirchmair L, Lirk P, Colvin J, Mitterschiffthaler G, Moriggl B. Lumbar plexus and psoas major muscle: not always as expected. Reg Anesth Pain Med. 2008; 33:109–114.

8. Anloague PA, Huijbregts P. Anatomical variations of the lumbar plexus: a descriptive anatomy study with proposed clinical implications. J Man Manip Ther. 2009; 17:e107–e114.

9. Perry CP. Peripheral neuropathies and pelvic pain: diagnosis and management. Clin Obstet Gynecol. 2003; 46:789–796.

10. Tubbs RS, Salter EG, Wellons JC 3rd, Blount JP, Oakes WJ. Anatomical landmarks for the lumbar plexus on the posterior abdominal wall. J Neurosurg Spine. 2005; 2:335–338.

11. Mahan MA, Sanders LE, Guan J, Dailey AT, Taylor W, Morton DA. Anatomy of psoas muscle innervation: cadaveric study. Clin Anat. 2017; 30:479–486.

12. Aichroth P, Rowe-Jones DC. Iliacus compartment compression syndrome. Br J Surg. 1971; 58:833–834.

13. Spratt JD, Logan BM, Abrahams PH. Variant slips of psoas and iliacus muscles, with splitting of the femoral nerve. Clin Anat. 1996; 9:401–404.

14. Moore KL, Persaud TV, Torchia MG. The developing human. 10th ed. Philadelphia: Elsevier;2016. p. 357–358. p. 367




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download