Abstract
Spinal stenosis most commonly occurs on lumbar vertebrae because of degenerative changes. This research studied the characteristics of osteophyte development in lumbar vertebrae foramina and association of osteophyte development with lumbar spinal stenosis. The total number of all levels of lumbar spines of subjects was 179 from 31 to 90 years of age. The vertebral foramen was divided into six zones. The prevalence and measurements of the length of osteophytes in the vertebral foramina were obtained. The prevalence and length of osteophytes in the posterior body zone were higher than the laminal zone, and higher than the pedicular zone, respectively. In each zone, the highest prevalence of osteophytes was at L5, except for the inferior posterior body zone that the highest prevalence is at L4. The length of osteophyte was also in same direction as the prevalence. The prevalence of osteophytes among six zones of each level were compared, and found, in L1 to L4, the inferior posterior body zone generally had the highest prevalence, except in L5, the superior posterior body zone had the highest prevalence. Moreover, prevalence, as well as length, of osteophytes in lumbar vertebral foramina, of all levels, was positively associated with age. Vertebral osteophytes can develop beginning at 31 years of age. In conclusion, posterior body of L4 and L5 had the highest prevalence of osteophyte formation, thus, these area had the highest probability to cause spinal stenosis.
Presently, the number of the elderly in Thailand is increasing with many of them suffering from low back pain. One of the causes is vertebral osteophyte formation [1]. The lumbar spine has the highest prevalence of vertebral osteophytes [2]. In some cases, osteophytes on the lumbar spine can cause severe effects, on the abdominal aorta or inferior vena cava [3]. If severe, osteophytes can be a life-threatening condition that requires surgery [9].
Spinal osteophyte is one of the conditions that can pathologically cause low back pain and other abnormal spinal disorders [4]. Some factors, leading to osteophyte formation, are age, gender and physical activities. The prevalence of osteophytes in all positions of the spine increases significantly with age [5]. Occupation, heavy physical activities and movements can also contribute to potential osteophyte formation [6]. Many studies showed that movements in a bowed position with torso tilted to the side and lifting an object had the most impact on the vertebral discs and vertebrae, especially in L4 and L5, which could increase the risk of osteophyte development. Moreover, vertebral osteophytes are found on L4 and L5 in the largest number [78].
Spinal stenosis can be affected by osteophyte formation, which can have narrowed vertebral foramina centrally and laterally. From the findings, L3 has the smallest developmental spinal canal cross-sectional area and depth, but cranially and caudally enlarging [9]. The spinal canal cross-sectional area does not change with age, weight, or body mass index [9]. Spinal stenosis most commonly occurs on lumbar vertebrae because of degenerative changes, which predominate at the L3, L4, and L5, in older ages [10]. The data collected from Northeast Thais shows that the prevalence is highest in L3, L4, and L5. The prevalence of osteophyte in lumbar vertebral foramen is 0% in age less than 51, 2.9% in age of 51–60, 9.6% in age of 61–70, and 4.5% in age over 70 [2]. Since, osteophytosis is one of the conditions that is linked to spinal stenosis, our research study explored the characteristics of lumbar osteophyte formation related to age in vertebral foramina.
Although lumbar foraminal osteophyte had been studied previously, the study did not provide much detail, or relationship to clinical application. Thus, we are interested in studying the changing of osteophytes on lumbar vertebral foramina. This research would provide information about the characteristics of osteophyte development in lumbar vertebral foramina in a Thai population. In addition, the basic information leading to an anticipation of spinal stenosis could be obtained.
The samples were selected from donated skeletons from the Center for Forensic Science, Faculty of Medicine, Chiang Mai University. We selected all levels of lumbar spines of dry skeletal bone from 31 to 90 years of age with conditions which had no foraminal damage and no pathological diseases of the spine, such as ankylosing spondylitis. The samples were stratified into six groups, age of 31 to 40, age of 41 to 50, age of 51 to 60, age of 61 to 70, age of 71 to 80, and age of 81 to 90. We calculated sample size of each group by using Cochran's formula (z=1.96, e=0.1). The total number of sample size was 179 which included the following age of 31 to 40 is 15, age of 41 to 50 is 26, age of 51 to 60 is 35, age of 61 to 70 is 35, age of 71 to 80 is 34, and age of 81 to 90 is 34.
We classified the lumbar spine into three zones, laminar zone (zone 1), pedicle zone (zone 2), and posterior body (zone 3) related with foraminal area. For the laminar and pedicle zones, each zone was divided into left and right part. For posterior body zone, it is divided into superior and inferior part. We observed each level of the lumbar spine to find osteophyte development. Then, we measured the longest osteophyte that invaded the foramen of each zone by using digital Vernier caliper.
After we collected data, we used the SPSS version 22 (IBM Corp., Armonk, NY, USA) to analyze the data. The prevalence of each levels, and each zones of all levels were calculated. Descriptive statistics were performed to compare; first, the prevalence of each level in each age group. Second, the prevalence of each zone in each age group. Third, the prevalence and length of each zone in each level of the lumbar spine. The test using for independence of the prevalence of osteophyte in each zone and each level, and age was chi-square test, or Fisher's exact test. Significance tests with P-value of 0.05 or less, were considered statistically significant. The correlation of the length of osteophyte and age was determined by the Spearman test (one-tailed significance tests with P-value of 0.05 or less). The test using for independence of the prevalence of osteophyte in each zone and each level, and sex was chi-square test, or Fisher exact test. Significance tests with P-value of 0.05 or less, were considered statistically significant.
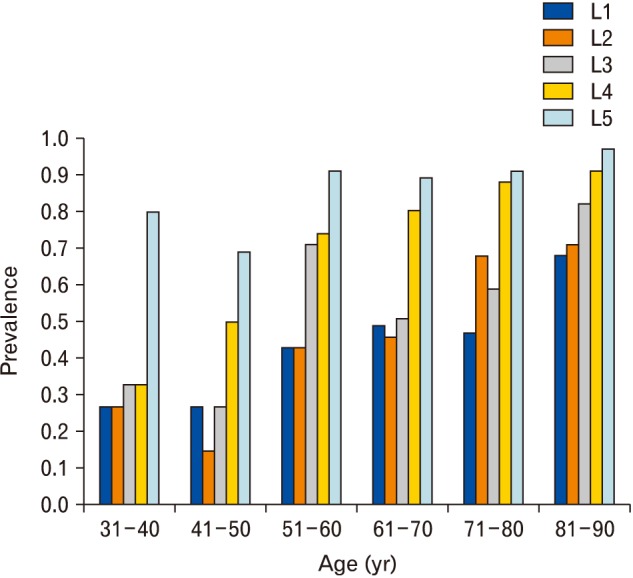
For the overall prevalence of osteophytes in the lumbar vertebral foramina, the study found that population aged over 31 years old could have a risk to develop osteophytes. The lumbar level that had the highest prevalence of osteophytes was at L5 (Fig. 1). Moreover, the prevalence of osteophytes in lumbar vertebral foramina, of all levels, was positively associated with age (Table 1).
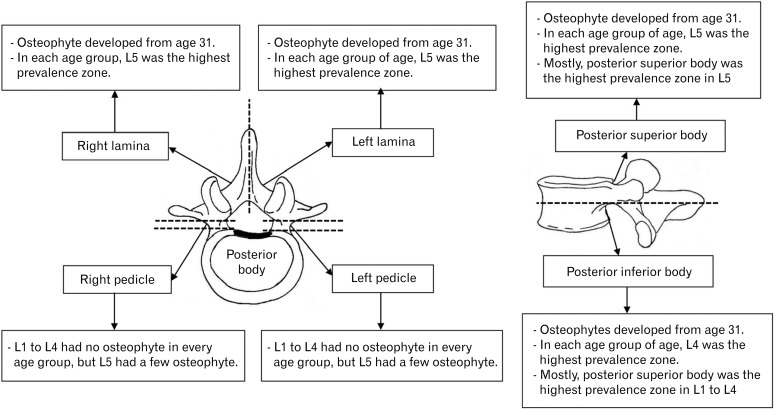
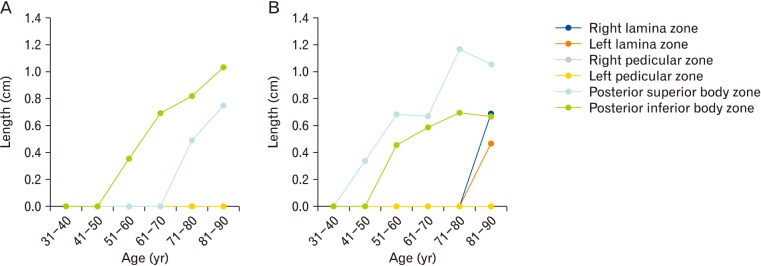
If lumbar vertebral foramina were divided into six zones, as previously mentioned. As in Fig. 2, we found that osteophytes could be developed in the right and left laminal zone in population aged over 31 years old. Similarly, in the superior and inferior posterior body zone, generally, osteophytes could also be developed in the population aged over 31 years old. In the left and right pedicular zone, the study found no osteophyte development in L1–L4, and very few in L5. Thus, osteophyte formation mainly occurred in the laminal and posterior body zone, but rarely in the laminal zone (Fig. 3). When comparing the prevalence of osteophytes in each zone, we concluded that the prevalence of osteophytes in the posterior body zone were higher than laminal zone, and higher than the pedicular zone, respectively. In each zone, we found that the highest prevalence was at L5, except the posterior inferior body zone where the highest prevalence was at L4. The highest prevalence of osteophytes was at the inferior posterior body of L4 of age 81 to 90 and superior posterior body of L5 of age 81 to 90 (prevalence=0.88). In case of the length of osteophyte in each zone, compared by median (Fig. 4). The length of osteophyte in the posterior body zone was higher than the laminal zone, and higher than the pedicular zone, respectively. Generally, the longest osteophyte was at L5 in each zone, except the posterior inferior body zone where the longest was at L4. Thus, the result of prevalence and length in our study are in the same direction.
When we compared the prevalence of osteophytes among six zones of each level, we found that, in L1 to L4, inferior posterior body zone generally had the highest prevalence, except in L5, superior posterior body zone had the highest prevalence. These prevalence data were obviously distinguishable at age over 51 years old. In age 31–50 years old, the prevalence of osteophytes in the laminal and posterior body zone were indistinguishable (Fig. 2).
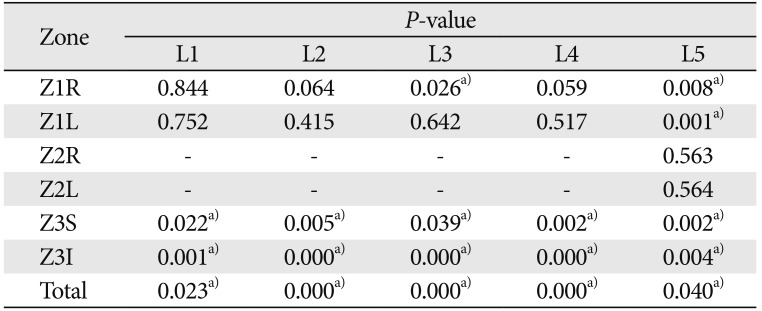
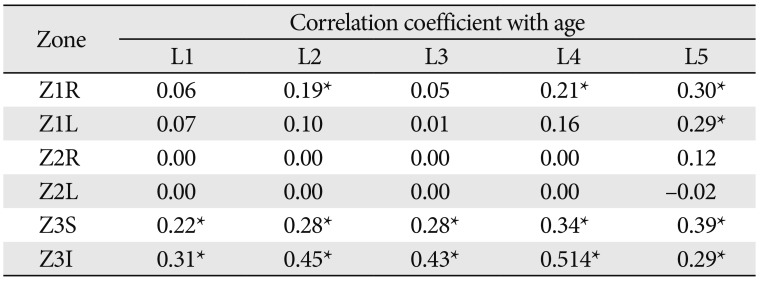
The association between prevalence and age was calculated by chi-square. The study found that, only the superior and inferior posterior body zone were significantly associated with age in L1 to L4. For L5, the right laminal zone, left laminal zone, superior and inferior posterior body zone were significantly associated with age (Table 1).
The relationships between the length of osteophyte and age were calculated by Spearman test. The study found that, only the superior and inferior posterior body zone were positively significantly associated with age in every lumbar vertebral level. In addition, right laminal zone, and left laminal zone in L4 and L5 were also positively significantly associated with age (Table 2).
The lumbar spine is a main supportive structure of body weight. It is regularly forced by compression, shear, torsion and bending [11]. Excessive motion, especially bending and torsion, causes cumulative trauma on the spine, leading to production of proinflammatory cytokines [11]. These proinflammatory cytokines can lead to osteophyte formation [12]. Thus, we can find osteophytes in lumbar vertebral foramina of dry bone over 31 years old in the study. The cumulative trauma increased with age, so, the prevalence of osteophytes also increased. Compressive force, equal to spinal loading, on vertebral body is increased when bending forward or lifting weight because of increased muscle tension [11]. The major forces were flexion and compression, that affected mainly the disc, vertebral body, and endplate [13]. The neural arch was affected mostly by shearing force, but also, extension and torsion [13]. Therefore, as our result, the prevalence of osteophytes of the posterior body was higher than the prevalence of osteophytes of the lamina and facet joints. The pedicle is a structure that helps in transmitting force between the posterior portion (transverse process, articular process, lamina, and spinous process) and vertebral body [13]. In addition, the pedicle has neither origin nor insertion of muscle and ligaments. In our study, osteophyte formation on the pedicle was rare Therefore, the prevalence of osteophytes at the posterior body was higher than the lamina, higher than the pedicle, respectively. Range of motion of lumbar flexion in vivo between L4 and L5 was highest [13]. Bending moment was exponentially increased with lumbar flexion angle [11]. This implied that the compression is also highest between L4 and L5. We found that the highest prevalence of osteophyte formation was at the inferior posterior body of L4, and superior posterior body of L5.
As discussed previously, the main forces were flexion and compression, that acted mainly on the disc, vertebral body and endplate. Thus, the length of osteophytes at the posterior body was higher than the lamina, and higher than the pedicle, respectively. In addition, the compression was highest between L4 and L5, so the highest length of osteophyte was at the inferior posterior body of L4, and superior posterior body of L5.
Because of the highest force loading on each lumbar vertebral body, the posterior body had the highest cumulative force. This made the prevalence and length of posterior body positively related to age, significantly. Spinal stenosis could be classified into three types as central, lateral recess, and foraminal stenosis [13]. Our study focused on central spinal stenosis, which occurred by a degenerative process. One of the causes of central spinal stenosis is osteophyte formation which is involved in the vertebral foramina [14]. Osteophytes that, originated from the posterior body, pedicle and lamina, can protrude into the vertebral foramen and lead to spinal canal narrowing. We suspect that the osteophytes at the posterior body had the highest chance to cause osteophyte relatedcentral spinal stenosis. We also suspected that the osteophyte at the posterior body had the highest chance to cause osteophyte related-central spinal stenosis because, from our study, the length of osteophyte at posterior body was the longest and had the highest prevalence. Moreover, enlargement of the facet joint and ligamentum flavum hypertrophy could narrow the spinal canal, leading to central spinal stenosis [13]. In order to decrease risk of osteophyte development and other spinal injuries, avoiding stooping to lift heavy weight and unsupported erect sitting should be considered in daily life, especially the elderly [11].
The comparison between our study results and the previous research, collected data from Northeast Thais, in 2008 [2], we found that the prevalence of lumbar vertebral foraminal osteophyte of all levels from our study is higher in every age group. Moreover, the studies had the same conclusion that prevalence of foraminal osteophyte is associated with age. In addition, the study in 2012 by Kim et al. [15] found that osteophytosis on L4 and L5 were apparently more severe than those on other lumbar vertebrae. Although the study did not focus on vertebral foraminal osteophyte, the result was in the same way as our study that L4 and L5 had the most severe osteophyte development.
The limitations of this study were, firstly, the result can only be applied in Thai population. Secondly, the dry skeletons in Medical Faculty, Chiang Mai University were insufficient for our sample size.
In the study, posterior body of L4 and L5 had the highest prevalence of osteophyte formation, thus, these areas had the highest probability to cause spinal stenosis. However, the information regarding spinal stenosis associated with foraminal osteophytes was not obvious. This might imply that foraminal osteophyte formation was less likely to cause spinal stenosis. Imaging studies could be performed for more evidence.
Acknowledgements
The authors are very grateful to Forensic Osteology Research Center and Department of Anatomy, Chiang Mai University. The authors also thank research funding received from Faculty of Medicine, Chiang Mai University.
References
1. Lamer TJ. Lumbar spine pain originating from vertebral osteophytes. Reg Anesth Pain Med. 1999; 24:347–351. PMID: 10445775.
2. Namking M, Buranaurgsa M, Jeeravipoolvarn P, Deesart M. The prevalence of vertebral osteophyte formation in Northeast Thais. Srinagarind Med J. 2008; 23:81–92.
3. Klaassen Z, Tubbs RS, Apaydin N, Hage R, Jordan R, Loukas M. Vertebral spinal osteophytes. Anat Sci Int. 2011; 86:1–9. PMID: 20383671.
4. Goode AP, Carey TS, Jordan JM. Low back pain and lumbar spine osteoarthritis: how are they related? Curr Rheumatol Rep. 2013; 15:305. PMID: 23307577.
5. Zukowski LA, Falsetti AB, Tillman MD. The influence of sex, age and BMI on the degeneration of the lumbar spine. J Anat. 2012; 220:57–66. PMID: 22050626.
6. O'Neill TW, McCloskey EV, Kanis JA, Bhalla AK, Reeve J, Reid DM, Todd C, Woolf AD, Silman AJ. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999; 26:842–848. PMID: 10229405.
7. Chanapa P. Relationship between Thai working lifestyles and lumbar osteophyte. Songkla Med J. 2016; 34:201–209.
8. Chanapa P, Yoshiyuki T, Mahakkanukrauh P. Distribution and length of osteophytes in the lumbar vertebrae and risk of rupture of abdominal aortic aneurysms: a study of dry bones from Chiang Mai, Thailand. Anat Cell Biol. 2014; 47:157–161. PMID: 25276474.
9. Griffith JF, Huang J, Law SW, Xiao F, Leung JC, Wang D, Shi L. Population reference range for developmental lumbar spinal canal size. Quant Imaging Med Surg. 2016; 6:671–679. PMID: 28090445.
10. Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010; 24:253–265. PMID: 20227646.
11. Adams MA, Bogduk N, Burton K, Dolan P. The biomechanics of back pain. Edinburgh: Elsevier Science;2002.
12. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskelet Dis. 2013; 5:77–94. PMID: 23641259.
13. Williams SK. Thoracic and lumbar spinal injuries. In : Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderston RA, editors. Rothman-Simeone the Spine. 6th ed. Philadelphia, PA: Elsevier Saunders;2011. p. 1132–1156.
14. Boos N, Aebi M. Spinal disorders: fundamentals of diagnosis and treatment. Berlin: Springer;2008.
15. Kim DK, Kim MJ, Kim YS, Oh CS, Shin DH. Vertebral osteophyte of pre-modern Korean skeletons from Joseon tombs. Anat Cell Biol. 2012; 45:274–281. PMID: 23301195.
Fig. 2
The prevalence of vertebral foraminal osteophyte on each lumbar level (A, L1; B, L2; C, L3; D, L4; E, L5) in each zone.
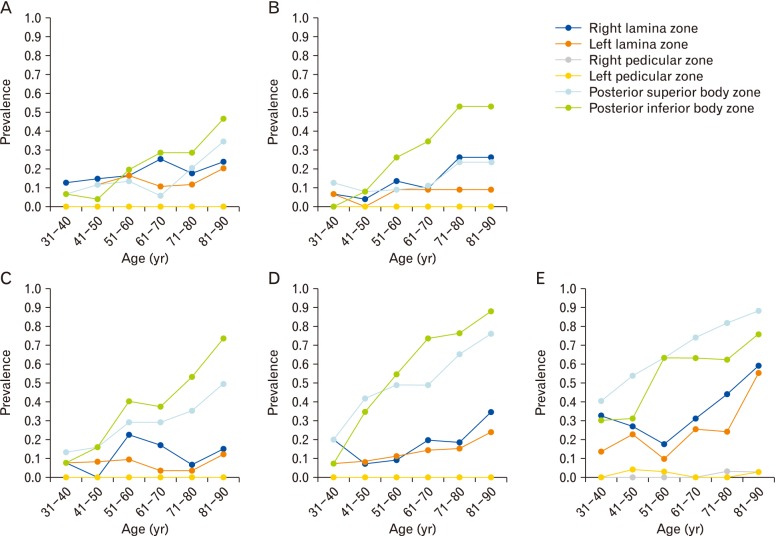
Table 1
Relationship between osteophyte prevalence and age




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download