1. Weyand CM, Goronzy JJ. Giant-cell arteritis and polymyalgia rheumatica. Ann Intern Med. 2003; 139:505–515. PMID:
13679329.

2. Rahman W, Rahman FZ. Giant cell (temporal) arteritis: an overview and update. Surv Ophthalmol. 2005; 50:415–428. PMID:
16139037.

3. Hayreh SS, Podhajsky PA, Zimmerman B. Occult giant cell arteritis: ocular manifestations. Am J Ophthalmol. 1998; 125:521–526. PMID:
9559738.

4. Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009; 28:34–62. PMID:
19063989.

5. Pereira LS, Yoon MK, Hwang TN, Hong JE, Ray K, Porco T, et al. Giant cell arteritis in Asians: a comparative study. Br J Ophthalmol. 2011; 95:214–216. PMID:
20584707.

6. Kobayashi S, Yano T, Inaba Y, Hashimoto H, Matsumoto Y, Tamakoshi A, et al. Ocular involvements of Japanese patients with giant cell arteritis from the first nation-wide survey. Arthritis Rheum. 2003; 49:867–868. PMID:
14673978.

7. Cha DM, Lee T, Choe G, Yang HK, Hwang JM. Silent giant cell arteritis in an elderly Korean woman. Korean J Ophthalmol. 2013; 27:224–227. PMID:
23730119.

8. Kang YS, Park SW, Lee HK, Choi YD, Heo H. Arteritic anterior ischemic optic neuropathy associated with giant cell arteritis in an elderly Korean man. Korean J Ophthalmol. 2016; 30:239–241. PMID:
27247526.

9. Yoon HJ, Park SW, Lee HK, Choi YD, Heo H. Bilateral arteritic anterior ischemic optic neuropathy associated with giant cell arteritis in Korea. Korean J Ophthalmol. 2017; 31:466–467. PMID:
28994270.

10. Lee SM, Shin DH, Choi JH, Jung JH. A case of bilateral arteritic anterior ischemic optic neuropathy in Korean patient. Clin Neuroophthalmol. 2018; 8:9–12.
11. Lee EJ, Woo KA, Koo DL. Giant cell arteritis associated arteritic anterior ischemic optic neuropathy: sudden vision loss on the contralateral side of headache. J Clin Neurol. 2018; 14:577–579. PMID:
30198237.

12. Miller NR. Anterior ischemic optic neuropathy: diagnosis and management. Bull N Y Acad Med. 1980; 56:643–654. PMID:
6932236.
13. Miller NR, Arnold AC. Current concepts in the diagnosis, pathogenesis and management of nonarteritic anterior ischaemic optic neuropathy. Eye (Lond). 2015; 29:65–79. PMID:
24993324.

14. Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990; 33:1122–1128. PMID:
2202311.

15. Hayreh SS. Ischemic optic neuropathies-where are we now? Graefes Arch Clin Exp Ophthalmol. 2013; 251:1873–1884. PMID:
23821118.
16. Gruener AM, Chang JR, Bosley TM, Al-Sadah ZM, Kum C, McCulley TJ. Relative frequencies of arteritic and nonarteritic anterior ischemic optic neuropathy in an Arab population. J Neuroophthalmol. 2017; 37:382–385. PMID:
28099197.

17. Tatò F, Hoffmann U. Giant cell arteritis: a systemic vascular disease. Vasc Med. 2008; 13:127–140. PMID:
18593802.

18. Nuenninghoff DM, Hunder GG, Christianson TJ, McClelland RL, Matteson EL. Incidence and predictors of large-artery complication (aortic aneurysm, aortic dissection, and/or large-artery stenosis) in patients with giant cell arteritis: a population-based study over 50 years. Arthritis Rheum. 2003; 48:3522–3531. PMID:
14674004.

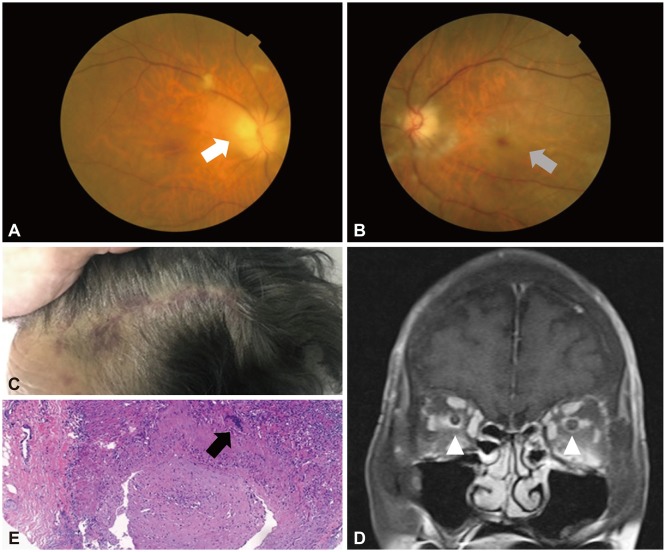
19. Currey J. Scalp necrosis in giant cell arteritis and review of the literature. Br J Rheumatol. 1997; 36:814–816. PMID:
9255121.

20. Tsianakas A, Ehrchen JM, Presser D, Fischer T, Kruse-Loesler B, Luger TA, et al. Scalp necrosis in giant cell arteritis: case report and review of the relevance of this cutaneous sign of large-vessel vasculitis. J Am Acad Dermatol. 2009; 61:701–706. PMID:
19577329.

21. Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol. 2001; 119:1299–1306. PMID:
11545635.
22. Hickman SJ. Optic perineuritis. Curr Neurol Neurosci Rep. 2016; 16:16. PMID:
26753870.

23. Byon IS, Jung JH, Kim HY, Park SW, Lee JE. Optic perineuritis secondary to acute retinal necrosis. J Neuroophthalmol. 2013; 33:419–421. PMID:
24177430.

24. Morgenstern KE, Ellis BD, Schochet SS, Linberg JV. Bilateral optic nerve sheath enhancement from giant cell arteritis. J Rheumatol. 2003; 30:625–627. PMID:
12610827.
25. Morotti A, Liberini P, Padovani A. Bilateral optic perineuritis as the presenting feature of giant cell arteritis. BMJ Case Rep. 2013; 2013:bcr2011007959.

26. Attaseth T, Vanikieti K, Poonyathalang A, Preechawat P, Jindahra P, Wattanatranon D. Anterior ischemic optic neuropathy due to biopsy-proven giant cell arteritis in Thai patients. Clin Ophthalmol. 2015; 9:1071–1075. PMID:
26109841.

27. Liu TY, Miller NR. Giant cell arteritis presenting as unilateral anterior ischemic optic neuropathy associated with bilateral optic nerve sheath enhancement on magnetic resonance imaging. J Neuroophthalmol. 2015; 35:360–363. PMID:
26087368.

28. Bengtsson BA, Malmvall BE. The epidemiology of giant cell arteritis including temporal arteritis and polymyalgia rheumatica. Incidences of different clinical presentations and eye complications. Arthritis Rheum. 1981; 24:899–904. PMID:
7259802.
29. Graham E, Holland A, Avery A, Russell RW. Prognosis in giant-cell arteritis. Br Med J (Clin Res Ed). 1981; 282:269–271.

30. Aiello PD, Trautmann JC, McPhee TJ, Kunselman AR, Hunder GG. Visual prognosis in giant cell arteritis. Ophthalmology. 1993; 100:550–555. PMID:
8479714.

31. Baldursson O, Steinsson K, Björnsson J, Lie JT. Giant cell arteritis in Iceland. An epidemiologic and histopathologic analysis. Arthritis Rheum. 1994; 37:1007–1012. PMID:
8024610.
32. Liu GT, Glaser JS, Schatz NJ, Smith JL. Visual morbidity in giant cell arteritis. Clinical characteristics and prognosis for vision. Ophthalmology. 1994; 101:1779–1785. PMID:
7800356.
33. Chen JJ, Leavitt JA, Fang C, Crowson CS, Matteson EL, Warrington KJ. Evaluating the incidence of arteritic ischemic optic neuropathy and other causes of vision loss from giant cell arteritis. Ophthalmology. 2016; 123:1999–2003. PMID:
27297405.

34. Giambene B, Sodi A, Sofi F, Marcucci R, Fedi S, Abbate R, et al. Evaluation of traditional and emerging cardiovascular risk factors in patients with non-arteritic anterior ischemic optic neuropathy: a case-control study. Graefes Arch Clin Exp Ophthalmol. 2009; 247:693–697. PMID:
19052769.

35. Arda H, Birer S, Aksu M, Ismailogullari S, Karakucuk S, Mirza E, et al. Obstructive sleep apnoea prevalence in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol. 2013; 97:206–209. PMID:
23203698.

36. Kim DH, Shin GR, Choi YJ. Risk factors for non-arteritic anterior ischaemic optic neuropathy in a Korean population. Neuroophthalmology. 2017; 41:68–75. PMID:
28348628.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download