Abstract
Background and Purpose
Cluster headache (CH) can present with migrainous symptoms such as nausea, photophobia, and phonophobia. In addition, an overlap between CH and migraine has been reported. This study aimed to determine the differences in the characteristics of CH according to the presence of comorbid migraine.
Methods
This study was performed using data from a prospective multicenter registry study of CH involving 16 headache clinics. CH and migraine were diagnosed by headache specialists at each hospital based on third edition of the International Classification of Headache Disorders (ICHD-3). We interviewed patients with comorbid migraine to obtain detailed information about migraine. The characteristics and psychological comorbidities of CH were compared between patients with and without comorbid migraine.
Results
Thirty (15.6%) of 192 patients with CH had comorbid migraine, comprising 18 with migraine without aura, 1 with migraine with aura, 3 with chronic migraine, and 8 with probable migraine. Compared to patients with CH without migraine, patients with CH with comorbid migraine had a shorter duration of CH after the first episode [5.4±7.4 vs. 9.0±8.2 years (mean±standard deviation), p=0.008], a lower frequency of episodic CH (50.0% vs. 73.5%, p=0.010), and a higher frequency of chronic CH (13.3% vs. 3.7%, p=0.033). Psychiatric comorbidities did not differ between patients with and without comorbid migraine. The headaches experienced by patients could be distinguished based on their trigeminal autonomic symptoms, pulsating character, severity, and pain location.
Cluster headache (CH) is a rare primary headache disorder with very severe pain characterized by autonomic symptoms and periodicity, and is the most common type of headache categorized under trigeminal autonomic cephalagia.1 Most patients with CH are classified as having episodic CH since they have a headache-free period of several months or even years, the so-called remission period. Those patients without such a long remission period are classified as having chronic CH.123
An overlap between CH and migraine has been reported. In addition to autonomic symptoms, 25–46% of patients with CH experience and report migraine-like features such as nausea, photophobia, phonophobia, and sometimes migraine itself.456 Furthermore, CH and migraine may share common clinical features such as unilateral pain location, similar triggering factors (histamine, calcitonin-gene-related peptide, or nitrate), a triptan response, and the treatment effect of neuromodulation.789 Moreover, a possible genetic link between CH and migraine has also been reported.10 Underlying migraine can delay the diagnosis of CH, which is of concern since the main abortive and preventive medications differ for the two disorders. Thus, both accurately diagnosing CH and distinguishing CH from migraine are essential to the correct management of CH. In addition, comorbidity of CH and migraine may reveal common neurobiological mechanisms.
A few studies have investigated the coincidence of CH and migraine, with comorbid migraine reportedly being present in 10–16.7% of patients with CH.41112 However, the differences between the characteristics of CH and migraine have not been evaluated adequately. Several other aspects also remain unknown, such as the times of onset of CH and migraine, clinical parameters for differentiation, and treatment pattern for migraine in patients who suffer from both migraine and CH. In this study we aimed to determine the differences in the characteristics and comorbidities of CH according to the history of preceding migraine, and to elucidate the detailed history of migraine in patients with CH.
The Korean Cluster Headache Registry (KCHR) is a prospective, multicenter, observational, registry-based study that included patients with CH at 16 hospitals in Korea between September 2016 and July 2018.13 In the present study, we included adult patients who were diagnosed as having CH (episodic, chronic, or probable CH) based on the judgment of the neurology board members. CH was diagnosed based on the third edition of the International Classification of Headache Disorders, 3rd edition beta version (ICHD-3 beta).14 Patients who were unable to communicate in Korean, who were unable to give reliable answers to questionnaires due to psychiatric reasons or cognitive decline at the time of the investigator's decision, or who were included in other clinical studies were not registered in the KCHR.1315 For our substudy we enrolled only those KCHR participants with CH compatible with the ICHD-3.1 Our study was approved by an Internal Review Board and a local ethics committee at each hospital (2016–396-I). All patients enrolled in the KCHR had already provided written informed consent, and all procedures complied with the tenets of the Declaration of Helsinki and Good Clinical Practice guidelines.
We have previously reported on the detailed protocol of the KCHR.1316 The clinical data collected about the last ictal period included sex, age at onset, body mass index, time to diagnosis of CH from the first headache onset, CH severity on a numeric rating scale (from 0 to 10), frequency of CH, mean duration of CH since the first episode, bout duration of CH during the ictal period, total number of CH bouts, smoking history (current smoker, ex-smoker, or never smoked), alcohol intake, headache impact (Headache Impact Test-6; HIT-6), anxiety (General Anxiety Disorder-7 scale; GAD-7), depression (Patient Health Questionnaire-9; PHQ-9), stress (Short-Form Perceived Stress Scale-4; PSS-4), quality of life (EuroQol: EQ-5D health utility score), and cutaneous allodynia (Allodynia Symptoms Scale-12).17181920 The bout duration was defined as the duration between the first day to the last day of cluster periods in which cluster attacks occurred in series lasting for weeks or months separated by remission periods, which usually lasted several months or even years.1 The total number of bouts was defined as total number of developing bout (cluster period) diagnosed as the CH. For all participants the investigators ascertained the presence of comorbid migraine based on the ICHD-3. The type of migraine was classified into migraine without aura, migraine with aura, chronic migraine, and probable migraine.1
We performed a comprehensive face-to-face or telephonic interview with each patient who agreed to participate to obtain further information about migraine and its relationship with CH. Furthermore, we assessed time parameters for diagnosing CH and migraine, clinical parameters for differentiating between patients with CH with and without migraine, and curative and preventive medications for migraine.
IBM SPSS Statistics software (version 20.0 for Windows, IBM Corporation, Armonk, NY, USA) was used for statistical analysis. Kolmogorov-Smirnov tests were performed to investigate whether the included variables conformed to a normal distribution. The chi-square test and Fisher's exact test were used to compare categorical variables, and the independent t-test was used to compare continuous variables. When normality was not present, continuous variables were analyzed using the Mann-Whitney U test or Kruskal-Wallis test. For convenience, the presence of migraine was dichotomized into with and without migraine regardless of the migraine classification. A probability value of p<0.05 in two-tailed tests was considered statistically significant.
Among 194 patients identified as having CH based on ICHD-3, 1 patient was excluded due to not meeting ICHD-3 criteria and another patient was excluded due to an uncertain history of migraine. We therefore finally analyzed 192 CH patients, comprising 26 with their first episode of CH, 134 with episodic CH, 10 with chronic CH, and 22 with probable CH. Their age was 38.1±10.8 years (mean±standard deviation) and 160 (83.3%) of them were male. The age at the onset of CH was 29.6±12.5 years and the CH duration was 8.4± 8.1 years. The score on the numeric rating scale for CH severity from the latest ictal period was 8.9±1.2. The frequency of CH was 2.2±1.8 per day during the latest ictal period, and the total number of CH bouts was 8.7±13.2.
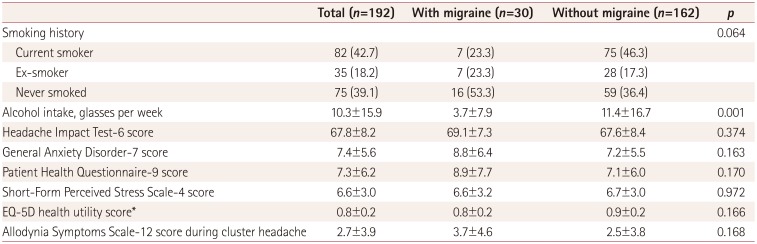
Thirty (15.6%) of the 192 patients with CH had comorbid migraine, comprising 18 with migraine without aura, 1 with migraine with aura, 3 with chronic migraine, and 8 with probable migraine. The CH duration was shorter in patients with CH with comorbid migraine than in those without (5.4±7.4 vs. 9.0±8.2 years, p=0.008), and the time delay to a CH diagnosis was shorter in patients with CH and comorbid migraine than in those without migraine (3.2±5.5 vs. 5.9±7.3 years, p=0.032). Episodic CH was less common (50.0% vs. 73.5%, p=0.010) and chronic CH was more common (13.3% vs. 3.7%, p=0.033) in patients with CH and comorbid migraine than in those without migraine. There were no significant differences between the patients with and without comorbid migraine in the age at study inclusion (37.6±8.4 vs. 38.2±11.3 years, p=0.781), age at CH onset (32.2±11.6 vs. 29.2±12.7 years, p=0.232), or total number of bouts (7.6±10.2 vs. 8.9±13.7 years, p=0.625) (Table 1). The following characteristics of CH and its comorbidity also did not differ significantly between patients with and without migraine history: HIT-6 score (69.1±7.3 vs. 67.6±8.4, p=0.374), GAD-7 score (8.8±6.4 vs. 7.2±5.5, p=0.163), PHQ-9 score (8.9±7.7 vs. 7.1±6.0, p=0.170), PSS-4 score (6.6±3.2 vs. 6.7±3.0, p=0.972), and EQ-5D score (0.8±0.2 vs. 0.9±0.2, p=0.166) (Table 2).
Nineteen of the 30 patients with CH and comorbid migraine participated in detailed interviews. The age at the onset of migraine was 27.6±9.3 years. The onset of migraine preceded the onset of CH by 6.5±4.9 years in 12 patients, the onset of CH preceded the onset of migraine by 9.7±5.5 years in 4 patients, and the onset of both conditions occurred in the same year in 3 patients. These patients distinguished their CH from migraine based on 3.5±1.7 features (range 1–8 features): trigeminal autonomic symptoms (n=14), pulsating character (n=8), severity (n=7), location of pain (n=7), timing of pain (n=6), presence of nausea (n=6), premonitory symptoms (just feeling) (n=5), frequency (n=5), phonophobia or photophobia (n=4), and agitation (n=4). As curative medications for migraine, 6 patients took triptans, 11 took nonsteroidal anti-inflammatory drugs, and 4 took acetaminophen, while 1 patient did not take any medication. Eight patients reported that the migraine-associated pain was endurable and wanted to defer medication use until the cluster period, three patients did not take any curative medication, and five patients took acetaminophen or acetaminophen-combination medications. Three patients took preventive medication for migraine: one took cinnarizine, one took topiramate and amitriptyline, and one took candesartan and amitriptyline. Two patients had a history of episodic tension-type headaches additional to CH and migraine.
The key findings of our study were as follows: First, 30 (15.6%) of the 192 patients had comorbid migraine, and the frequency of chronic CH was higher in patients with comorbid migraine than in those without migraine (13.3% vs. 3.7%). Second, the clinical characteristics and psychiatric comorbidity did not differ according to the presence of comorbid migraine in patients with CH. Third, comorbid migraine was associated with a shorter duration of CH and shorter delay in diagnosing CH.
To our knowledge, this is the first study to prospectively investigate migraine comorbidity and its relationship with CH in patients with ICHD-3-compatible CH. Migraine is reportedly present in about one-fourth of patients with CH, but the additional diagnosis of migraine based on the ICHD-3 has not been evaluated in patients with CH.6 In our study, the prevalence of migraine comorbidity was 15.6% in all CH patients, and as higher as 40% in patients with chronic CH. Our study results are consistent with a Swedish study finding migraine in 15.6% of patients with episodic CH and 22.2% of patients with chronic CH.12 Regarding the prevalence of chronic CH being higher with migraine comorbidity, the traditional hypothesis is that migraines may culminate into CH.21 However, both CH and migraine were considered as different clinical entities, with either of them potentially leading to the other.1122 Furthermore, considering chronicity, a central sensitization or biological correlation could result in a closer association between chronic CH and migraine.2324
In our study we found that most of the clinical parameters and psychiatric comorbidities did not differ significantly according to the presence of migraine comorbidity, except for the disease duration and diagnostic delay time in patients with CH. The trigeminovascular system, parasympathetic nerve fibers (trigeminal autonomic reflex), and the hypothalamus are three key structures associated with CH.7 Despite CH and migraine having been categorized as different diseases, as mentioned above, CH presents with headache-associated symptoms such as nausea, photophobia, and phonophobia that are similar to those appearing in migraine. Moreover, considering their disease mechanisms, hypothalamus involvement in migraine pathophysiology is also closely associated with triggering CH.25 Psychosocial problems including stress levels and the daily quality of life of patients with CH have not previously been researched in the context of the history of migraine comorbidity. In our study, stress and psychiatric comorbidities did not differ with the presence of comorbid migraine. These results are in line with previous studies showing that the presence of comorbid migraine does not affect the pain intensity and clinical characteristics of CH;46 furthermore, our results additionally indicate that psychological comorbidities do not differ among patients with CH according to the presence or absence of comorbid migraine.
Contrary to the belief that migraine can cause a diagnostic delay in CH,26 we found that the headache duration and diagnostic delay time were shorter in patients with CH and comorbid migraine than in those without migraine comorbidity. Although the underlying mechanism remains unclear, this may be due to the onset of migraine occurring earlier than that of CH, which was reported in two-thirds of patients interviewed in our study; these patients may therefore have focused more on their headache and sought medical advice, which may have facilitated the early diagnosis of CH. In addition, our patients with both CH and migraine reported that they regarded their migraine headaches as less severe than CH. This may have resulted in a difference between the medications they used for migraine or CH.
Our research was subject to some limitations. First, although we screened a large number of patients with CH who were recruited from a multicenter study, only a relatively small number of patients with comorbid migraine participated in the interview substudy. Thus, our results might not be generalizable before more patients are investigated in a population-based study. Second, although our study included more patients with migraine than in other studies, the number was still not sufficient for a more-detailed comparison that also considered the subtypes of migraine. Third, the relationship between CH and migraine was judged based on the medical records and history-taking, and not in a prospective follow-up.
In conclusion, this study found no significant differences in the characteristics of CH and its comorbidities according to the presence of comorbid migraine. However, the chronic CH subtype appeared more often with comorbid migraine, which may make the diagnosis of CH faster and easier. The correct management of both primary headache disorders requires clinicians to check for the history of preceding migraine or to follow up the occurrence of migraine during the diagnosis and management of CH.
Acknowledgements
This project was supported by grant from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (2018R1D1A1B07040959).
References
1. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018; 38:1–211.
2. Ljubisavljevic S, Zidverc Trajkovic J. Cluster headache: pathophysiology, diagnosis and treatment. J Neurol. 2018; 8. 17. DOI: 10.1007/s00415-018-9007-4. [Epub].

3. Burish M. Cluster headache and other trigeminal autonomic cephalalgias. Continuum (Minneap Minn). 2018; 24:1137–1156. PMID: 30074553.

4. Gaul C, Christmann N, Schröder D, Weber R, Shanib H, Diener HC, et al. Differences in clinical characteristics and frequency of accompanying migraine features in episodic and chronic cluster headache. Cephalalgia. 2012; 32:571–577. PMID: 22529192.

5. Taga A, Russo M, Manzoni GC, Torelli P. Cluster headache with accompanying migraine-like features: a possible clinical phenotype. Headache. 2017; 57:290–297. PMID: 27861832.

6. Zidverc-Trajkovic J, Podgorac A, Radojicic A, Sternic N. Migraine-like accompanying features in patients with cluster headache. How important are they? Headache. 2013; 53:1464–1469. PMID: 23534887.

7. Vollesen AL, Benemei S, Cortese F, Labastida-Ramírez A, Marchese F, Pellesi L, et al. Migraine and cluster headache-the common link. J Headache Pain. 2018; 19:89. PMID: 30242519.
8. Láinez MJ, Guillamón E. Cluster headache and other TACs: pathophysiology and neurostimulation options. Headache. 2017; 57:327–335. PMID: 28128461.

9. Vukovic Cvetkovic V, Jensen RH. Neurostimulation for the treatment of chronic migraine and cluster headache. Acta Neurol Scand. 2019; 139:4–17. PMID: 30291633.

10. Kudrow L, Kudrow DB. Inheritance of cluster headache and its possible link to migraine. Headache. 1994; 34:400–407. PMID: 7928324.

11. D'Amico D, Centonze V, Grazzi L, Leone M, Ricchetti G, Bussone G. Coexistence of migraine and cluster headache: report of 10 cases and possible pathogenetic implications. Headache. 1997; 37:21–25. PMID: 9046719.
12. Steinberg A, Fourier C, Ran C, Waldenlind E, Sjöstrand C, Belin AC. Cluster headache-clinical pattern and a new severity scale in a Swedish cohort. Cephalalgia. 2018; 38:1286–1295. PMID: 28906127.
13. Choi YJ, Kim BK, Chung PW, Lee MJ, Park JW, Chu MK, et al. Impact of cluster headache on employment status and job burden: a prospective cross-sectional multicenter study. J Headache Pain. 2018; 19:78. PMID: 30178397.

14. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013; 33:629–808. PMID: 23771276.
15. Song TJ, Kim YJ, Kim BK, Kim BS, Kim JM, Kim SK, et al. Characteristics of elderly-onset (≥65 years) headache diagnosed using the International Classification of Headache Disorders, third edition beta version. J Clin Neurol. 2016; 12:419–425. PMID: 27819415.

16. Sohn JH, Choi YJ, Kim BK, Chung PW, Lee MJ, Chu MK, et al. Clinical features of probable cluster headache: a prospective, cross-sectional multicenter study. Front Neurol. 2018; 9:908. PMID: 30416482.

17. Seo JG, Park SP. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. 2015; 16:97. PMID: 26596588.

18. Seo JG, Park SP. Validation of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with migraine. J Headache Pain. 2015; 16:65. PMID: 26174509.

19. Lee EH, Chung BY, Suh CH, Jung JY. Korean versions of the Perceived Stress Scale (PSS-14, 10 and 4): psychometric evaluation in patients with chronic disease. Scand J Caring Sci. 2015; 29:183–192. PMID: 24660854.

20. Lee YK, Nam HS, Chuang LH, Kim KY, Yang HK, Kwon IS, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. 2009; 12:1187–1193. PMID: 19659703.

21. Wei DY, Yuan Ong JJ, Goadsby PJ. Cluster headache: epidemiology, pathophysiology, clinical features, and diagnosis. Ann Indian Acad Neurol. 2018; 21:S3–S8. PMID: 29720812.

22. Boes CJ, Capobianco DJ, Matharu MS, Goadsby PJ. Wilfred Harris' early description of cluster headache. Cephalalgia. 2002; 22:320–326. PMID: 12100097.

23. Mosnaim AD, Puente J, Wolf ME. Biological correlates of migraine and cluster headaches: an overview of their potential use in diagnosis and treatment. Pragmat Obs Res. 2010; 1:25–32. PMID: 27774006.

24. D'Andrea G, Terrazzino S, Leon A, Fortin D, Perini F, Granella F, et al. Elevated levels of circulating trace amines in primary headaches. Neurology. 2004; 62:1701–1705. PMID: 15159465.
25. Overeem S, Van Vliet JA, Lammers GJ, Zitman FG, Swaab DF, Ferrari MD. The hypothalamus in episodic brain disorders. Lancet Neurol. 2002; 1:437–444. PMID: 12849366.

26. Bahra A, Goadsby PJ. Diagnostic delays and mis-management in cluster headache. Acta Neurol Scand. 2004; 109:175–179. PMID: 14763953.

Table 1
Comparative analysis of demographics according to the history of preceding migraine
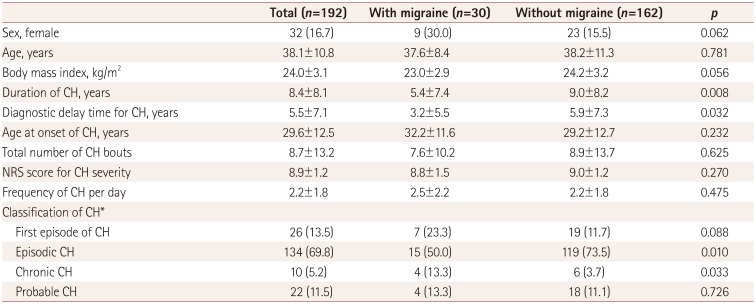
Table 2
Comparative analysis of clinical variables according to the history of preceding migraine




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download