1. Hodges JR, Warlow CP. Syndromes of transient amnesia: towards a classification. A study of 153 cases. J Neurol Neurosurg Psychiatry. 1990; 53:834–843. PMID:
2266362.

2. Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol. 2010; 9:205–214. PMID:
20129169.

3. Burwell RD. The parahippocampal region: corticocortical connectivity. Ann N Y Acad Sci. 2000; 911:25–42. PMID:
10911865.

4. Libby LA, Ekstrom AD, Ragland JD, Ranganath C. Differential connectivity of perirhinal and parahippocampal cortices within human hippocampal subregions revealed by high-resolution functional imaging. J Neurosci. 2012; 32:6550–6560. PMID:
22573677.

5. Ranganath C, Ritchey M. Two cortical systems for memory-guided behaviour. Nat Rev Neurosci. 2012; 13:713–726. PMID:
22992647.

6. La Joie R, Landeau B, Perrotin A, Bejanin A, Egret S, Pélerin A, et al. Intrinsic connectivity identifies the hippocampus as a main crossroad between Alzheimer's and semantic dementia-targeted networks. Neuron. 2014; 81:1417–1428. PMID:
24656258.

7. Yi S, Park YH, Jang JW, Lim JS, Chun IK, Kim S. Decreased metabolism in the posterior medial network with concomitantly increased metabolism in the anterior temporal network during transient global amnesia. Brain Topogr. 2018; 31:468–476. PMID:
29038979.

8. Park YH, Jeong HY, Jang JW, Park SY, Lim JS, Kim JY, et al. Disruption of the posterior medial network during the acute stage of transient global amnesia: a preliminary study. Clin EEG Neurosci. 2016; 47:69–74. PMID:
25392008.
9. Trenner MU, Fahle M, Fasold O, Heekeren HR, Villringer A, Wenzel R. Human cortical areas involved in sustaining perceptual stability during smooth pursuit eye movements. Hum Brain Mapp. 2008; 29:300–311. PMID:
17415782.

10. Morrow MJ, Sharpe JA. Cerebral hemispheric localization of smooth pursuit asymmetry. Neurology. 1990; 40:284–292. PMID:
2300251.

11. Lencer R, Trillenberg P. Neurophysiology and neuroanatomy of smooth pursuit in humans. Brain Cogn. 2008; 68:219–228. PMID:
18835076.

12. Komatsu H, Wurtz RH. Modulation of pursuit eye movements by stimulation of cortical areas MT and MST. J Neurophysiol. 1989; 62:31–47. PMID:
2754480.

13. Mikami A, Newsome WT, Wurtz RH. Motion selectivity in macaque visual cortex I Mechanisms of direction and speed selectivity in extrastriate area MT. J Neurophysiol. 1986; 55:1308–1327. PMID:
3016210.

14. Dürsteler MR, Wurtz RH. Pursuit and optokinetic deficits following chemical lesions of cortical areas MT and MST. J Neurophysiol. 1988; 60:940–965. PMID:
3171667.
15. Orban GA, Van Essen D, Vanduffel W. Comparative mapping of higher visual areas in monkeys and humans. Trends Cogn Sci. 2004; 8:315–324. PMID:
15242691.

16. Barnes GR. Cognitive processes involved in smooth pursuit eye movements. Brain Cogn. 2008; 68:309–326. PMID:
18848744.

17. Kerzel D, Souto D, Ziegler NE. Effects of attention shifts to stationary objects during steady-state smooth pursuit eye movements. Vision Res. 2008; 48:958–969. PMID:
18295816.

18. Treue S, Maunsell JH. Effects of attention on the processing of motion in macaque middle temporal and medial superior temporal visual cortical areas. J Neurosci. 1999; 19:7591–7602. PMID:
10460265.

19. Contreras R, Ghajar J, Bahar S, Suh M. Effect of cognitive load on eyetarget synchronization during smooth pursuit eye movement. Brain Res. 2011; 1398:55–63. PMID:
21620377.

20. Hutton SB, Tegally D. The effects of dividing attention on smooth pursuit eye tracking. Exp Brain Res. 2005; 163:306–313. PMID:
15654587.

21. Chung YA, Jeong J, Yang DW, Kang BJ, Kim SH, Chung SK, et al. A Tc-99m SPECT study of regional cerebral blood flow in patients with transient global amnesia. Neuroimage. 2009; 47:50–55. PMID:
19073268.

22. Kim BS, Cho SS, Choi JY, Kim YH. Transient global amnesia: a study with Tc-99m ECD SPECT shortly after symptom onset and after recovery. Diagn Interv Radiol. 2016; 22:476–480. PMID:
27535207.

23. Matsuda H, Higashi S, Tsuji S, Sumiya H, Miyauchi T, Hisada K, et al. High resolution Tc-99m HMPAO SPECT in a patient with transient global amnesia. Clin Nucl Med. 1993; 18:46–49. PMID:
8422720.

24. Segraves MA, Goldberg ME, Deng SY, Bruce CJ, Ungerleider LG, Mishkin M. The role of striate cortex in the guidance of eye movements in the monkey. J Neurosci. 1987; 7:3040–3058. PMID:
3668615.

25. Robinson DA. The mechanics of human smooth pursuit eye movement. J Physiol. 1965; 180:569–591. PMID:
5846794.

26. Ono S, Mustari MJ. Smooth pursuit-related information processing in frontal eye field neurons that project to the NRTP. Cereb Cortex. 2009; 19:1186–1197. PMID:
18820288.

27. Lindner A, Haarmeier T, Erb M, Grodd W, Thier P. Cerebrocerebellar circuits for the perceptual cancellation of eye-movement-induced retinal image motion. J Cogn Neurosci. 2006; 18:1899–1912. PMID:
17069480.

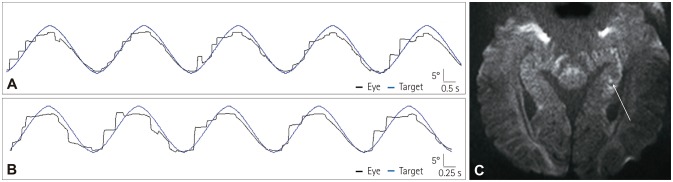
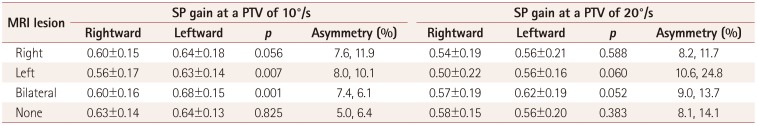
28. Yang Y, Kim JS, Kim S, Kim YK, Kwak YT, Han IW. Cerebellar hypoperfusion during transient global amnesia: an MRI and oculographic study. J Clin Neurol. 2009; 5:74–80. PMID:
19587813.

29. Keller EL, Heinen SJ. Generation of smooth-pursuit eye movements: neuronal mechanisms and pathways. Neurosci Res. 1991; 11:79–107. PMID:
1656345.

30. Westmacott R, Silver FL, McAndrews MP. Understanding medial temporal activation in memory tasks: evidence from fMRI of encoding and recognition in a case of transient global amnesia. Hippocampus. 2008; 18:317–325. PMID:
18064704.

31. Bartsch T, Schönfeld R, Müller FJ, Alfke K, Leplow B, Aldenhoff J, et al. Focal lesions of human hippocampal CA1 neurons in transient global amnesia impair place memory. Science. 2010; 328:1412–1415. PMID:
20538952.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download