This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Undescended testis (UDT) is a developmental defect in which one or both testicles do not arrive in the scrotum. Its prevalence at birth and one year after is 2%–4% and less than 1%, respectively. Currently, surgery is recommended to treat congenital cryptorchidism in order to prevent testicular degeneration. Classic method is performed via incision in inguinal and scrotum and the new method is done via incision in scrotum.
Method
Sixty male participants with 65 UDT undergoing surgery were randomly assigned to scrotal incision (n=31) and classic inguinal incision methods (n=34). Patients were followed for 6 months and testicular atrophy, infection, recurrence, and duration of surgery were compared between two groups.
Results
Scrotal incision compared to classic incision method had significantly lower duration of surgery (19.06±2.96 minutes vs. 30±10.42 minutes; p=0.002) and recurrence during follow-up (0 vs. 5 cases; p=0.026). There was only one surgical site infection in the scrotal incision method. There were hematoma and post-operative swelling in 13.3% of cases after scrotal incision method.
Conclusion
Scrotal incision is an alternative method for the UDT with lower duration of surgery, lower recurrence rate, and better cosmetic results.
Keywords: Orchiopexy, Scrotal incision, Undescended testis
INTRODUCTION
Cryptorchidism or undescended testis (UDT) is a developmental defect in which one or both testicles do not arrive in the scrotum [
1]. Its prevalence at birth and 1 year after birth is 2%–4% and less than 1%, respectively [
23]. Although causes of undescended testicle are not certainly known, the following risk factors are reported: gonadotropin stimulation failure, taking estrogen during pregnancy, disorder of gubernaculums, lack of stimulation testicular descent by genitofemoral nerve, epididymal anomalies, and abdominal wall abnormalities [
4].
Most of undescended testicles move down in the first three months of life and a few percent over the next 9 months [
5]. Although the morphology of undescended testicles is almost normal, reducing the number of primary reproductive cells is often seen up to 2 years of age [
4].
Hormone therapy is one of the treatment options with less than 30% response rate depending on being unilateral or bilateral as well as the age of patients. Surgery is recommended before 1 years old in order to reduce complications [
67].
Cryptorchidism is usually operated by incision in inguinal and scrotum through which it is associated with inguinal hernia. Sometimes, the testicle is located inlet of scrotal sac that is called low-lying UDT. In these cases, orchiopexy can be performed by only an incision in the scrotum, if there is no obvious hernia sac in preoperative examination [
89]. Traditional method for treatment of the UDT is inguinal approach including 2 incisions: inguinal incision to access the inguinal canal and scrotal incision to conduct orchiopexy [
10]. It was suggested that inguinal incision is more helpful in visualizing and mobilizing the spermatic cord, hernia sac, and high ligation of the sac to achieve adequate length for testis to be posited in the scrotum and fixated by means of a dartos pouch [
11-
13]. Scrotal incision method was developed by Bianchi and Squire [
14] to decrease the potential morbidity of traditional inguinal incision method (bianchi). In the present study, we compared transscrotal and traditional inguinal approaches for performing orchiopexy in patients with an UDT.
METHODS
In this study, 60 male patients with 65 UDT undergoing surgery in Pediatric Hospital, Tabriz, Iran, between March 2014 and March 2015, were recruited. All the boys under 2 years old with low lying UDT whose testis was palpable in inguinal canal were included. Children with history of inguinal or abdominal surgery, secondary ascending testis, ectopic testis, UDT related to intersex situation or ambiguous genitalia, primary or secondary hypogonadism, known hormonal disorders, hormone therapy, retractile testis, UDT inter abdominal or above the inguinal canal, and recurrent cases were excluded. The study was approved by the Ethics Committee of Tabriz University of Medical Sciences and the written informed consent was obtained from parents or legal guardians of children (IR.TBZMED.REC.1394.819).
Using RandList 1.2 software, random numbers were produced and patients were selected according to the sample size. The case group included 30 patients that were operated with the minimally invasive trans-scrotal orchiopexy and the control group included 30 patients that were operated with classic technique via 2 incisions (scrotal and inguinal). All operations were performed by 1 surgeon (Badbarin D). In the traditional approach, the following 2 skin incisions were used. At first, an inguinal incision was made to access inguinal canal in order to visualize the cord structures to separation and high ligation of the hernia sac in order to achieve an adequate length for the testis to be posited to the scrotum. Then, scrotal incision was made to fix the testis in the scrotum by means of dartos pouch with the chromic suture to the tunica albuginea. Next, skin and dartos fascia was repaired, respectively.
In scrotal incision method, an incision is made in scrotal skin and subcutaneous tissues and fascia was dissected to carry down to the tunica vaginalis. Gubernacular attachments were divided. Using the gentle traction on the testis, the mobilization of the spermatic cord was performed. Cremasteric fibers were cut to achieve excess mobilization. Hernia sac was carefully separated from the spermatic cord and then was high-ligated. Additional dissection is carried along the cord by opening the external ring and canal, if additional cord length is needed. Dartos pouch was created and the testis was fixed in it with the chromic suture to the tunica albuginea. Finally, dartos fascia and skin were repaired, respectively.
Patients were followed for 6 months after surgery and were analyzed in terms of recurrence and testis retraction, duration of surgery, and complications of surgery such as testicles atrophy. Duration of surgery and wound infection was considered as primary outcomes and recurrence and testicle atrophy as secondary outcomes. Ultrasonography used as a good and reliable tool for determining testicular size. Parents were asked about their satisfaction with the cosmetic result of the operation. Their opinions were submitted as satisfied or unsatisfied.
1. Statistics
Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). The t-test, χ2 test, and fisher's exact test were used for data analysis. The p<0.05 were deemed to be statistically significant.
RESULTS
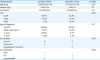
Sixty patients (65 testicles) underwent orchiopexy using scrotal incision method (n=31) or inguinal incision method (n=34). The baseline data is demonstrated in
Table 1. There was a significant difference between scrotal incision and inguinal incision groups in terms of the operation time (minutes) (19.06±2.96 vs 30±10.42; p=0.002).
Table 1
base line data
|
Characteristic |
Scrotal incision |
Inguinal incision |
p-value |
|
Age (mo) |
3.58±2.66 (1–14) |
2.57±2.03 (5–12) |
0.14 |
|
Weight (kg) |
5.85±1.53 |
5.26±1.2 |
0.1 |
|
Term born |
30 (100.0%) |
29 (96.7%) |
0.4 |
|
UDT |
|
|
<0.05 |
|
LUDT |
26.7% |
33.3% |
|
RUDT |
70.0% |
53.3% |
|
BUDT |
3.3% |
13.4% |
|
Age of diagnosis |
|
|
0.3 |
|
At birth |
60.0% |
80.0% |
|
Before admission |
16.7% |
10.0% |
|
<1 year |
20.0% |
6.7% |
|
>1 year |
3.3% |
3.3% |
|
Co-disease |
|
|
<0.05 |
|
Hernia |
2 |
7 |
|
Hydrocele |
3 |
1 |
|
Hyppoplastic scrotum |
- |
3 |
|
Co-anomalies |
|
|
<0.05 |
|
ASD |
1 |
- |
|
PS |
- |
1 |
|
Hypospadias |
4 |
1 |

After a week, 93.3% of testicles were in the scrotal pouch and 6.7% were the inlet of scrotum in scrotal incision method, while, in inguinal incision method, 100% of the testicles were in the scrotal pouch; however, this difference was not significant. There was no recurrence a week after surgery in both groups.
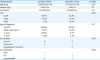
There were not any short-term complications after surgery in control group, while 4 cases of inflammation, 4 cases of hematoma, and 2 cases of swelling were seen in the scrotal incision group that is significantly higher than control group (p<0.05). Surgery site infection was occurred in the scrotal incision group (1 case), while it was not seen in inguinal incision group. However, there were no significant differences between 2 groups in this regard (p=0.5). It is worth mentioning that this complication was not worrisome and was treated during 1 week with antibiotics and conservative managements.
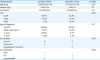
There was a significant difference between case and control groups in terms of recurrence after 6 months of surgery (0 vs. 5 cases; p=0.026). Testicle atrophy was not seen in the scrotal incision group, while 2 cases of testicle atrophy were reported in the inguinal incision group. Nevertheless, the differences were not significant (p=0.24). Testicles' size before and after 6 months surgery is demonstrated in
Table 2.
Table 2
Testicles size before and 6 months after surgery

|
Status |
Before surgery |
6 months after surgery |
|
Scrotal incision |
Inguinal incision |
Scrotal incision |
Inguinal incision |
|
¼ Normal |
13.3% |
40.0% |
6.6% |
6.6% |
|
½ Normal |
40.0% |
33.3% |
13.4% |
26.7% |
|
¾ Normal |
33.3% |
13.3% |
40.0% |
40.0% |
|
Normal |
13.4% |
13.4% |
40.0% |
26.7% |
|
p-value |
0.08 |
0.54 |

According to the
Table 3, satisfaction of incision scar was significantly higher in scrotal group. The scar was invisible during 6 months of follow-up visit in the majority of the patient in the scrotal incision group. Besides, the scrotal incision showed better cosmetic results. Short term and long-term complications are demonstrated in
Table 3.
Table 3
Complication

|
Complication |
Scrotal incision |
Inguinal incision |
p-value |
|
Short-term complication |
|
|
|
|
Inflammation |
4 cases |
- |
<0.05 |
|
Hematoma |
4 cases |
- |
<0.05 |
|
Swelling |
2 cases |
- |
<0.05 |
|
Surgery site infection |
1 case |
- |
0.5 |
|
Long-term complication |
|
|
|
|
Recurrence |
- |
5 cases |
0.026 |
|
Testicle atrophy |
- |
2 cases |
0.24 |
|
Satisfaction about scar |
100% |
76%/66% |
<0.05 |

DISCUSSION
UDT is the most common finding during routine examinations after childbirth in newborns. Several studies demonstrated different prevalence in all ages [
15]. Currently, surgery is recommended for congenital cryptorchidism in the early infancy to prevent testicle degeneration [
12].
The inguinal canal exploration is the old method for management and treatment of UDT. Opening the inguinal canal provides cord structure exploration, hernia sac ligation, and enough length access to pull down testicle to scrotum. Orchiopexy is done by the other incision in scrotum. Mobility of incision in children and short distance to the external ring has led to creating this idea that can operate UDT by the scrotal incision below the inguinal external ring [
1416].
Bassel et al. [
17] demonstrated that duration of surgery by scrotal incision is shorter than that of classic method. Similar results were obtained in studies of Karaman et al. [
11] and Dayanç et al. [
12] in which the operative time by scrotal incision method is significantly shorter than the inguinal incision technique.
Our results also showed that duration of surgery by scrotal incision technique is shorter than that of the other method (p=0.002). Moreover, in Na et al. [
10], the hospital stay and operation time were shorter in the scrotal incision technique than in the classic method.
Na et al. [
10] demonstrated that short term complications such as hematoma and wound dehiscence after scrotal incision surgery are more than those in the classic technique with 2 incisions. According to our results, some short-term complications such as hematoma, swelling, and inflammation occurred more frequently in children operated with scrotal incision technique (p<0.05).
Bassel et al. [
17] showed that complications after scrotal incision technique were lesser than inguinal incision technique. The only complication was wound infection and there were no testicular atrophy or ascent and hernia or hydrocele formation during 6 months up to 1 year follow-up.
One case of recurrence was reported in Russinko et al. [
18] during follow-up in the children operated with scrotal incision, while in our study; no recurrence and testicle atrophy were observed in scrotal incision technique. However, 2 cases of testicle atrophy and 5 cases of recurrences were seen in inguinal incision technique.
In addition, in Na et al. [
10], no cases of testicle atrophy were reported after the surgery via scrotal incision technique.
Bassel et al. [
17] demonstrated that scrotal incision method has less skin scar. Similar result was obtained in our study. Dayanç et al. [
12] showed that scrotal incision method is better than classic method in terms of cosmetic results.
In our study, normal testicle size before surgery was approximately 13% in both group, while, after surgery, except for two cases in the inguinal incision group, in the rest of the cases, the size of the testicles increased or remained unchanged that became normal via scrotal incision in most of the patients (40% in scrotal incision vs. 26.7% in inguinal incision).
According to the results, scrotal incision method has better cosmetic outcome, and less duration. In Na et al. [
10], scrotal incision is more feasible cosmetically.
In conclusion, according to the results of the present study, orchiopexy via the scrotal incision technique is better compared to the inguinal incision method in terms of operation time, cosmetic results, and long-term complications (recurrence) and is recommended for palpable low-lying UDT treatment.