Abstract
Background
Methods
Results
Figures and Tables
 | Figure 1Flow of patient selection. We excluded the patients with bronchiectasis, history of asthma and the patients with definite parenchymal infiltration on the initial chest X-ray. In addition, we excluded the patients who performed chest computed tomography (CT) before the initial chest X-ray or 48 hours after hospitalization and also excluded the patients who performed chest CT at a hospital or a clinic other than our medical center. Initial diagnosis of chronic obstructive pulmonary disease (COPD) exacerbation is aggravated respiratory symptoms in COPD patients and defined as no definite infiltration on initial chest X-ray. |
Table 1
Baseline patients' characteristics
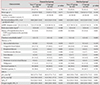
*Matched group: after propensity score matching, CT group and non-CT group was matched with baseline characteristics. The following variables were matched; sex, age, smoking status, Charlson comorbidity index, mMRC dyspnea scale, FEV1%, initial concentration of O2 supply. †Non-CT group: patients with COPD exacerbation but didn't performed chest CT. ‡CT group: patients with COPD exacerbation and performed chest CT within 72 hours after ER visit. §These characteristics were not normal distribution, and described as median (interquartile) scale. ∥The data of these characteristics were at the time in stable state of the COPD patients before hospitalization. ¶Charlson comorbidity index predict one-year mortality for patients who have comorbid conditions, such as heart disease, cancer, diabetes mellitus. Each condition is assigned a score of 1, 2, 3, or 6, depending on the risk of dying associated with each one.
Table 2
Changed or additional diagnosis and treatment after chest CT
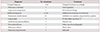
*After computed tomography (CT) diagnosis was changed in two patients out of 64 patients who performed CT. †17 out of 21 patients already used antibiotics before CT was performed; to only 4 patients, antibiotics was added. ‡One patient with lung nodule performed percutaneous needle biopsy for lung nodule and squamous cell carcinoma was diagnosed but no further treatment for poor performance status. The other patient with lung nodule was examined 6 months later, and the lung nodule disappeared at follow up chest CT.
Table 3
Clinical outcomes according to CT group vs. non-CT group

Matching variables were selected through a multivariate regression model of ICU care and hospital stay: sex, age, smoking status, Charlson comorbidity index, purulent sputum, history of hospitalization due to COPD exacerbation in the previous year, mMRC dyspnea scale, FEV1%, and initial concentration of O2 supply.
CT: computed tomography; ICU: intensive care unit; COPD: chronic obstructive pulmonary disease; mMRC: modified Medical Round Council Dyspnea Scale; FEV1: forced expiratory volume in 1 second.
Table 4
Length of hospital stay and performance of CT were not related significantly

Multiple linear regression analysis was performed with an adjustment of covariates; age, sex, FEV1, initial concentration of O2 supply, smoking, charlson comorbidity index, body mass index, history of hospitalization due to COPD exacerbation in the previous year, baseline mMRC dyspnea scale, increased or purulent sputum, initial pO2, pCO2 results.
CT: computed tomography; β: regression coefficient; FiO2: fraction of inspired oxygen; mMRC: modified Medical Research Council Dyspnea Scale; FEV1: forced expiratory volume in 1 second; COPD: chronic obstructive pulmonary disease; pO2: partial pressure of oxygen; pCO2: partial pressure of carbon dioxide.
Acknowledgments
Notes
Authors' Contributions
Conceptualization: Oh YM.
Methodology: Park HJ, Oh YM.
Formal analysis: Park HJ, Kim SH, Kim HC.
Data curation: Park HJ, Kim HC.
Validation: Seo JB, Lee BY, Lee SW, Lee JS, Lee SD.
Writing - original draft preparation: Park HJ, Kim SH.
Writing - review and editing: Park HJ, Oh YM.
Approval of final manuscript: all authors.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download