Abstract
Objective
Materials and Methods
Results
Conclusion
Notes
This study was supported by the Korea Ministry of Environment (MOE) as “The Environmental Health Action Program” [RE201806039, and RE201806027], Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education [NRF-2017R1D1A1B03034157, and NRF-2016R1D1A1B03936078], and National Institutes of Health (NIH) [S10 RR022421, U01 HL114494, U10 HL109152-04, 109257-04, 109168-04, 109172-04, 109046-04, 109250-05, 109164, 109086-04, and HHSN268200900013C, 268200900014C, 268200900015C, 268200900016C, 268200900017C, 268200900018C, 268200900019C, 268200900020C].
Conflicts of Interest: Eric A. Hoffman is a shareholder in VIDA diagnostics, a company that is commercializing lung image analysis software derived by the University of Iowa lung imaging group. He is also a member of the Siemens CT advisory board. Sean B. Fain receives grant funding from GE Healthcare. Mark L. Schiebler is a shareholder in Stemina Biomarker Discovery, Inc. and Healthmyne, Inc.
References
Supplementary Materials
Supplementary Table 1
Supplementary Table 2
Supplementary Table 3
Supplementary Table 4
Fig. 1
Flow chart of subject selection of male and female subgroups.
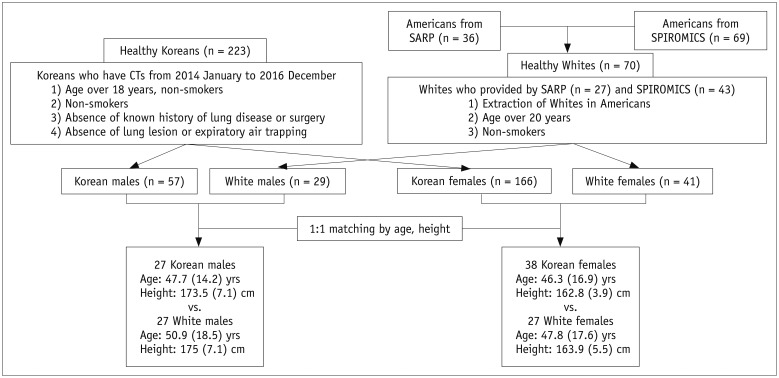
Fig. 2
A. Five central airways and five subgroups of segmental airway. B. Frontal view of color-coded five lobes.
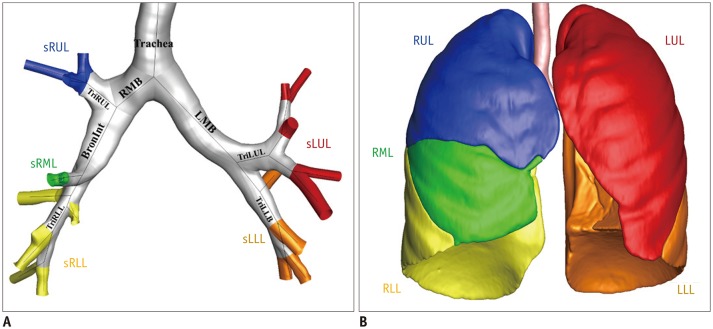
Fig. 3
Distribution of ΔVair* (A, B), and fSAD in Korean (left column) and White female (right column) samples (C, D).
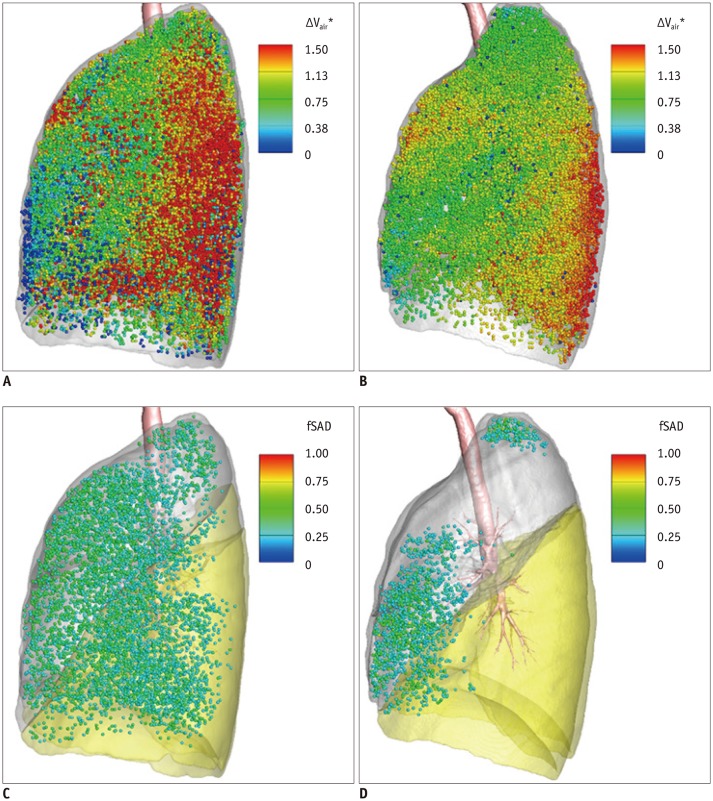
Table 1
Demographic and PFT Information of Koreans and Whites
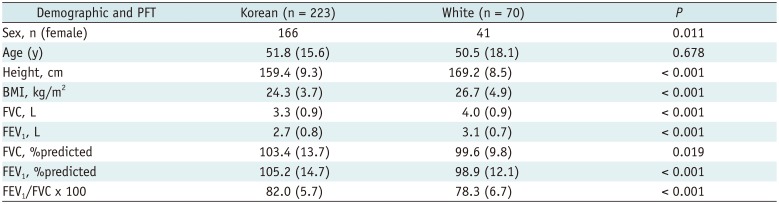
Table 2
Comparison of PFT Information and Functional Variables between Korean Male Subjects and White Male Subjects
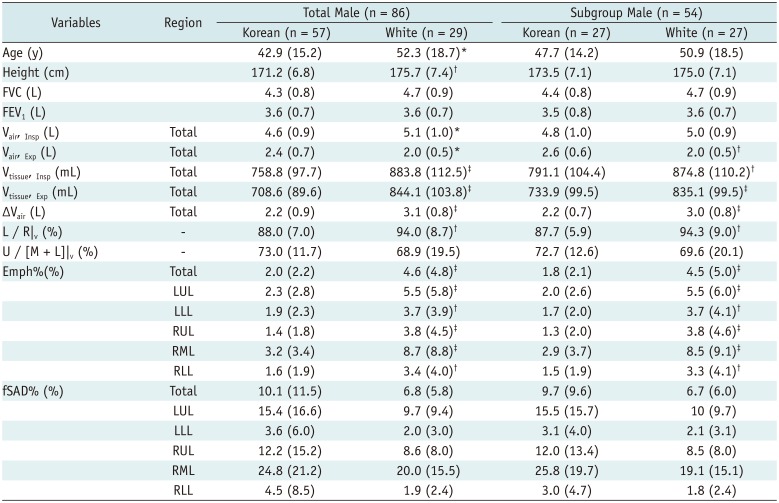
Values are presented as mean (SD). *p < 0.05, †p < 0.01, ‡p < 0.001. Emph% = percent emphysema-like lung, fSAD% = percent functional small airway disease-like lung, LLL = left lower lobe, L / R|v = ratio of air volume changes in left to those in right lobes, LUL = left upper lobe, RLL = right lower lobe, RML = right middle lobe, RUL = right upper lobe, U / [M + L]|v = ratio of air volume changes at upper lobes to those at middle and lower lobes, Vair, Exp = air volume at expiration, Vair, Insp = air volume at inspiration, Vtissue, Exp = tissue volume at expiration, Vtissue, Insp = tissue volume at inspiration, ΔVair = total air volume change in lung
Table 3
Comparison of PFT Information and Functional Variables between Korean Female Subjects and White Female Subjects
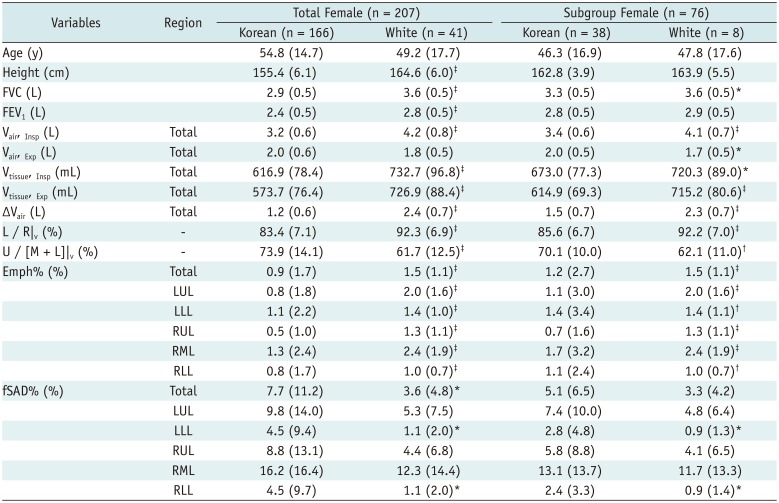
Table 4
Comparison of Structural Variables between Korean Male Subjects and White Male Subjects
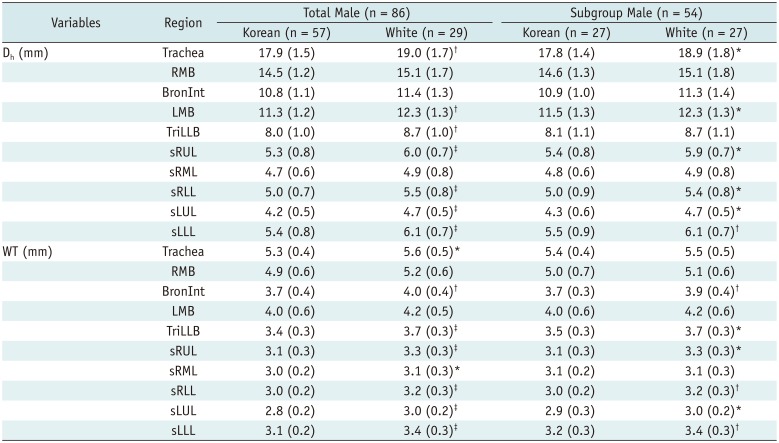
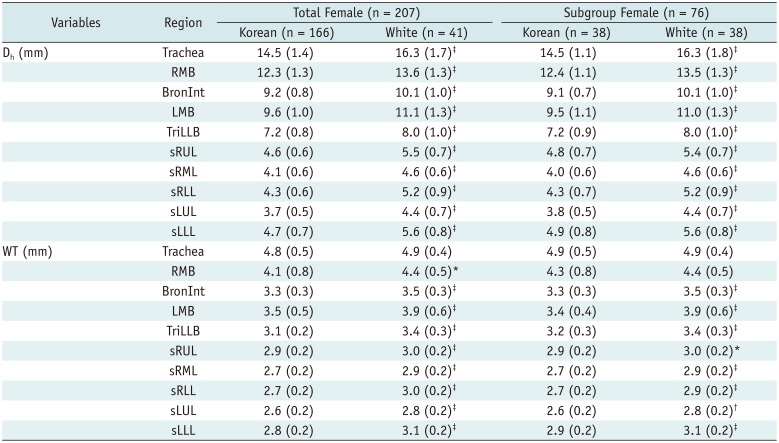
Values are presented as mean (SD). *p < 0.05, †p < 0.01, ‡p < 0.001. BronInt = bronchus intermedius, Dh = hydraulic diameter, LMB = left main bronchus, RMB = right main bronchus, sLLL = subgrouped LLL including branches of LB6 and LB8 to LB10, sLUL = subgrouped LUL including branches of LB1 to LB5, sRLL = subgrouped RLL including branches of RB6 to RB10, sRML = subgrouped RML including branches of RB4 and RB5, sRUL = subgrouped RUL including branches of RB1 to RB3, TriLLB = trifurcation of left lower bronohus, WT = wall thickness
Table 5
Comparison of Structural Variables between Korean Female Subjects and White Female Subjects




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download