Abstract
Purpose
To evaluate the categories of nocturia and relationships with the international prostate symptom score (IPSS) in Korean men with lower urinary tract symptoms (LUTS) accompanying nocturia.
Materials and Methods
Five hundred twenty-one male patients from five different hospitals, aged ≥18 years, were included. The 3-day frequency volume chart was used to identify nocturia. We also used the IPSS and The International Consultation on Incontinence Modular Questionnaire-Nocturia (ICIQ-N) module to verify the correlation between nocturia and quality of life.
Results
The distribution of nocturia events varied from 1 to 11, and 2 nocturia events were most prevalent (48.4%). Across the various numbers of nocturia events, the mean age, first sleep period, functional bladder capacity (FBC), nocturnal polyuria index (NPI), nocturia index (NI), predicted number of nightly voids, and nocturnal bladder capacity index (NBCI) were statistically different. Patients with pure nocturnal polyuria showed different night lengths, nocturnal urine volume, FBC, NPI, NI, and predicted number of nightly voids than those without nocturnal polyuria. Patients with severely reduced NBCI were prominent in the IPSS >20 group, and the degree of vexation increased with the number of nocturia events. The IPSS storage symptom score and ICIQ-N symptom score positively correlated with nocturia events.
Nocturia is the condition when an individual has to wake at night one or more times for voiding [1]. Its causes are varied, and in many patients, its cause is difficult to discern. Nocturia is associated with ageing, behavioral influences (e.g., late-night fluid intake and consumption of caffeine) or several medical conditions (e.g., diabetes, congestive heart failure, lower urinary tract obstruction, prostatic disease, and overactive bladder) [2]. Although nocturia can occur at any age, it is more common among older adults, and was the most commonly reported storage symptom for both men and women in five European countries [3]. The overall prevalence rates for nocturia range from 10.8% to 25% in men and increase with age [45], and the most frequent concern regarding nocturia in elderly individuals is that rising at night to urinate could induce traumatic falls that lead to prolonged morbidity [6]. Additionally, Shao et al. [7] reported that nocturia plays an important role in patients younger than 65 years of age in daytime dysfunction, which should not be overlooked.
Because nocturia affects a significant proportion of adults and has a detrimental effect on health-related quality of life, the impact, cause, and result of lower urinary tract symptoms (LUTS) and nocturia have been widely studied in North America and Europe [8]. In Japan, Yoshimura et al. [9] reported that benign prostate hyperplasia was an independent positive risk factor for nocturia. However, in Korea, few studies have evaluated nocturia, especially with the frequency volume chart and international prostate symptom score (IPSS) in men. The frequency volume chart is a simple but essential for measuring the outcomes in clinical trials of interventions for LUTS [10]. A 3-consecutiveday chart is widely used to assess patients' voiding patterns.
In an effort to collect cornerstone data for treatment of nocturia in Korean men, the present study was conducted to assess the categories of nocturia by analyzing the frequency volume chart in male patients with LUTS accompanying nocturia one or more times a day and relationships with IPSS in Korean men.
The observational, multicenter study protocol was approved by the Institutional Review Board and Medical Ethics Committee of The Catholic University of Korea (approval number: XC11OIMI0150O). All patients provided informed consent before participating in the study.
Patients aged 18 years and older who visited five different university hospitals in Korea because of LUTS with one or more nighttime voiding were included in this study. Patients with neurogenic bladder, diabetes insipidus, urinary tract symptoms related with spinal injury or surgery, and those taking an alpha blocker, anticholinergics, and 5-androgen receptor inhibitor were excluded.
The primary endpoint of this study was to acquire the baseline data in bothersome nocturia through assessment of the 3-days frequency volume chart. The secondary endpoint was to determine relationships between nocturia and the IPSS and The International Consultation on Incontinence Modular Questionnaire-Nocturia (ICIQ-N) score.
From the included patients, completed 3-day frequency volume charts and the IPSS were analyzed. The total urine volume (TUV), nocturnal urine volume (NUV), and functional bladder capacity (FBC) were reviewed from the frequency volume charts. Twenty-four-hour polyuria was defined as a total voiding volume exceeding 2.8 liters per day. Nocturnal polyuria was defined as NUV/TUV >0.2 in patients aged 18 to 49 years, NUV/TUV of 0.2 to 0.33 in those aged 18–49, 50–64, ≥65 years, and NUV/TUV >0.33 in those older than 65 years of age. Reduced nocturnal bladder capacity or nocturnal bladder overactivity was defined as a nocturnal bladder capacity index (NBCI) >0. The IPSS was used simultaneously to determine the patients' prostate symptoms and relationships with nocturia. We used the ICIQ-N module to evaluate the correlation between nocturia and quality of life.
The frequency volume chart and IPSS of all patients were analyzed for patterns of nocturia according to the number of nocturia events per night, and patients were classified into four groups (24-hour polyuria, nocturnal polyuria, reduced NBCI, and mixed type). Furthermore, these data were compared with the IPSS and ICIQ-N.
The sample size was calculated based on prevalence— 53.7% for male patients with LUTS in Korea and 30% to 35% for patients with nocturia according to the Korea expanded prostate cancer index composite (EPIC) study [11]. Mean and frequencies are used as descriptive parameters. The Pearson chi-square test was used to compare the categorical variables, Student t-test was used to analyze two continuous variables, and analysis of variance was used to analyze more than two continuous variables. A p-value <0.05 was considered statistically significant. All statistical analyses were conducted with SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Five hundred twenty-one patients from five different hospitals were included in this study.
The distribution of nocturia episodes varied from 1 to 11. Two nocturia events were most prevalent (48.4%), followed by 1 event (25.7%), 3 events (18.4%), and 4 events (5.4%) (Fig. 1).
When dividing those patients into groups according to the number of nocturia events (nocturia events <2, 2 nocturia events, and nocturia events >2), there were no differences in height, weight, body mass index, systolic blood pressure, diastolic blood pressure, and pulse rate among the groups. The mean age, first sleep period (period from sleep until waking for the first nocturia), void at the time of waking after sleep (first sleep period), FBC, nocturnal polyuria index (NPI), nocturia index (NI), predicted number of nightly voids, and NBCI were statistically different among the groups (Table 1).
Forty-five patients (8.6%) had polyuria, and there were no differences in epidemiologic characteristics among these patients. However, the first void at the time of waking after the sleep period and FBC were lower in patients with polyuria than in those without polyuria (Table 2). Three hundred seventy-six patients (72.2%) had nocturnal polyuria, and the night length, NUV, FBC, NPI, NI, and predicted numbers of nightly voids were different between the groups (Table 3). Five hundred twenty patients (99.8%) showed a reduced NBCI. There was only 1 exceptional patient in this evaluation, so the reduced NBCI showed no statistical importance in all variables. Three hundred seventy-six patients (72.2%) were mixed type, and 145 patients were non-mixed type; the night length, NUV, FBC, NPI, NI, and predicted numbers of nightly voids were different between these two groups (Table 4).
When dividing those patients into 4 groups by age (<50, 50–59, 60–69, ≥70 years), 24-hour polyuria showed the highest prevalence in the 60- to 69-year-old group. Nocturnal polyuria and mixed type showed the highest prevalence in patients older than 70 years of age. In patients younger than 50 years of age, severely reduced NBCI was the prominently observed symptom of nocturia (Table 5).
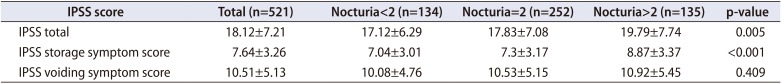
The IPSS was analyzed according to the number of nocturia events (<2, 2, and >2). The subtotal storage symptom score (IPSS 2+4+7) was statistically different among the groups; however, there was no difference in the voiding symptom score (IPSS 1+3+5+6) (Table 6).
According to the severity of the IPSS, we divided patients into the IPSS <8, 8≤IPSS<20, and IPSS ≥20 groups. The prevalence values for polyuria, nocturnal polyuria, reduced NBCI, and mixed nocturnal polyuria in the 8≤IPSS<20 group were high. The severely reduced NBCI was the most prevalent in the IPSS ≥20 group. A shorter first sleep period (p=0.003), small FBC (p<0.001), high NI (p=0.002), and predicted number of nightly voids (p=0.002) were observed in the IPSS ≥20 group. The IPSS total symptom score, storage symptom score (p<0.001), and voiding symptom score (p<0.001) were statistically different between the groups.
Nocturia is the most bothersome of all LUTS, and it is most strongly associated with reduced quality of life, as evaluated by health-related quality of life questionnaire [12131415]. The International Continence Society defines nocturia as the condition when an individual must wake at night one or more times to void. Two or more episodes are generally considered as being clinically significant, as this threshold is the one that is associated with reduced quality of life [16]. Because of the clinical impact of nocturia, the classification, prevalence, therapeutic modalities, and outcomes have been widely studied in Western countries. However, little is known about nocturia in East Asian countries including Korea [917]. The problem is that most elderly individuals consider nocturia as a normal part of the ageing process that does not need treatment. Moreover, a very small proportion of patients with nocturia have sought medical care [18], and only 63% of them were offered treatment because physicians are still unfamiliar or concerned about the impact of nocturia [11].
In this study, we observed many distinctive results. The baseline characteristics showed that age and nocturia have a strong positive correlation, as Wang et al. [17] reported. Additionally, the first sleep period and FBC decreased with age and nocturia events. Overall, 71.2% of patients had nocturnal polyuria, and all their voiding parameters were different from those of patients without nocturnal polyuria, except the NBCI. These data were consistent with those of Matthiesen et al.' s study [19] and Weiss et al.'s report [2] that nocturnal polyuria was a significant component of nocturia in 43% of patients, most of whom had reduced NBC.
When considering the relationships of the frequency volume chart with IPSS, each IPSS questionnaire (2, 4, and 7) and subtotal storage symptom scores were correlated with the number of nocturia events. Moreover, we observed a reduced NBCI more in the group with a severe IPSS.
The ICIQ-N is a simple diagnostic tool that can measure the burden caused by the frequency of daytime and nighttime voiding. Eckhardt et al. [20] reported that nocturia was one of the most bothersome symptoms in male patients with LUTS, and our data measured by the ICIQ-N was consistent with their finding. Furthermore, our study showed that nocturia was the prominent bothersome factor for sleep quality.
The LUTS assessment with questionnaires can be affected by recall bias. In the real-time clinical setting, a difference or poor correlation between the 3-day frequency volume chart and patient's perception can be easily observed. Thus, the real-time completion of documentation is important to obtain accurate voiding function and reduce recall bias. Although the frequency volume chart cannot replace a urodynamic study, it is crucial for recognizing the condition of a patient's bladder function.
This study has a couple limitations. Comorbidities such as cardiovascular disease, central nervous system disease, peripheral edema or hypertension, and diabetes mellitus were not considered. Additionally, we could only identify the characteristics of patients in some areas of the country; thus, the enrolled patients who visited the tertiary hospitals do not represent the general population. Despite those limitations, the number of study subjects was sufficient to represent general baseline populational data. Further nationwide study is needed to collect and analyze data of nocturia in Korea.
Nocturia has a wide etiology, and it has a crucial impact on quality of life. Despite the importance of nocturia, the prevalence and classification of nocturia in Korea is still lacking. This is the first large multicenter study of Korean male patients with LUTS and nocturia that assessed the frequency volume chart, IPSS, and ICIQ-N. Our data showed that in Korean male LUTS patients with nocturia, the mixed type of nocturia was prominent, and patients with a higher IPSS showed much lower sleep quality than those with a lower IPSS. Korean male nocturia patients with LUTS also have a reduced NBCI. In addition, we found that the first sleep period and FBC are negatively correlated with nocturia, whereas the IPSS and ICIQ-N are positively correlated with nocturia. The nocturia score of the IPSS could be a predictive factor for a high total IPSS, high storage score, and poor sleep quality. This manuscript provides concrete evidence that proper nocturia managements with reduced nocturnal bladder capacity and nocturnal polyuria could improve patients' quality of life as well as sleep quality.
References
1. van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, et al. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:179–183. PMID: 11857672.

2. Weiss JP, Blaivas JG, Stember DS, Brooks MM. Nocturia in adults: etiology and classification. Neurourol Urodyn. 1998; 17:467–472. PMID: 9776009.

3. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314. discussion 1314–5. PMID: 17049716.

4. Muscatello DJ, Rissel C, Szonyi G. Urinary symptoms and incontinence in an urban community: prevalence and associated factors in older men and women. Intern Med J. 2001; 31:151–160. PMID: 11478344.

5. Schatzl G, Temml C, Schmidbauer J, Dolezal B, Haidinger G, Madersbacher S. Cross-sectional study of nocturia in both sexes: analysis of a voluntary health screening project. Urology. 2000; 56:71–75. PMID: 10869627.

6. Stewart RB, Moore MT, May FE, Marks RG, Hale WE. Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc. 1992; 40:1217–1220. PMID: 1447437.

7. Shao IH, Wu CC, Hsu HS, Chang SC, Wang HH, Chuang HC, et al. The effect of nocturia on sleep quality and daytime function in patients with lower urinary tract symptoms: a crosssectional study. Clin Interv Aging. 2016; 11:879–885. PMID: 27418814.
8. Chapple C, Castro-Diaz D, Chuang YC, Lee KS, Liao L, Liu SP, et al. Prevalence of lower urinary tract symptoms in China, Taiwan, and South Korea: results from a cross-sectional, population-based study. Adv Ther. 2017; 34:1953–1965. PMID: 28687936.

9. Yoshimura K, Terada N, Matsui Y, Terai A, Kinukawa N, Arai Y. Prevalence of and risk factors for nocturia: analysis of a health screening program. Int J Urol. 2004; 11:282–287. PMID: 15147543.

10. Bright E, Drake MJ, Abrams P. Urinary diaries: evidence for the development and validation of diary content, format, and duration. Neurourol Urodyn. 2011; 30:348–352. PMID: 21284023.

11. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011; 29:185–190. PMID: 19898824.

12. Agarwal A, Eryuzlu LN, Cartwright R, Thorlund K, Tammela TL, Guyatt GH, et al. What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women? Eur Urol. 2014; 65:1211–1217. PMID: 24486308.

13. Zhang L, Zhu L, Xu T, Lang J, Li Z, Gong J, et al. A populationbased survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. Eur Urol. 2015; 68:97–112. PMID: 25572826.

14. Miranda Ede P, Gomes CM, Torricelli FC, de Bessa J Júnior, de Castro JE, Ferreira BR, et al. Nocturia is the lower urinary tract symptom with greatest impact on quality of life of men from a community setting. Int Neurourol J. 2014; 18:86–90. PMID: 24987561.

15. Dani H, Esdaille A, Weiss JP. Nocturia: aetiology and treatment in adults. Nat Rev Urol. 2016; 13:573–583. PMID: 27455894.

16. Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E. The prevalence of nocturia and its effect on healthrelated quality of life and sleep in a community sample in the USA. BJU Int. 2003; 92:948–954. PMID: 14632853.

17. Wang Y, Hu H, Xu K, Wang X, Na Y, Kang X. Prevalence, risk factors and the bother of lower urinary tract symptoms in China: a population-based survey. Int Urogynecol J. 2015; 26:911–919. PMID: 25653032.

18. Choo MS, Ku JH, Park CH, Lee YS, Lee KS, Lee JG, et al. Prevalence of nocturia in a Korean population aged 40 to 89 years. Neurourol Urodyn. 2008; 27:60–64. PMID: 17565726.

19. Matthiesen TB, Rittig S, Nørgaard JP, Pedersen EB, Djurhuus JC. Nocturnal polyuria and natriuresis in male patients with nocturia and lower urinary tract symptoms. J Urol. 1996; 156:1292–1299. PMID: 8808857.

20. Eckhardt MD, van Venrooij GE, van Melick HH, Boon TA. Prevalence and bothersomeness of lower urinary tract symptoms in benign prostatic hyperplasia and their impact on well-being. J Urol. 2001; 166:563–568. PMID: 11458069.

Fig. 1
Distribution of nocturia episodes of 521 patients. The distribution of nocturia episode varies from 1 to 11. The most prevalent episode is 2 (48.4%), and 1 (25.7%), 3 (18.4%), 4 events (5.4%) respectively.
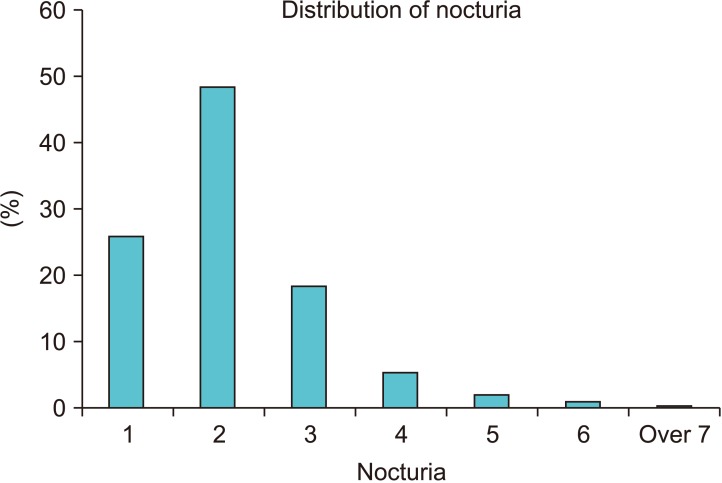
Table 1
Results of variables associated with nocturia by analyzing frequency volume chart according to the frequency of nocturia
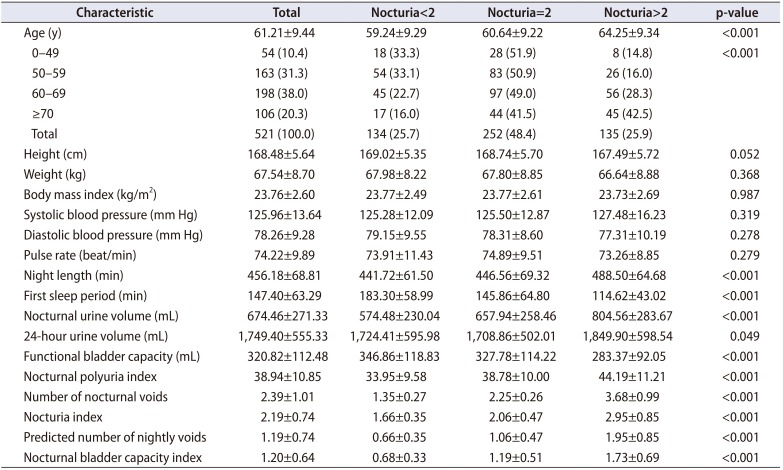
Table 2
Comparison of variables associated with nocturia between 24-hour polyuria and non-polyuria (most variables associated with nocturia were high in 24-hour polyuria group)
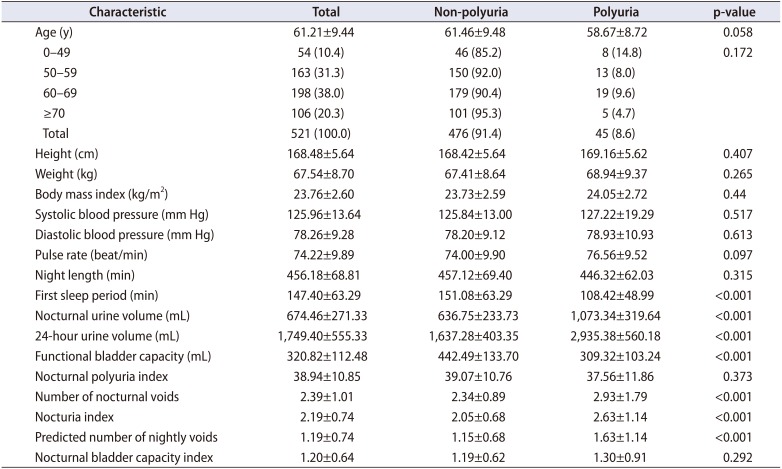
Table 3
Comparison of variables associated with nocturia between non- nocturnal and nocturnal polyuria (most variables associated with nocturia except NBCI were high in nocturnal polyuria group)
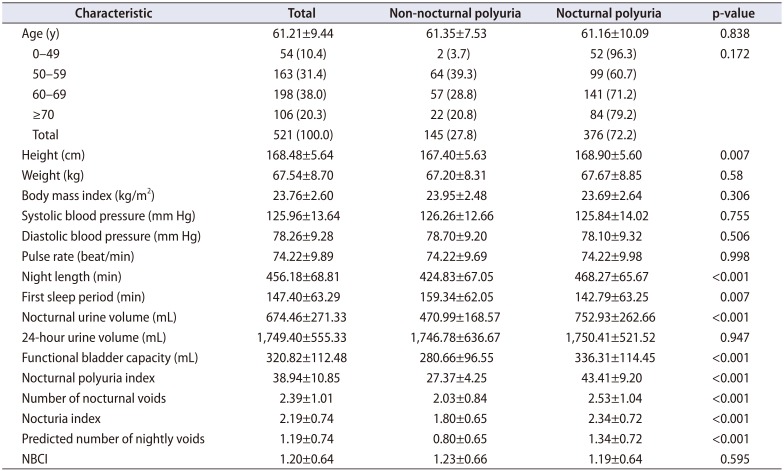
Table 4
Comparison of variables associated with nocturia between non-mixed and mixed types of nocturia (most variables associated with nocturia except NBCI were high in mixed type)
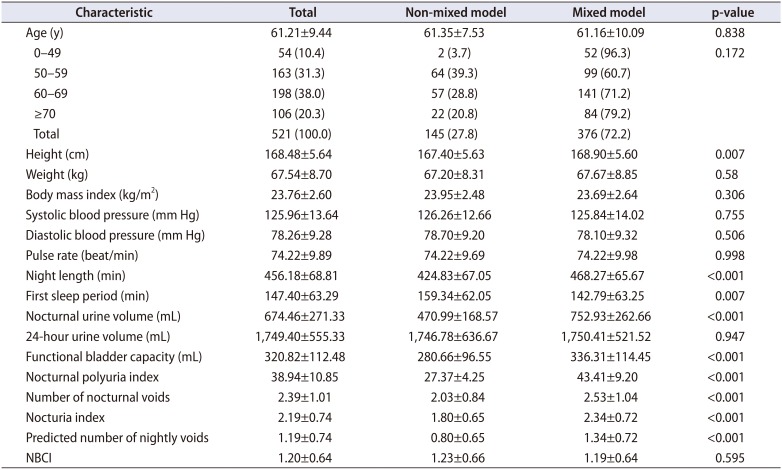
Table 5
Comparison of factors associated with nocturia depending on age (<50, 50–59, 60–69, and ≥70 years) (most variables were high in patients over 70 years old)
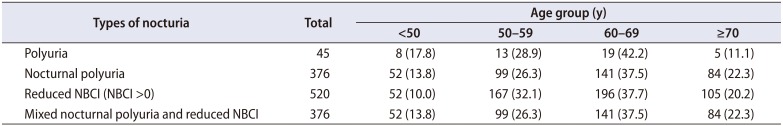
Table 6
Distribution of IPSS questionnaire according to frequency of nocturia (IPSS storage symptom score was high when the number of nocturia was increased)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download