Noro Viruses (NoV), a single-stranded RNA virus in the geunus
Norovirus of the
Caliciviridae family, is one of the major pathogens causing outbreaks of acute gastroenteritis [
1]. NoV infections have been known as a short self-limiting disease with sudden onset of abdominal discomfort, nausea, vomiting and diarrhea; however, it also causes poor clinical outcome for those having underlying diseases or aged [
2]. NoV is highly contagious, stable outside of the host and the lack of long-lasting immunity of the host; thus, it usually results in high attack rate [
34].
It is well-established that NoV can be transmitted from an affected individual (via the fecal to oral route), from contaminated food, through contaminated airborne droplets, and through contact with contaminated environments surfaces [
45]. To our knowledge, there have been lack of studies in Korea specifically addressing infection control measure of the NoV outbreak transmitted from human to human. Therefore, the purpose of this study is to demonstrate the norovirus outbreak which is likely spread by human to human infection.
On January 5, 2018, a staff at a kindergarten was reported to the public health authority that several children presented with vomiting. An outbreak investigation was implemented to identify the possible source of infection and the route of transmission, and recommend appropriate control measures.
Ethical approval for this study was not required under the Korean Infectious Disease Control and Prevention Act No. 4 and the Enforcement Rule of Bioethics and Safety Act No. 33.
A case was defined as a kindergartener presented vomiting or diarrhea more than twice between the period January 1, 2018 (three days before the first case's symptoms presented) and January 5, 2018. A laboratory-confirmed case was defined as a case who had tested positive on laboratory test confirming the presence of NoV.
Data on demographic factors was collected using interview included sex and the class name attended in the kindergarten. To measure the risk of case development among children ate lunch between 2nd and 3rd of January 2018, kindergarteners were interviewed using questionnaires of lunch menu by public health officers. Furthermore, to assess the level of environmental contamination, environmental swabs were taken from the doorknob of classrooms named “Fruit” and “Leaf”, and toilet in the kindergarten.
Rectal swabs were taken from six of fifteen cases and a food handler during the investigation. All the preserved food cooked in the kindergarten, water sample, swabs from six cases and a food handler and environments were transported to the provincial public health laboratory to identify the presence of bacteria (
Salmonella spp.,
Shigella spp., Enterohemorrhagic
Escherichia coli, Enterotoxigenic
Escherichia coli, Enteropathogenic
Escherichia coli, Enteroaggregative
Escherichia coli, Enteroinvasive
Escherichia coli,
Vibrio phaemolyticus,
Campylobacter jejuni,
Staphylococcus aureus,
Clostridium perfringens,
Bacillus cereus,
Yersinia enterocolitica, and
Listeria monocytogenes) and viruses (Group A Rotavirus, Astrovirus, Enteric adenovirus, Norovirus, and Sapoviruss). To detect the NoV, Real-time Reverse Transcription Polymerase Chain Reaction testing targeted genes coding for ORF1-ORF2 junction region was conducted as which described elsewhere [
67].
The overall attack rate was calculated by dividing the total number of case by the total number of children in the kindergarten. Fisher's exact test was used to assess the significant differences in demographic factors and food in the lunch between case and non-case. Epi-info 7 (Centers for Disease Control and Prevention, United States) was used for all statistical analyses, and a P-value ≤0.05 was considered statistically significant.
The kindergarten includes 48 children with five classrooms (class name: Fruit, Leaf, Sun, Petal and Sprout) in a single floor (
Fig. 1). The only food they consumed was lunch which was cooked in a kindergarten and delivered to each classroom at lunch.
A total of 48 children were enrolled in this study. Fifteen children were identified as cases, and the overall attack rate was 31.3%. Among the 15 cases, seven (47%) were boys and the mean age was 2.7 years (range 1–3 years).
The first case in a class “Fruit” presented with a vomiting at 3:30 AM on January 3, 2018, in her house and then another child in the same classroom presented vomiting at 17:00 PM.
The epidemic curve comprised of a peak between 21:30 PM on January 3, 2018 and 3:30 AM on January 4, 2018 with eight cases and no additional cases were reported after 5:00 AM on January 4, 2018. (
Fig. 2). Reported symptoms of cases were a vomiting (15 cases; 100% of total cases), fever (three cases; 20%), abdominal pain (two cases; 13%), and diarrhea (one case; 7%). All cases were improved after conservative management through outpatient clinics.
NoV was not isolated from the specimen of the food, environments and a food handler.
However, among six cases who conducted laboratory tests, four were confirmed to be Group II, NoroV positive.
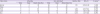
On the analysis of attack rate by classrooms, class named “Leaf” (63%) and “Fruit” (50%) had relatively higher attack rate than class “Sprout” (33%), “Sun” (17%) and “Petal” (0%) (
Table 1). We did not identify the difference of case-development by sex. Furthermore, we did not find significant difference among the menus of food between the cases and non-cases.
On January 5, 2018, cases were recommended to be isolated from others by the day of disappearing their symptoms and environmental cleaning with disinfectants including alcohol and chlorine was implemented as a measure to control this outbreak. Furthermore, monitoring of any abnormal symptoms of children were implemented by the four days after the last case identified.
From our results, although we cannot be certain whether the source of infection was environmental, or shedding of virus from index cases, this outbreak of NoV genogroup II is likely originated from the index case and transmitted to others in the same classroom and adjacent classrooms in the kindergarten. There are three reasons following; first, only Group II NoV had been identified among cases and had not been identified from the food, a food handler and environment. Second, the children in class “Petal”, the most far-away classroom from the class “Fruit” where the index and second case developed, had not been identified any case. Third, the epidemic curve, which had a peak with a time interval of 13.5 hours between an index case and other clusters of cases, demonstrated the cases in the cluster were likely exposed to the index cases.
In our study, there was no significant difference between the sex of cases and the most frequently presented symptom of cases was vomiting. These findings were consistent with a previous study of NoV surveillance [
8].
Group II NoV caused the predominant cause of acute gastroenteritis in many countries (71.4% of NoV affected patients in Korea) [
910], and large portion of NoV outbreak caused by infected humans (64% in the US) [
11]. To date, high-profile of outbreaks of acute gastroenteric illness in Korea have focused on the food and water borne transmission, and led to serious efforts to assess and control the food contamination and food handlers [
12]. Based on the guidelines published in the US, the measure of infection control includes discarding exposed materials from vomiting and environmental decontamination all the surface areas within at least a 25-foot radius of the vomiting site with temporary closure of the area where vomiting incidence occurred and the toilet in the facility until the contaminated area is properly disinfected with bleach solution [
1]. Therefore, additional study to control NoV outbreak should be considered for the appropriateness of environmental disinfection of the area where NoV affected patient resided to prevent a large number of cases during outbreaks in Korea.
There are several limitations to this study. First, sequencing of NoV identified in this outbreak was not conducted to determine whether the NoV genotype II strains were identical. However, regarding the clusters of cases during a short period of time, they were most likely affected by an identical strain. Second, in a time- and resource-limited setting, the non-symptomatic children were not tested for NoV infection by laboratory tests. Previous study has demonstrated that up to 30% of NoV infection was not presenting symptoms with possibility of shedding virus; however, asymptomatic infection has lower titers of virus than symptomatic [
13]. Third, there may be recall bias by the parents and children due to the delay in conducting interviews. However, we interviewed the staffs in an attempt to correct any bias.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download