1. Wachter RM, Goldman L. Zero to 50,000 - The 20th anniversary of the hospitalist. N Engl J Med. 2016; 375(11):1009–1011.

2. Shu CC, Lin JW, Lin YF, Hsu NC, Ko WJ. Evaluating the performance of a hospitalist system in Taiwan: a pioneer study for nationwide health insurance in Asia. J Hosp Med. 2011; 6(7):378–382.

3. Kisuule F, Howell E. Hospital medicine beyond the United States. Int J Gen Med. 2018; 11:65–71.

4. Meltzer D, Manning WG, Morrison J, Shah MN, Jin L, Guth T, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002; 137(11):866–874.

5. Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002; 137(11):859–865.

6. Bellet PS, Whitaker RC. Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges. Pediatrics. 2000; 105(3 Pt 1):478–484.

7. Howrey BT, Kuo YF, Goodwin JS. Association of care by hospitalists on discharge destination and 30-day outcomes after acute ischemic stroke. Med Care. 2011; 49(8):701–707.

8. Tadros RO, Faries PL, Malik R, Vouyouka AG, Ting W, Dunn A, et al. The effect of a hospitalist comanagement service on vascular surgery inpatients. J Vasc Surg. 2015; 61(6):1550–1555.

9. Landefeld CS. Care of hospitalized older patients: opportunities for hospital-based physicians. J Hosp Med. 2006; 1(1):42–47.

10. Jang SI, Jang SY, Park EC. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med. 2015; 89(1):1–5.

11. Eom JS. Operating the hospitalist system. J Korean Med Assoc. 2016; 59(5):342–344.

12. Lee DK. Launching the hospitalist in Korea. Korean J Med. 2016; 91(3):241–244.

13. Kim HW. The current status of hospital medicine in Korea, 2019. Korean J Med. 2019; 94(2):139–144.

14. Ohn JH, Kim NH, Kim ES, Baek SH, Lim Y, Hur J, et al. An Acute medical unit in a Korean tertiary care hospital reduces the length of stay and waiting time in the emergency department. J Korean Med Sci. 2017; 32(12):1917–1920.

15. Weng TC, Huang CC, Zhang CC, Huang HK, Wu MC, Wsu CC. Application of integrated medical care model (hospitalist) in emergency department and its efficiency and outcome: 4 years' experience in Taiwan. Health Care Curr Rev. 2017; 5(4):211–216.

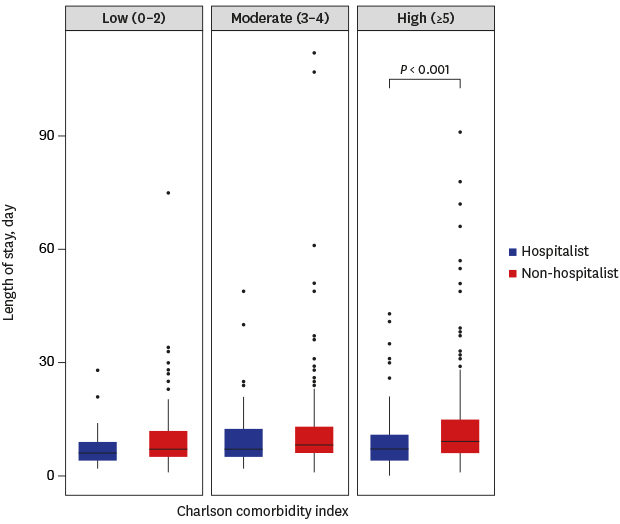
16. Matsui K, Goldman L, Johnson PA, Kuntz KM, Cook EF, Lee TH. Comorbidity as a correlate of length of stay for hospitalized patients with acute chest pain. J Gen Intern Med. 1996; 11(5):262–268.

17. Rosenthal GE, Harper DL, Quinn LM, Cooper GS. Severity-adjusted mortality and length of stay in teaching and nonteaching hospitals. Results of a regional study. JAMA. 1997; 278(6):485–490.
18. Ofori-Asenso R, Zomer E, Chin KL, Si S, Markey P, Tacey M, et al. Effect of comorbidity assessed by the Charlson comorbidity index on the length of stay, costs and mortality among older adults hospitalised for acute stroke. Int J Environ Res Public Health. 2018; 15(11):E2532.

19. Hijazi HH, Alyahya MS, Hammouri HM, Alshraideh HA. Risk assessment of comorbidities on 30-day avoidable hospital readmissions among internal medicine patients. J Eval Clin Pract. 2017; 23(2):391–401.

20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383.

21. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; 173(6):676–682.

22. Stavem K, Hoel H, Skjaker SA, Haagensen R. Charlson comorbidity index derived from chart review or administrative data: agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017; 9:311–320.

23. Yang Y, Yang KS, Hsann YM, Lim V, Ong BC. The effect of comorbidity and age on hospital mortality and length of stay in patients with sepsis. J Crit Care. 2010; 25(3):398–405.

24. Shapiro NI, Howell MD, Talmor D, Donnino M, Ngo L, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score predicts 1-year mortality. Crit Care Med. 2007; 35(1):192–198.

25. Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003; 31(3):670–675.

26. Williams JM, Greenslade JH, Chu K, Brown AF, Lipman J. Severity scores in emergency department patients with presumed infection: a prospective validation study. Crit Care Med. 2016; 44(3):539–547.
27. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315(8):801–810.

28. Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003; 58(5):377–382.

29. Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011; 6(3):115–121.

30. Feng C, Wang H, Lu N, Tu XM. Log transformation: application and interpretation in biomedical research. Stat Med. 2013; 32(2):230–239.

31. Health Insurance Review & Assessment Service. Hospital Average Length of Stay by Diagnostic Categories in 2017 and 2018. Indicator Status. Wonju: Health Insurance Review & Assessment Service;2019.
32. Rachoin JS, Skaf J, Cerceo E, Fitzpatrick E, Milcarek B, Kupersmith E, et al. The impact of hospitalists on length of stay and costs: systematic review and meta-analysis. Am J Manag Care. 2012; 18(1):e23–e30.
33. Kuo YF, Goodwin JS. Effect of hospitalists on length of stay in the medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010; 58(9):1649–1657.

34. Southern WN, Berger MA, Bellin EY, Hailpern SM, Arnsten JH. Hospitalist care and length of stay in patients requiring complex discharge planning and close clinical monitoring. Arch Intern Med. 2007; 167(17):1869–1874.

35. Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007; 357(25):2589–2600.

36. Howell EE, Bessman ES, Rubin HR. Hospitalists and an innovative emergency department admission process. J Gen Intern Med. 2004; 19(3):266–268.

37. Freed DH. Hospitalists: Evolution, evidence, and eventualities. Health Care Manag (Frederick). 2004; 23(3):238–256.
38. Goodwin JS, Salameh H, Zhou J, Singh S, Kuo YF, Nattinger AB. Association of hospitalist years of experience with mortality in the hospitalized medicare population. JAMA Intern Med. 2018; 178(2):196–203.

39. Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011; 155(3):152–159.

40. Hamel MB, Drazen JM, Epstein AM. The growth of hospitalists and the changing face of primary care. N Engl J Med. 2009; 360(11):1141–1143.

41. Sharma G, Fletcher KE, Zhang D, Kuo YF, Freeman JL, Goodwin JS. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. JAMA. 2009; 301(16):1671–1680.

42. Bell CM, Schnipper JL, Auerbach AD, Kaboli PJ, Wetterneck TB, Gonzales DV, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009; 24(3):381–386.

43. Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003; 18(8):646–651.

44. Cabré M, Serra-Prat M, Force L, Almirall J, Palomera E, Clavé P. Oropharyngeal dysphagia is a risk factor for readmission for pneumonia in the very elderly persons: observational prospective study. J Gerontol A Biol Sci Med Sci. 2014; 69(3):330–337.
45. Tong L, Arnold T, Yang J, Tian X, Erdmann C, Esposito T. The association between outpatient follow-up visits and all-cause non-elective 30-day readmissions: a retrospective observational cohort study. PLoS One. 2018; 13(7):e0200691.

46. Burke RE, Ryan P. Postdischarge clinics: hospitalist attitudes and experiences. J Hosp Med. 2013; 8(10):578–581.

47. Mahant S, Weinstein M. Hospitalists and the outpatient clinic: time to reconsider. J Pediatr. 2016; 168:3–4.

48. Shu CC, Hsu NC, Lin YF, Wang JY, Lin JW, Ko WJ. Integrated postdischarge transitional care in a hospitalist system to improve discharge outcome: an experimental study. BMC Med. 2011; 9(1):96.









 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download