1. Avery ME, Mead J. Surface properties in relation to atelectasis and hyaline membrane disease. AMA J Dis Child. 1959; 97(5, Part 1):517–523.

2. Fujiwara T, Maeta H, Chida S, Morita T, Watabe Y, Abe T. Artificial surfactant therapy in hyaline-membrane disease. Lancet. 1980; 1(8159):55–59.

3. Obladen M. History of surfactant up to 1980. Biol Neonate. 2005; 87(4):308–316.

4. Halliday HL. Surfactants: past, present and future. J Perinatol. 2008; 28:Suppl 1. S47–S56.

5. Bae CW. The history of neonatology in Korea. J Korean Med Assoc. 2016; 59(7):490–497.

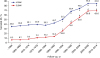
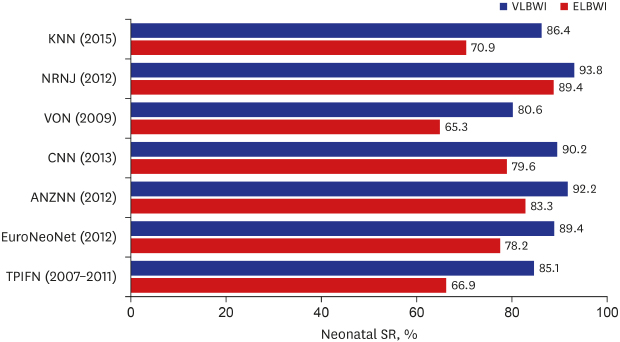
6. Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011; 26(4):467–473.

7. Choi JH. Milestones of the history of neonatal intensive care in Korea. Neonatal Med. 2013; 20(3):236–248.

8. Shim JW, Jin HS, Bae CW. Changes in survival rate for very-low-birth-weight infants in Korea: comparison with other countries. J Korean Med Sci. 2015; 30:Suppl 1. S25–S34.

9. Chung SH, Bae CW. Improvement in the survival rates of very low birth weight infants after the establishment of the Korean neonatal network: comparison between the 2000s and 2010s. J Korean Med Sci. 2017; 32(8):1228–1234.

10. Prange HD. Laplace's law and the alveolus: a misconception of anatomy and a misapplication of physics. Adv Physiol Educ. 2003; 27(1-4):34–40.

11. Neergaard K. Neue auffassungen über einen grundbegriff der atemmechanik. Z Gesamte Exp Med. 1929; 66(1):373–394.

12. Thannhauser SJ, Penotti J, Boncoddo NF. Isolation and properties of hydrolecithin (dipalmityl lecithin) from lung; its occurrence in the sphingomyelin fraction of animal tissues. J Biol Chem. 1946; 166(2):669–675.

13. Gruenwald P. Surface tension as a factor in the resistance of neonatal lungs to aeration. Am J Obstet Gynecol. 1947; 53(6):996–1007.

14. Clements JA. Dependence of pressure-volume characteristics of lungs on intrinsic surface active material. Am J Physiol. 1956; 187:592.
15. MacKlin CC. The pulmonary alveolar mucoid film and the pneumonocytes. Lancet. 1954; 266(6822):1099–1104.

16. Stevens TP, Sinkin RA. Surfactant replacement therapy. Chest. 2007; 131(5):1577–1582.

17. Chu J, Clements JA, Cotton EK, Klaus MH, Sweet AY, Tooley WH, et al. Neonatal pulmonary ischemia. I. Clinical and physiological studies. Pediatrics. 1967; 40(4):709–782.
18. Enhörning G, Robertson B. Lung expansion in the premature rabbit fetus after tracheal deposition of surfactant. Pediatrics. 1972; 50(1):58–66.
19. Adams FH, Towers B, Osher AB, Ikegami M, Fujiwara T, Nozaki M. Effects of tracheal instillation of natural surfactant in premature lambs. I. Clinical and autopsy findings. Pediatr Res. 1978; 12(8):841–848.

20. King RJ, Klass DJ, Gikas EG, Clements JA. Isolation of apoproteins from canine surface active material. Am J Physiol. 1973; 224(4):788–795.

21. Hallman M, Merritt TA, Schneider H, Epstein BL, Mannino F, Edwards DK, et al. Isolation of human surfactant from amniotic fluid and a pilot study of its efficacy in respiratory distress syndrome. Pediatrics. 1983; 71(4):473–482.
22. Wiseman LR, Bryson HM. Porcine-derived lung surfactant. A review of the therapeutic efficacy and clinical tolerability of a natural surfactant preparation (Curosurf) in neonatal respiratory distress syndrome. Drugs. 1994; 48(3):386–403.
23. Singh N, Halliday HL, Stevens TP, Suresh G, Soll R, Rojas-Reyes MX. Comparison of animal-derived surfactants for the prevention and treatment of respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2015; (12):CD010249.

24. Kattwinkel J. Surfactant. Evolving issues. Clin Perinatol. 1998; 25(1):17–32.

25. Robertson B, Halliday HL. Principles of surfactant replacement. Biochim Biophys Acta. 1998; 1408(2-3):346–361.

26. Almlén A, Walther FJ, Waring AJ, Robertson B, Johansson J, Curstedt T. Synthetic surfactant based on analogues of SP-B and SP-C is superior to single-peptide surfactants in ventilated premature rabbits. Neonatology. 2010; 98(1):91–99.

27. Cochrane CG, Revak SD, Merritt TA, Heldt GP, Hallman M, Cunningham MD, et al. The efficacy and safety of KL4-surfactant in preterm infants with respiratory distress syndrome. Am J Respir Crit Care Med. 1996; 153(1):404–410.

28. Häfner D, Germann PG, Hauschke D, Kilian U. Effects of early treatment with rSP-C surfactant on oxygenation and histology in rats with acute lung injury. Pulm Pharmacol Ther. 1999; 12(3):193–201.

29. The Korean Society of Neonatology. History of the Korean Society of Neonatology. Updated 2018. Accessed May 7, 2019.
http://www.neonatology.or.kr.
30. Bae CW, editor. The 20th Annual Celebration of the 20th Annual Conference of the Korean Society of Neonatology. 2013 Oct 19; Seoul. Seoul: Korean Society of Neonatology;c2013.
31. Namgung R, Lee C, Suh JS, Park KI, Han DG. Exogenous surfactant replacement therapy of hyaline membrane disease in premature infants. Yonsei Med J. 1989; 30(4):355–366.

32. Park CO, Lim BY, Yeo BG, Song JH, Sohn EK, Bae CW, et al. Surfactant replacement therapy in neonatal respiratory distress syndrome. J Korean Pediatr Soc. 1991; 34(9):1211–1222.
33. Bae CW, Kwon YD, Ko SJ, Kim KS, Kim HM, Park WS, et al. Surfactant replacement therapy in neonates with respiratory distress syndrome: a collective evaluation of trials from 16 hospitals. J Korean Pediatr Soc. 1993; 36(2):244–265.
34. Bae CW. Surfactant replacement therapy in RDS: a collaborative study of multi-center trials in Korea. J Korean Soc Neonatol. 1997; 4(1):124–135.
35. Bae CW, Kim YM. Surfactant therapy for neonatal respiratory distress syndrome: experience in Korea over 15 years. Korean J Pediatr. 2004; 47(9):940–948.
36. Bae CW, Hahn WH. Surfactant therapy for neonatal respiratory distress syndrome: a review of Korean experiences over 17 years. J Korean Med Sci. 2009; 24(6):1110–1118.

37. Bae CW, Hahn WH, Chang JY, Kim SM. Surfactant replacement therapy for RDS: a collaborative study of 72 multi-center trials in Korea (2010) and a review of Korean experiences over 20 years. J Korean Soc Neonatol. 2011; 18(2):409–411.

38. Kim SM, Park YJ, Chung SH, Choi YS, Kim CH, Bae CW. Early prophylactic versus late selective use of surfactant for respiratory distress syndrome in very preterm infants: a collaborative study of 53 multi-center trials in Korea. J Korean Med Sci. 2014; 29(8):1126–1131.

39. Niemarkt HJ, Hütten MC, Kramer BW. Surfactant for respiratory distress syndrome: new ideas on a familiar drug with innovative applications. Neonatology. 2017; 111(4):408–414.

40. Kribs A, Roll C, Göpel W, Wieg C, Groneck P, Laux R, et al. Nonintubated surfactant application vs conventional therapy in extremely preterm infants: a randomized clinical trial. JAMA Pediatr. 2015; 169(8):723–730.
41. Koh JW, Kim JW, Chang YP. Transient intubation for surfactant administration in the treatment of respiratory distress syndrome in extremely premature infants. Korean J Pediatr. 2018; 61(10):315–321.

42. Seo MY, Shim GH, Chey MJ. Clinical outcomes of minimally invasive surfactant therapy via tracheal catheterization in neonates with a gestational age of 30 weeks or more diagnosed with respiratory distress syndrome. Neonatal Med. 2018; 25(3):109–117.

43. Bae CW, Chung SH, Choi YS. Development of a synthetic surfactant using a surfactant protein-C peptide analog: in vitro studies of surface physical properties. Yonsei Med J. 2016; 57(1):203–208.

44. Choi YS, Chung SH, Bae CW. A combination of short and simple surfactant protein B and C analogues as a new synthetic surfactant: in vitro and animal experiments. Yonsei Med J. 2017; 58(4):823–828.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download