1. Whelton PK. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanisation. Lancet. 1994; 344(8915):101–106.
2. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA. 2017; 317(2):165–182.
3. Lauer RM, Burns TL, Clarke WR, Mahoney LT. Childhood predictors of future blood pressure. Hypertension. 1991; 18(3):Suppl. I74–I81.

4. Hait HI, Lemeshow S, Rosenman KD. A longitudinal study of blood pressure in a national survey of children. Am J Public Health. 1982; 72(11):1285–1287.

5. Suh I, Nam CM, Jee SH, Kim SI, Lee KH, Kim HC, et al. Twelve-year tracking of blood pressure in Korean school children: the Kangwha Study. Yonsei Med J. 1999; 40(4):383–387.

6. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008; 117(25):3171–3180.
7. Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007; 116(13):1488–1496.

8. Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988–2008. Hypertension. 2013; 62(2):247–254.
9. Bayazit AK, Yalcinkaya F, Cakar N, Duzova A, Bircan Z, Bakkaloglu A, et al. Reno-vascular hypertension in childhood: a nationwide survey. Pediatr Nephrol. 2007; 22(9):1327–1333.

10. Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003; 115(4):291–297.

11. Luyckx VA, Shukha K, Brenner BM. Low nephron number and its clinical consequences. Rambam Maimonides Med J. 2011; 2(4):e0061.
12. Brenner BM, Garcia DL, Anderson S. Glomeruli and blood pressure. Less of one, more the other? Am J Hypertens. 1988; 1(4 Pt 1):335–347.

13. Brenner BM, Anderson S. The interrelationships among filtration surface area, blood pressure, and chronic renal disease. J Cardiovasc Pharmacol. 1992; 19:Suppl 6. S1–S7.

14. White SL, Perkovic V, Cass A, Chang CL, Poulter NR, Spector T, et al. Is low birth weight an antecedent of CKD in later life? A systematic review of observational studies. Am J Kidney Dis. 2009; 54(2):248–261.

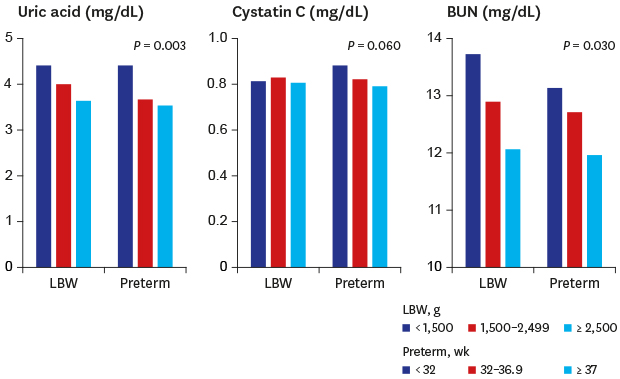
15. Park B, Lee HA, Lee SH, Park BM, Park EA, Kim HS, et al. Association between serum levels of uric acid and blood pressure tracking in childhood. Am J Hypertens. 2017; 30(7):713–718.

16. Park B, Park E, Cho SJ, Kim Y, Lee H, Min J, et al. The association between fetal and postnatal growth status and serum levels of uric acid in children at 3 years of age. Am J Hypertens. 2009; 22(4):403–408.

17. Lee HA, Park BH, Park EA, Cho SJ, Kim HS, Park H. Long-term effects of the SLC2A9 G844A and SLC22A12 C246T variants on serum uric acid concentrations in children. BMC Pediatr. 2018; 18(1):296.

18. Lee CG, Moon JS, Choi JM, Nam CM, Lee SY, Oh K, et al. Normative blood pressure references for Korean children and adolescents. Korean J Pediatr. 2008; 51(1):33–41.

19. Barker DJ, Bull AR, Osmond C, Simmonds SJ. Fetal and placental size and risk of hypertension in adult life. BMJ. 1990; 301(6746):259–262.

20. Barker DJ, Osmond C, Winter PD, Margetts B, Simmonds SJ. Weight in infancy and death from ischaemic heart disease. Lancet. 1989; 2(8663):577–580.

21. Baum M. Role of the kidney in the prenatal and early postnatal programming of hypertension. Am J Physiol Renal Physiol. 2010; 298(2):F235–F247.

22. Brenner BM, Chertow GM. Congenital oligonephropathy and the etiology of adult hypertension and progressive renal injury. Am J Kidney Dis. 1994; 23(2):171–175.

23. Luyckx VA. Preterm birth and its impact on renal health. Semin Nephrol. 2017; 37(4):311–319.

24. Saxén L, Sariola H. Early organogenesis of the kidney. Pediatr Nephrol. 1987; 1(3):385–392.

25. Dressler GR. The cellular basis of kidney development. Annu Rev Cell Dev Biol. 2006; 22(1):509–529.

26. Hughson M, Farris AB 3rd, Douglas-Denton R, Hoy WE, Bertram JF. Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int. 2003; 63(6):2113–2122.

27. Mañalich R, Reyes L, Herrera M, Melendi C, Fundora I. Relationship between weight at birth and the number and size of renal glomeruli in humans: a histomorphometric study. Kidney Int. 2000; 58(2):770–773.

28. Rodríguez MM, Gómez AH, Abitbol CL, Chandar JJ, Duara S, Zilleruelo GE. Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol. 2004; 7(1):17–25.

29. Feig DI, Nakagawa T, Karumanchi SA, Oliver WJ, Kang DH, Finch J, et al. Hypothesis: uric acid, nephron number, and the pathogenesis of essential hypertension. Kidney Int. 2004; 66(1):281–287.

30. Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008; 359(17):1811–1821.

31. Franco MC, Christofalo DM, Sawaya AL, Ajzen SA, Sesso R. Effects of low birth weight in 8- to 13-year-old children: implications in endothelial function and uric acid levels. Hypertension. 2006; 48(1):45–50.
32. Washburn LK, Nixon PA, Russell GB, Snively BM, O'Shea TM. Preterm birth is associated with higher uric acid levels in adolescents. J Pediatr. 2015; 167(1):76–80.

33. Kwinta P, Klimek M, Drozdz D, Grudzień A, Jagła M, Zasada M, et al. Assessment of long-term renal complications in extremely low birth weight children. Pediatr Nephrol. 2011; 26(7):1095–1103.

34. Frankfurt JA, Duncan AF, Heyne RJ, Rosenfeld CR. Renal function and systolic blood pressure in very-low-birth-weight infants 1–3 years of age. Pediatr Nephrol. 2012; 27(12):2285–2291.
35. Starzec K, Klimek M, Grudzień A, Jagła M, Kwinta P. Longitudinal assessment of renal size and function in extremely low birth weight children at 7 and 11 years of age. Pediatr Nephrol. 2016; 31(11):2119–2126.
36. Roggero P, Giannì ML, Morlacchi L, Piemontese P, Liotto N, Taroni F, et al. Blood urea nitrogen concentrations in low-birth-weight preterm infants during parenteral and enteral nutrition. J Pediatr Gastroenterol Nutr. 2010; 51(2):213–215.

37. Bloomfield GS, Yi SS, Astor BC, Kramer H, Shea S, Shlipak MG, et al. Blood pressure and chronic kidney disease progression in a multi-racial cohort: the Multi-Ethnic Study of Atherosclerosis. J Hum Hypertens. 2013; 27(7):421–426.

38. Rohani F, Hooman N, Moradi S, Mobarra M, Najafizadeh M, Tatarpoor P. The Prevalence of pre-hypertension in children with type 1 diabetes mellitus. Int J Prev Med. 2014; 5:Suppl 1). S44–9.
39. Wlodek ME, Mibus A, Tan A, Siebel AL, Owens JA, Moritz KM. Normal lactational environment restores nephron endowment and prevents hypertension after placental restriction in the rat. J Am Soc Nephrol. 2007; 18(6):1688–1696.

40. Wlodek ME, Westcott K, Siebel AL, Owens JA, Moritz KM. Growth restriction before or after birth reduces nephron number and increases blood pressure in male rats. Kidney Int. 2008; 74(2):187–195.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download