1. Lina TT, Alzahrani S, Gonzalez J, Pinchuk IV, Beswick EJ, Reyes VE. Immune evasion strategies used by Helicobacter pylori. World J Gastroenterol. 2014; 20:12753–12766.
2. Yee JK.
Helicobacter pylori colonization of the oral cavity: a milestone discovery. World J Gastroenterol. 2016; 22:641–648.

3. Krajden S, Fuksa M, Anderson J, Kempston J, Boccia A, Petrea C, et al. Examination of human stomach biopsies, saliva, and dental plaque for
Campylobacter pylori
. J Clin Microbiol. 1989; 27:1397–1398.

4. Dye BA, Kruszon-Moran D, McQuillan G. The relationship between periodontal disease attributes and
Helicobacter pylori infection among adults in the United States. Am J Public Health. 2002; 92:1809–1815.

5. Souto R, Colombo AP. Detection of
Helicobacter pylori by polymerase chain reaction in the subgingival biofilm and saliva of non-dyspeptic periodontal patients. J Periodontol. 2008; 79:97–103.

6. Al Asqah M, Al Hamoudi N, Anil S, Al Jebreen A, Al-Hamoudi WK. Is the presence of
Helicobacter pylori in dental plaque of patients with chronic periodontitis a risk factor for gastric infection? Can J Gastroenterol. 2009; 23:177–179.

7. Nonnenmacher C, Dalpke A, Rochon J, Flores-de-Jacoby L, Mutters R, Heeg K. Real-time polymerase chain reaction for detection and quantification of bacteria in periodontal patients. J Periodontol. 2005; 76:1542–1549.

8. Tatakis DN, Kumar PS. Etiology and pathogenesis of periodontal diseases. Dent Clin North Am. 2005; 49:491–516.

9. Mysak J, Podzimek S, Sommerova P, Lyuya-Mi Y, Bartova J, Janatova T, et al. Porphyromonas gingivalis: major periodontopathic pathogen overview. J Immunol Res. 2014; 2014:476068.
10. Socransky SS, Haffajee AD. Dental biofilms difficult therapeutic targets. Periodontol 2000. 2002; 28:12–55.

11. Andersen RN, Ganeshkumar N, Kolenbrander PE.
Helicobacter pylori adheres selectively to
Fusobacterium spp. Oral Microbiol Immunol. 1998; 13:51–54.

12. Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998; 25:134–144.

13. Okuda K, Kimizuka R, Katakura A, Nakagawa T, Ishihara K. Ecological and immunopathological implications of oral bacteria in
Helicobacter pylori-infected disease. J Periodontol. 2003; 74:123–128.

14. Hu Z, Zhang Y, Li Z, Yu Y, Kang W, Han Y, et al. Effect of Helicobacter pylori infection on chronic periodontitis by the change of microecology and inflammation. Oncotarget. 2016; 7:66700–66712.
15. Al Sayed A, Anand PS, Kamath KP, Patil S, Preethanath RS, Anil S. Oral cavity as an extragastric reservoir of Helicobacter pylori
. ISRN Gastroenterol. 2014; 2014:261369.
16. Zu L. Reviews of research on the relationship between oral
Helicobacter pylori and
H. pylori infection. Infect Int. 2016; 5:5–10.

17. Salehi MR, Shah Aboei M, Naghsh N, Hajisadeghi S, Ajami E. A comparison in prevalence of Helicobacter pylori in the gingival crevicular fluid from subjects with periodontitis and healthy individuals using polymerase chain reaction. J Dent Res Dent Clin Dent Prospect. 2013; 7:238–243.
18. Chu YT, Wang YH, Wu JJ, Lei HY. Invasion and multiplication of
Helicobacter pylori in gastric epithelial cells and implications for antibiotic resistance. Infect Immun. 2010; 78:4157–4165.

19. Evans DG, Evans DJ Jr, Graham DY. Adherence and internalization of
Helicobacter pylori by HEp-2 cells. Gastroenterology. 1992; 102:1557–1567.

20. Dubois A, Borén T.
Helicobacter pylori is invasive and it may be a facultative intracellular organism. Cell Microbiol. 2007; 9:1108–1116.

21. Huang Y, Wang QL, Cheng DD, Xu WT, Lu NH. Adhesion and invasion of gastric mucosa epithelial cells by
Helicobacter pylori
. Front Cell Infect Microbiol. 2016; 6:159.

22. Petersen AM, Krogfelt KA.
Helicobacter pylori: an invading microorganism? A review. FEMS Immunol Med Microbiol. 2003; 36:117–126.
23. Necchi V, Candusso ME, Tava F, Luinetti O, Ventura U, Fiocca R, et al. Intracellular, intercellular, and stromal invasion of gastric mucosa, preneoplastic lesions, and cancer by
Helicobacter pylori
. Gastroenterology. 2007; 132:1009–1023.

24. Amieva MR, Salama NR, Tompkins LS, Falkow S.
Helicobacter pylori enter and survive within multivesicular vacuoles of epithelial cells. Cell Microbiol. 2002; 4:677–690.

25. Bode G, Mauch F, Malfertheiner P. The coccoid forms of Helicobacter pylori. Criteria for their viability. Epidemiol Infect. 1993; 111:483–490.
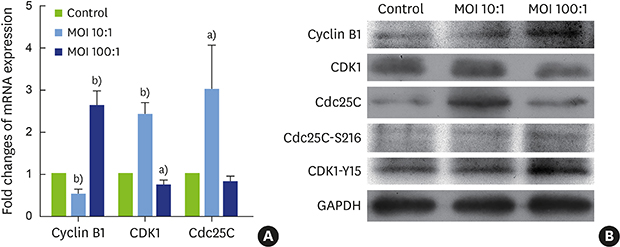
26. Cuddihy AR, O'Connell MJ. Cell-cycle responses to DNA damage in G2. Int Rev Cytol. 2003; 222:99–140.

27. Strauss B, Harrison A, Coelho PA, Yata K, Zernicka-Goetz M, Pines J. Cyclin B1 is essential for mitosis in mouse embryos, and its nuclear export sets the time for mitosis. J Cell Biol. 2018; 217:179–193.

28. Santos SD, Wollman R, Meyer T, Ferrell JE Jr. Spatial positive feedback at the onset of mitosis. Cell. 2012; 149:1500–1513.

29. Schmidt M, Rohe A, Platzer C, Najjar A, Erdmann F, Sippl W. Regulation of G2/M transition by inhibition of WEE1 and PKMYT1 kinases. Molecules. 2017; 22:E2045.

30. Sur S, Agrawal DK. Phosphatases and kinases regulating CDC25 activity in the cell cycle: clinical implications of CDC25 overexpression and potential treatment strategies. Mol Cell Biochem. 2016; 416:33–46.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download