Abstract
Purpose
Anatomical variations of the external nasal wall are highly important, since they play a role in obstruction or drainage of the ostiomeatal complex and ventilation and can consequently elevate the risk of pathological sinus conditions. This study aimed to assess anatomical variations of the nasal cavity and ethmoidal sinuses and their correlations on cone-beam computed tomography (CBCT) scans.
Materials and Methods
This cross-sectional study evaluated CBCT scans of 250 patients, including 107 males and 143 females, to determine the prevalence of anatomical variations of the nasal cavity and ethmoidal sinuses. All images were taken using a New Tom 3G scanner. Data were analyzed using the chi-square test, Kruskal-Wallis test, and the Mann-Whitney test.
Results
The most common anatomical variations were found to be nasal septal deviation (90.4%), agger nasi air cell (53.6%), superior orbital cell (47.6%), pneumatized nasal septum (40%), and Onodi air cell (37.2%). Correlations were found between nasal septal deviation and the presence of a pneumatized nasal septum, nasal spur, and Haller cell. No significant associations were noted between the age or sex of patients and the presence of anatomical variations (P>0.05).
Go to : 
The paranasal sinuses are 4 pairs of air spaces located around the nasal cavity. The nasal cavity and the paranasal sinuses decrease the weight of the skull, warm and moisturize the inhaled air, regulate speech resonance and intranasal pressure, and improve the sense of smell.12 Pathological changes are often of greater interest to radiologists than anatomical variations.3 Nonetheless, anatomical variations of the lateral nasal wall are highly important since they play a role in obstruction or drainage of the ostiomeatal complex and ventilation, and can consequently elevate the risk of sinus conditions.4 Moreover, anatomical variations can affect the outcomes and safety of surgical procedures performed in this region.5
The formation of paranasal sinuses following depression of the nasal mucosa around the facial bones explains the high frequency of anatomical variations in this region.6 Anatomical variations of the paranasal sinuses are highly important since they may predict inflammatory changes in the paranasal sinuses. Such variations of the sinus can complicate clinical procedures, particularly functional endoscopic surgery, in which accurate assessment of the region plays a pivotal role in the success and safety of surgical procedures.7 Most dental clinicians are acquainted with radiographic images of the maxillary sinuses on 2-dimensional (periapical and panoramic) radiographs.2 Computed tomography (CT) is the modality of choice for assessing the paranasal sinuses, and the coronal section is the best section for evaluation of the ostiomeatal complex.7
Cone-beam computed tomography (CBCT) is the most significant technological advance in maxillofacial imaging since the introduction of panoramic radiography. CBCT, which was initially developed commercially for angiography in the early 1980s,8 is a novel imaging modality that generates high-quality images with high accuracy.9 In comparison to CT scans, the lower radiation dose of CBCT, its lower cost, and the compact scanner design have made CBCT a suitable modality for diagnosis and treatment planning, particularly in the head and neck region. According to recent studies, CBCT has adequate quality for imaging of paranasal sinuses, even with low doses of X-ray irradiation.610
Considering the advances in imaging technology in recent decades, increased attention has been paid to the radiographic details of the anatomy of the paranasal sinuses and ostiomeatal complex.11 CBCT may be preferable to CT for these purposes because it yields high-quality images of bony structures, including maxillary structures, and is particularly valuable for assessing the position, shape, and variations of the paranasal sinuses.7
To the best of our knowledge, a comprehensive range of anatomical variations and their correlations have been evaluated in a limited number of studies. Thus, the aim of this study was to calculate the frequency of anatomical variations of the nasal cavity and ethmoidal sinuses on CBCT scans, to determine the statistical significance of differences in the frequency of these anatomical variations according to sex and age, and to evaluate the correlations between different variations.
Go to : 
This cross-sectional study evaluated CBCT scans of the nasal cavity and ethmoidal sinuses retrieved from the archives of the Radiology Department of the School of Dentistry, Hamadan University of Medical Sciences, Iran from 2013 to 2016 and received ethical approval from Hamadan University of Medical Sciences under the code IR.UMSHA. REC.1396.616. This study included images from 250 patients (107 males and 143 females) in the age range of 10–55 years. The patients' age was limited to the range of 10–55 years to ensure sufficient accuracy of the statistical results because the majority of the patients were in this age range. Patients with a history of surgical procedures in this region, trauma to the head or face, and clefts or benign or malignant tumors of the sinonasal mucosa causing changes in the anatomy of the nasal cavity or ethmoidal sinuses were excluded. Patients were divided into 3 age groups (10–25 years, 26–40 years, and 41–55 years) to obtain a uniform sample distribution.
All images were captured with a New Tom 3G CBCT scanner (Quantitative Radiology, Verona, Italy) and evaluated in the axial, coronal, and sagittal planes by an oral and maxillofacial radiologist with 10 years of educational experience and a senior resident of oral and maxillofacial radiology using NNT Viewer software (New Tom, Verona, Italy). The images were viewed on a 20-inch LG monitor (LG, Seoul, Korea) in partly dark conditions. The observers could change the optical density and contrast of images using rendering software. The results were documented using a checklist. If there was any conflict between the 2 observers, the final decision was made by consulting a third observer, who was an experienced oral and maxillofacial radiologist. All images were analyzed again by the observers after 2 weeks, and the results were documented. The parameters that were evaluated are described below.
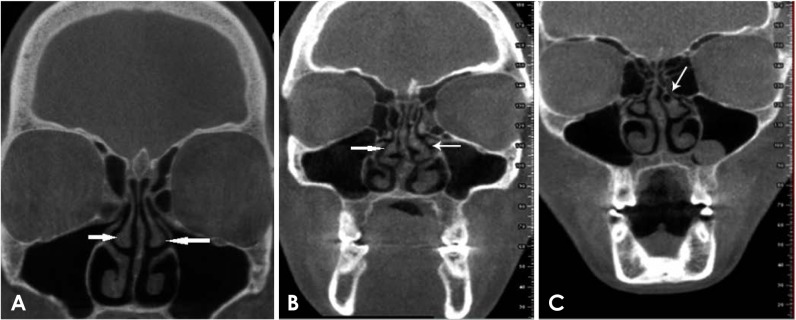
The first parameter was the shape of the middle turbinate, which was categorized as normal, paradoxical, or concha bullosa (Fig. 1). A paradoxical middle turbinate is a rare developmental variation of the middle turbinate in which the border of the middle turbinate is bent and its convex surface faces the lateral aspect. There is no evidence supporting a correlation between the presence of paradoxical middle turbinate and sinusitis, although clear obstruction of the nasal airway can occur due to a paradoxical middle turbinate.1213 Concha bullosa, which can occur in any part of the ethmoid bone complex that becomes pneumatized, is the most common anatomical variation that occurs in the middle turbinate. When it occurs, posterior ethmoidal air cells are pulled in to pneumatize the middle turbinate. The area of pneumatization of the turbinate can be small, medium, or large. Very large cases can cause nasal septal deviation and nasal obstruction.112
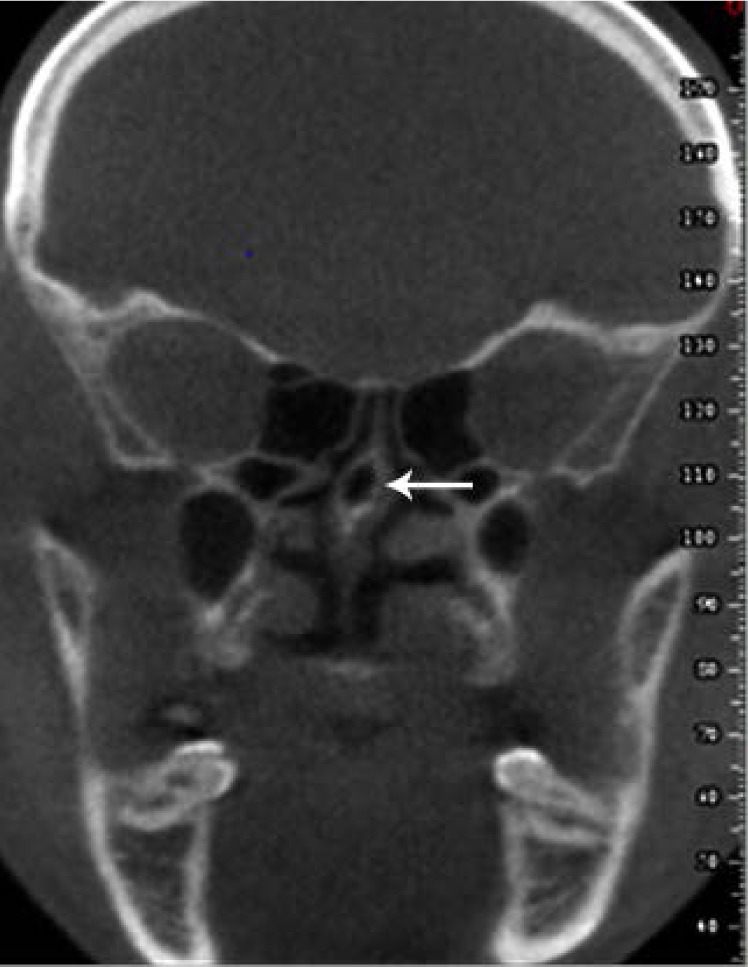
The second parameter was the shape of the uncinate process. The uncinate process of the ethmoid bone is a thin hook-like osseous structure of the wall of the lateral nasal cavity, which can be normal, atelectatic, inclusive of the lamina terminalis, pneumatized, or curved (Fig. 2). In an atelectatic uncinate process, the free margin of the uncinate process may sometimes be attached to the orbital floor or the inferior surface of the lamina papyracea. It is often associated with a hypoplastic maxillary sinus, which is usually opaque due to obstruction of the infundibulum.12 The lamina terminalis is defined as a superior extension of the uncinate process towards the roof of the anterior ethmoid.12 Pneumatization of the uncinate process is rare, but may occur as the result of intrusion of air cells into the uncinate process, which can cause narrowing of the infundibulum and impair ventilation.1 A curved uncinate process is defined as any curvature in the uncinate process that can cause stenosis of the ostium of the maxillary sinus.12
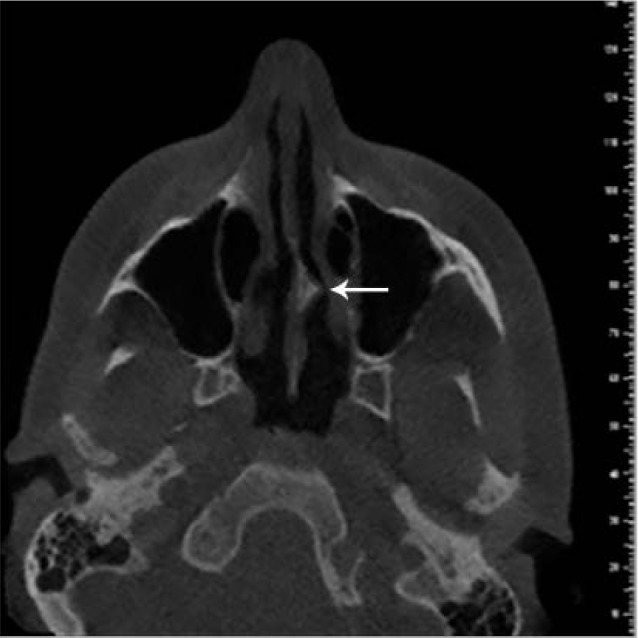
The third parameter was nasal septal deviation (Fig. 3), which refers to any curvature in the nasal septum and is seen in more than half of patients. Nasal septal deviation leads to compensatory hypertrophy of the inferior turbinate and the occurrence of concha bullosa in the middle turbinate at the convex side of the nasal septum. This further aggravates nasal obstruction.1
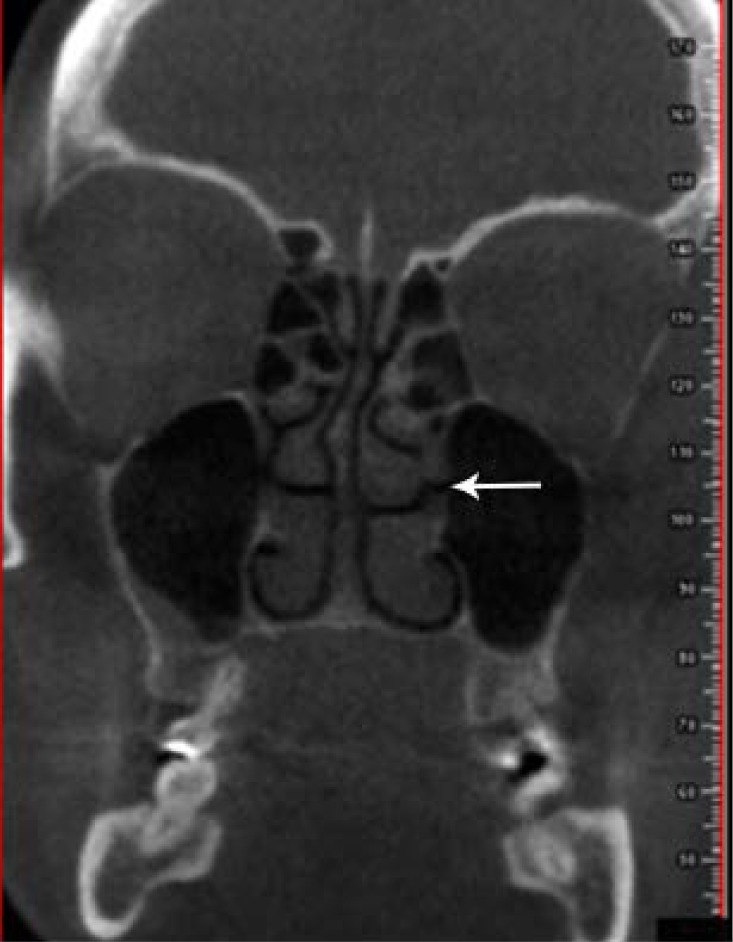
The fourth parameter was pneumatization of the nasal septum (Fig. 4). Air cells are often seen in the posterosuperior part of the nasal septum. When present, they are related to the sphenoid sinus. Thus, inflammatory disease in the paranasal sinuses may affect these cells.12
The fifth parameter was the presence of a nasal septal spine (Fig. 5). A spine may be present on the nasal septum. It often forms at the interface of the perpendicular plate of the ethmoid bone and the upper surface of the vomer. In some cases, a nasal spine forms on the convex or concave part of a deviated nasal septum and can be tangent to the turbinate or the lateral nasal wall.12
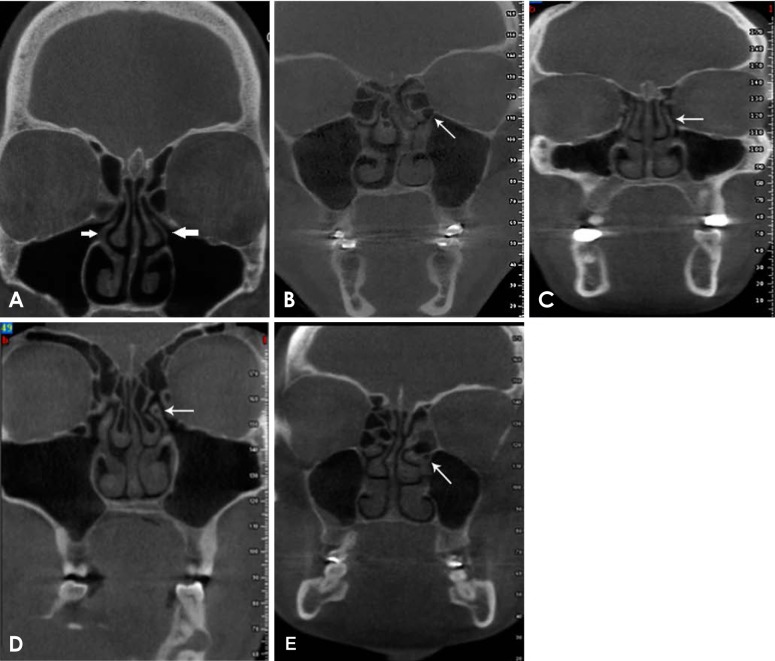
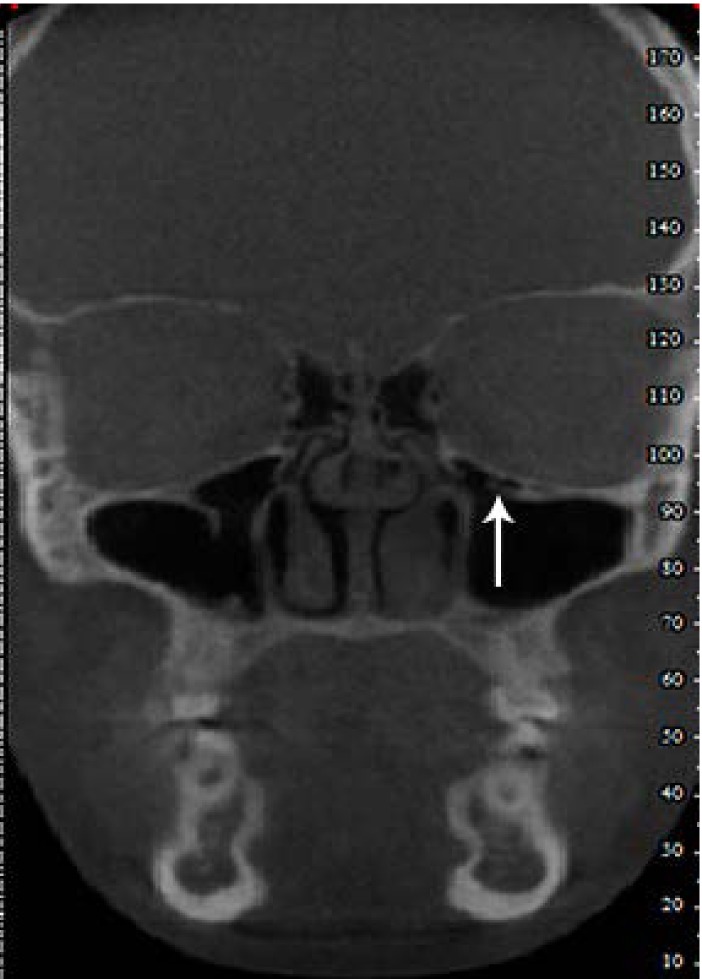
The sixth parameter was the presence of an Onodi cell (Fig. 6). Posterior ethmoidal cells can also invade the sphenoid bone, usually from the superior and lateral parts, and may become associated with the optic nerve and internal carotid artery. This phenomenon is therefore a risk factor during surgical procedures.712
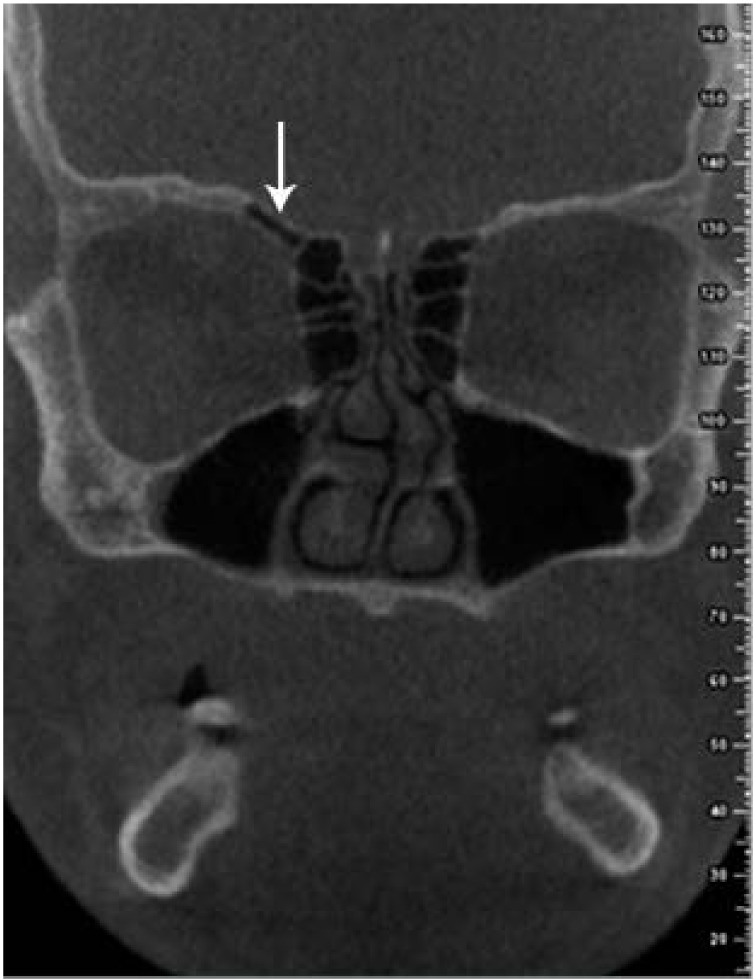
The seventh parameter was the presence of an anterior agger nasi cell (Fig. 7), which reflects a clinically important pattern of the outward spread of air cells. Anterior ethmoidal cells can pneumatize the frontal process of the maxilla. These cells are known as agger nasi cells and are related to the lacrimal bone.12
The seventh parameter was asymmetry of the ethmoid roof (Fig. 8). Any asymmetry in the height of the ethmoid roof should be taken into account, because in endoscopic surgery of the sinus, such anatomical variations increase the risk of further penetration into the brain from the lower side of the roof.12
The eighth parameter was the presence of accessory maxillary sinus ostium (Fig. 9). The membranous areas in the middle meatus can disintegrate following obstruction of the maxillary sinus ostium, sinusitis, or other anatomical or pathological factors, resulting in the formation of accessory maxillary sinus ostium.12
The ninth parameter was the presence of a Haller cell (Fig. 10), which is a posterior ethmoidal cell invading the floor of the orbit and internal orbital wall; Haller cells can sometimes obstruct the ostiomeatal complex and impair sinus drainage, thereby leading to persistent infections.712
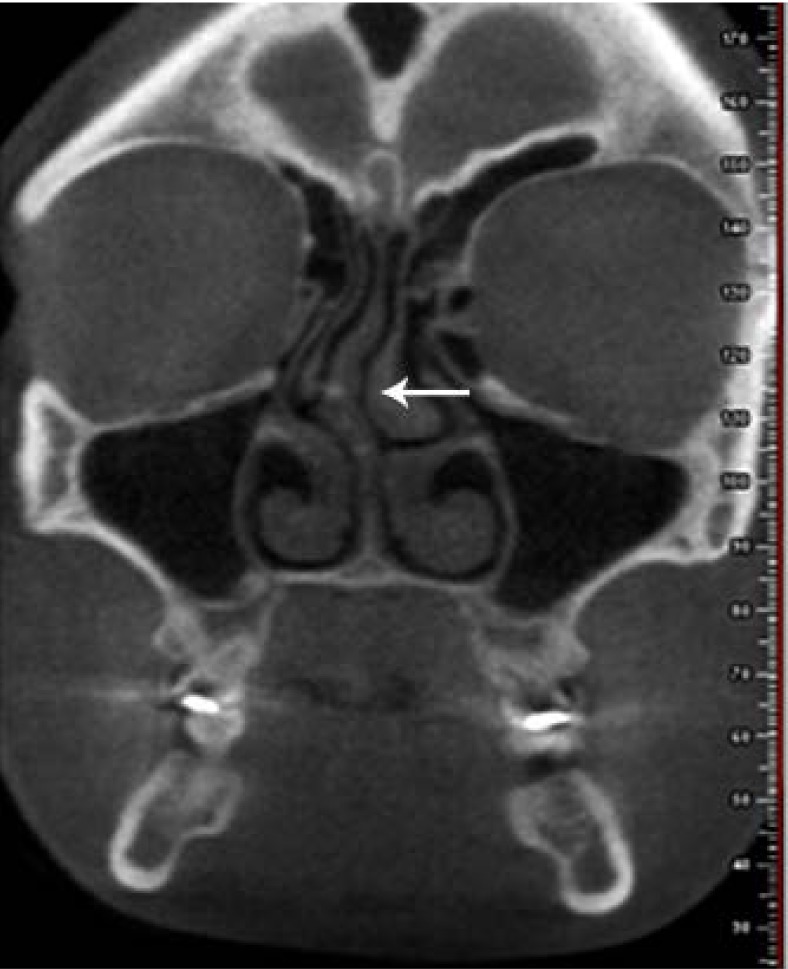
The tenth parameter was the presence of a superior orbital cell (Fig. 11). Anterior ethmoidal cells can pneumatize the orbital floor as supraorbital ethmoidal cells. Not detecting such cells can cause surgical procedures of the frontal sinus to fail.12
The chi-square test, Kruskal-Wallis test, and Mann-Whitney test were used for multiple comparisons. P values lower than 0.05 were considered to indicate statistical significance. All statistical analyses were performed using SPSS version 24 (IBM Corp., Armonk, NY, USA).
Go to : 
The intra-class correlation was calculated to assess intraobserver and interobserver reliability, and values of 94% and 92% were found for interobserver agreement and intraobserver agreement, respectively.
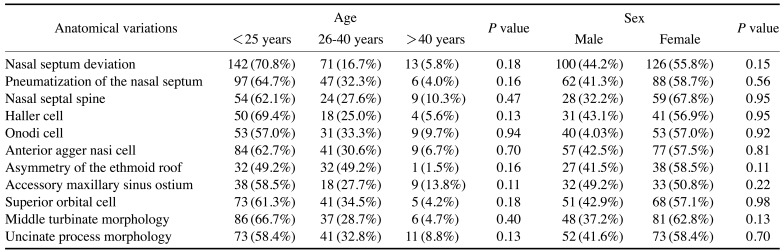
The highest prevalence of anatomical variations was noted in 10- to 25-year-olds. The Mann-Whitney test revealed no significant relationship between the prevalence of anatomical variations and patients' sex (P=0.254), and the Kruskal-Wallis test showed no significant relation between the prevalence of anatomical variations and patients' age (P=0.273). Table 1 summarizes these data.
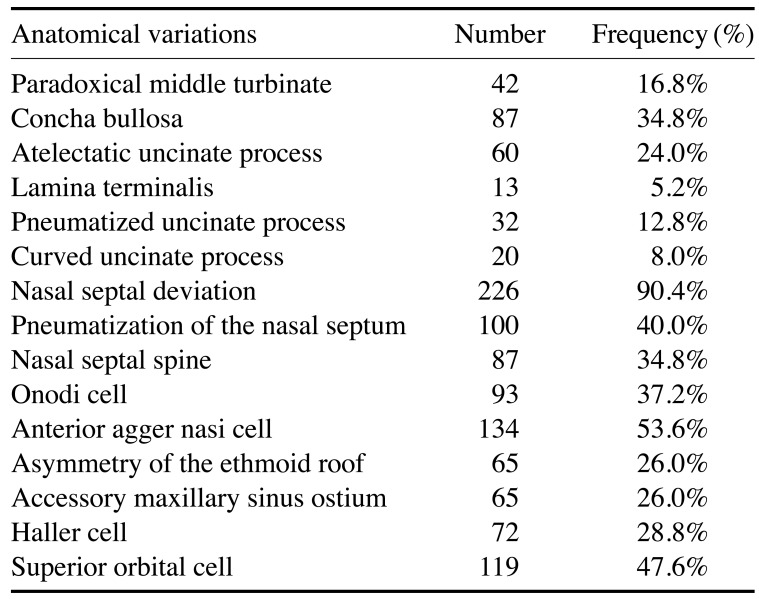
The most common anatomical variations in order of frequency were as follows: nasal septal deviation (90.4%), agger nasi cells (53.6%), superior orbital cells (47.6%), a pneumatized nasal septum (40%), and Onodi cells (37.2%). Table 2 summarizes these findings.
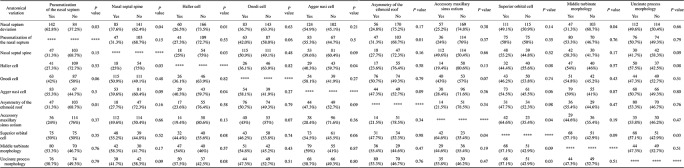
There were significant correlations between the presence of nasal septal deviation and pneumatized nasal septum (P=0.03), Haller cell (P=0.01), as well as between a pneumatized nasal septum and asymmetry of the ethmoid roof (P=0.01). Correlations were also observed between the presence of a Haller cell and an agger nasi cell (P=0.04) and nasal septal spine (P=0.03), as well as between the presence of a superior orbital cell and accessory maxillary sinus ostium (P=0.04). Table 3 summarizes these data.
Go to : 
Anatomical variations of the sinonasal region should be carefully identified prior to surgical procedures. These anatomical variations are important for 2 reasons. First, anatomical variations have a direct correlation with the drainage and ventilation of the paranasal sinuses. Second, anatomical variations can significantly affect the safety of surgical procedures.141516
CBCT is a novel imaging modality with a higher modulation transfer function than CT, leading to higher spatial resolution. Furthermore, CBCT has a lower patient radiation dose and cost than CT. With these advantages, CBCT can provide accurate information about maxillofacial anatomy.710
Previous studies have reported the prevalence of anatomical variations in this region to be 64%–98%. The prevalence of anatomical variations was found to be 5.2%–90.4% in our study. This discrepancy may be due to differences in age, race, and the type of imaging modality used.13
In the present study, the prevalence of concha bullosa was 32.8%, in agreement with the results of Roman et al. (35%) and Mamatha et al. (15%).717 However, no significant correlation exists between sinusitis and concha bullosa unless the concha bullosa is large enough to cause airway obstruction.1216 The prevalence of paradoxical middle turbinate was 16.8% in our study, which is in agreement with the results of Dasar and Gokce (15.8%), Adeel et al. (18.2%), and Al-Abri et al. (13%).31318
Knowledge of uncinate process variations in patients undergoing functional endoscopic sinus surgery is imperative for the surgeon. During uncinectomy, if the uncinate process is attached to the ethmoid roof or the middle turbinate, the surgeon must be careful not to apply excessive tensile or torsional force on its superior tip. If it is unintentionally damaged, cerebrospinal fluid rhinorrhea or brain damage may occur. In some cases, the free margin of the uncinate process is attached to the orbital floor or the inferior surface of the lamina papyracea and is often associated with a hypoplastic maxillary sinus, which is frequently opaque due to obstruction of the infundibulum. When the orbital floor of the same side is low due to maxillary sinus hypoplasia, the risk of penetration into the orbit during surgery increases. During the preoperative assessment, it is important to pay close attention to anatomical variations. Furthermore, an abnormal shape or position may play a role in the development of sinusitis.51213
In our study, the prevalence of anatomical variations in the morphology of the uncinate process was 50%, which is in agreement with the results of Khojastepour et al. (54.8%), and Mamtha et al. (65%).517
Nasal septal deviation is another common anatomical variation, with a prevalence of 14.1%–80%.112 It has been reported that nasal septal deviation can cause infection of all paranasal sinuses, due to narrowing of the airway, weak mucociliary clearance, and mucus drainage.118 In the current study, the prevalence of nasal septal deviation was 90.4%, which is in agreement with the results of Aramani et al. (75%).16
The nasal septum was almost always deviated away from either a unilateral concha or the dominant concha if there were bilateral conchae. The septum was not pushed by the concha, as the air channel between them was maintained. There appears to be some type of an inductive relationship between the presence of concha bullosa and deviated septum.12
In the present study, a correlation between middle turbinate morphology and nasal septum deviation was detected, which is validated by the study of Koo et al.1
A spine may be present on the nasal septum, which is often located at the interface of the perpendicular plate of the ethmoid bone and the upper surface of the vomer. In some cases, the nasal spine is located over the concave or convex part of the deviated nasal septum and can be tangent to the turbinate or the lateral nasal wall. There appears to be a relationship between the presence of a nasal septal spine and deviated septum, although in this study a correlation was found between nasal septum deviation and a nasal septal spine.12
The prevalence of a nasal spine was 34.8% in our study, which is in accordance with the results of Dasar and Gokce (42.3%). Approximately half of patients with nasal spine have been reported to have sinonasal mucosal diseases, but no such association was confirmed in this study.13 Moreover, 36% of patients had both nasal septal deviation and a nasal spine in our study, which is in agreement with the findings of Earwaker (34%).21 When nasal septal deviation and a nasal spine are both present, the nasal meatus path is narrowed, impairing the function of nasal endoscopy and functional endoscopic sinus surgery (FESS).131920
Some authors believe that Haller cells are responsible for the recurrence of maxillary sinusitis, but their effect on the prevalence of sinusitis is still a matter of debate.1216 In the current study, the prevalence of Haller cells was 28.8%. In the literature, the reported prevalence ranges from 2% to 70%. This broad range may be due to controversies in the definition of Haller cells and differences in the mean age of patients, their race, and the imaging protocols used.14212223
Nonetheless, a correlation was detected in this study between Haller cells and nasal septum deviation was detected, as validated by Dasar and Gokce's study.13
Onodi cells often extend close to the carotid canal and optic nerve, further adding to the significance of this anatomical variant during surgical procedures. Invasive procedures should be avoided in this area. Additionally, in the preoperative assessment, surgeons should pay close attention to Onodi cells to prevent any problems in FESS.1 The presence of an Onodi cell can result in traumatization of the olfactory nerve during surgical procedures. Additionally, infections of Onodi cells can compress the optic nerve and cause periorbital swelling.13 The reported prevalence of Onodi cells ranges from 3.4% to 51%, and the prevalence found in the present study was 30.8%, in agreement with the results of Dasar and Gokce (25.3%).1213
Evidence has shown that the larger size of agger nasi cells can narrow the drainage path of the frontal sinus and impair drainage. However, other studies have found no significant association between agger nasi cells and frontal sinus infection.1317
The presence of an asymmetrical ethmoid sinus roof is among the most common anatomical variants of the sinonasal region; it has a significant correlation with chronic sinusitis and is seen in over 80% of patients with sinusitis.12
During surgical procedures, any asymmetry in the height of the ethmoid roof should be taken into account because during endoscopic surgery of the sinus, these anatomical variations increase the risk of penetration into the brain in the lower side of the roof.12 This variation had a prevalence of 26% in our study, in agreement with the results of Fadda et al. (25%), and Al-Abri et al.(32%).324
Anterior ethmoidal cells can pneumatize the orbital floor as supraorbital ethmoidal cells. Not noticing the diseased condition of these cells can cause frontal sinus surgical procedures to fail.3
The prevalence of supraorbital cells was 26% in our study, in line with the results of Dasar and Gokce (15%).13 The prevalence of accessory maxillary sinus ostium has been reported to be 15%–40%, and this variant structure often drains into the infundibulum or, even more commonly, the fontanel.11 In our study, the prevalence of accessory maxillary sinus ostium was 26%, similar to the value reported by Dasar and Gokce (21.8%).13
Patients' age and sex showed no significant correlations with anatomical variations in our study, similar to the findings of Khojastepour et al.5
We conclude that the high prevalence of anatomical variations in the ostiomeatal complex and their correlations mean that they are very important considerations when establishing a diagnosis or treatment plan. Radiologists must focus on anatomical variants in the preoperative evaluation, and it is important for surgeons to be aware of these variations.
Go to : 
Acknowledgements
The authors would like to thank the Vice-Chancellor for Education and the Vice-Chancellor for Research and Technology of Hamadan University of Medical Sciences, and to express special thanks to Dr. Samira Saati, an oral and maxillofacial radiologist, who was the third observer for evaluating the images.
Go to : 
References
1. Koo SK, Kim JD, Moon JS, Jung SH, Lee SH. The incidence of concha bullosa, unusual anatomic variation and its relationship to nasal septal deviation: a retrospective radiologic study. Auris Nasus Larynx. 2017; 44:561–570. PMID: 28173975.

2. Parks ET. Cone beam computed tomography for the nasal cavity and paranasal sinuses. Dent Clin North Am. 2014; 58:627–651. PMID: 24993926.

3. Al-Abri R, Bhargava D, Al-Bassam W, Al-Badaai Y, Sawhney S. Clinically significant anatomical variants of the paranasal sinuses. Oman Med J. 2014; 29:110–113. PMID: 24715937.

4. Tao Z, Zhang J, Yang Q, Xiao B, Kong Y. Differences of anatomic variations in ostiomeatal complex between two sides of the deviated septum. Zhonghua Er Bi Yan Hou Ke Za Zhi. 2001; 36:132–134. PMID: 12761982.
5. Khojastepour L, Mirhadi S, Mesbahi SA. Anatomical variations of ostiomeatal complex in CBCT of patients seeking rhinoplasty. J Dent (Shiraz). 2015; 16:42–48. PMID: 25759857.
6. Güldner C, Ningo A, Voigt J, Diogo I, Heinrichs J, Weber R, et al. Potential of dosage reduction in cone-beam-computed tomography (CBCT) for radiological diagnostics of the paranasal sinuses. Eur Arch Otorhinolaryngol. 2013; 270:1307–1315. PMID: 22986413.

7. Roman RA, Hedeşiu M, Gersak M, Fidan F, Băciuţ G, Băciuţ M. Assessing the prevalence of paranasal sinuses anatomical variants in patients with sinusitis using cone beam computer tomography. Clujul Med. 2016; 89:419–421.

8. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th ed. St. Louis: Elsevier;2014.
9. Shokri A, Khajeh S. In vitro comparison of the effect of different slice thicknesses on the accuracy of linear measurements on cone beam computed tomography images in implant sites. J Craniofac Surg. 2015; 26:157–160. PMID: 25569395.

10. Shokri A, Miresmaeili A, Farhadian N, Falah-Kooshki S, Amini P, Mollaie N. Effect of changing the head position on accuracy of transverse measurements of the maxillofacial region made on cone beam computed tomography and conventional posterior-anterior cephalograms. Dentomaxillofac Radiol. 2017; 46:20160180. PMID: 28306330.

11. de Miranda CM, de Miranda Maranhão CP, Arraes FM, Padilha IG, de Farias LD, de Araujo Jatobá MS. Anatomical variations of paranasal sinuses at multislice computed tomography: what to look for. Radiol Bras. 2011; 44:256–262.
12. Som PM, Curtin HD. Head and neck imaging. 5th ed. St. Louis: Mosby Elsevier;2011.
13. Dasar U, Gokce E. Evaluation of variations in sinonasal region with computed tomography. World J Radiol. 2016; 8:98–108. PMID: 26834948.

14. Bremke M, Leppek R, Werner JA. Digital volume tomography in ENT medicine. HNO. 2010; 58:823–832. PMID: 20544169.
15. Kurzweg T, Dalchow CV, Bremke M, Majdani O, Kureck I, Knecht R, et al. The value of digital volume tomography in assessing the position of cochlear implant arrays in temporal bone specimens. Ear Hear. 2010; 31:413–419. PMID: 20440115.

16. Aramani A, Karadi RN, Kumar S. A study of anatomical variations of osteomeatal complex in chronic rhinosinusitis patients-CT findings. J Clin Diagn Res. 2014; 8:KC01–KC04.
17. Mamatha H, Shamasundar NM, Bharathi MB, Prasanna LC. Variations of ostiomeatal complex and its applied anatomy: a CT scan study. Indian J Sci Technol. 2010; 3:904–907.

18. Adeel M, Rajput MS, Akhter S, Ikram M, Arain A, Khattak YJ. Anatomical variations of nose and para-nasal sinuses; CT scan review. J Pak Med Assoc. 2013; 63:317–319. PMID: 23914628.
19. Lerdlum S, Vachiranubhap B. Prevalence of anatomic variation demonstrated on screening sinus computed tomography and clinical correlation. J Med Assoc Thai. 2005; 88(Suppl 4):S110–S115.
20. Stallman JS, Lobo JN, Som PM. The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease. AJNR Am J Neuroradiol. 2004; 25:1613–1618. PMID: 15502150.
22. Mathew R, Omami G, Hand A, Fellows D, Lurie A. Cone beam CT analysis of Haller cells: prevalence and clinical significance. Dentomaxillofac Radiol. 2013; 42:20130055. PMID: 23975112.

23. Fadda GL, Rosso S, Aversa S, Petrelli A, Ondolo C, Succo G. Multiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. Acta Otorhinolaryngol Ital. 2012; 32:244–251. PMID: 23093814.
24. Albuquerque CB, Zambrana NR, Zambrana JR, Ribeiro RA, Salgado DM, Costa C. Evaluation of prevalence of Haller cells and their relationship with maxilofacial changes. Clin Lab Res Dent. 2018; 54:1–7.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download