1. Hultén LM, Levin M. The role of hypoxia in atherosclerosis. Curr Opin Lipidol. 2009; 20:409–414. PMID:
19644366.

2. Taylor PC, Sivakumar B. Hypoxia and angiogenesis in rheumatoid arthritis. Curr Opin Rheumatol. 2005; 17:293–298. PMID:
15838239.

3. Ishida S, Shinoda K, Kawashima S, Oguchi Y, Okada Y, Ikeda E. Coexpression of VEGF receptors VEGF-R2 and neuropilin-1 in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 2000; 41:1649–1656. PMID:
10845581.
4. Mateo J, Izquierdo-Garcia D, Badimon JJ, Fayad ZA, Fuster V. Noninvasive assessment of hypoxia in rabbit advanced atherosclerosis using
18f-fluoromisonidazole PET imaging. Circ Cardiovasc Imaging. 2014; 7:312–320. PMID:
24508668.
5. Fu Q, Colgan SP, Shelley CS. Hypoxia: the force that drives chronic kidney disease. Clin Med Res. 2016; 14:15–39. PMID:
26847481.

6. Bonnitcha P, Grieve S, Figtree G. Clinical imaging of hypoxia: current status and future directions. Free Radic Biol Med. 2018; 126:296–312. PMID:
30130569.

7. Vaupel P, Mayer A, Höckel M. Tumor hypoxia and malignant progression. Methods Enzymol. 2004; 381:335–354. PMID:
15063685.

8. Wallace TE, Patterson AJ, Abeyakoon O, Bedair R, Manavaki R, McLean MA, et al. Detecting gas-induced vasomotor changes via blood oxygenation level-dependent contrast in healthy breast parenchyma and breast carcinoma. J Magn Reson Imaging. 2016; 44:335–345. PMID:
26898173.

9. Vaupel P. Prognostic potential of the pre-therapeutic tumor oxygenation status. Adv Exp Med Biol. 2009; 645:241–246. PMID:
19227477.

10. Gilkes DM. Implications of hypoxia in breast cancer metastasis to bone. Int J Mol Sci. 2016; 17:E1669. PMID:
27706047.

11. Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signalling - in control of vascular function. Nat Rev Mol Cell Biol. 2006; 7:359–371. PMID:
16633338.

12. Lu H, Shu XO, Cui Y, Kataoka N, Wen W, Cai Q, et al. Association of genetic polymorphisms in the VEGF gene with breast cancer survival. Cancer Res. 2005; 65:5015–5019. PMID:
15958542.

13. Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin Oncol. 2002; 29:15–18.

14. Harris AL. Hypoxia--a key regulatory factor in tumour growth. Nat Rev Cancer. 2002; 2:38–47. PMID:
11902584.
15. Vaupel P, Harrison L. Tumor hypoxia: causative factors, compensatory mechanisms, and cellular response. Oncologist. 2004; 9(Suppl 5):4–9.

16. Bristow RG, Hill RP. Hypoxia and metabolism. Hypoxia, DNA repair and genetic instability. Nat Rev Cancer. 2008; 8:180–192. PMID:
18273037.
17. Shaw RJ. Glucose metabolism and cancer. Curr Opin Cell Biol. 2006; 18:598–608. PMID:
17046224.

18. Dang CV, Semenza GL. Oncogenic alterations of metabolism. Trends Biochem Sci. 1999; 24:68–72. PMID:
10098401.

19. Semenza GL. Hydroxylation of HIF-1: oxygen sensing at the molecular level. Physiology (Bethesda). 2004; 19:176–182. PMID:
15304631.

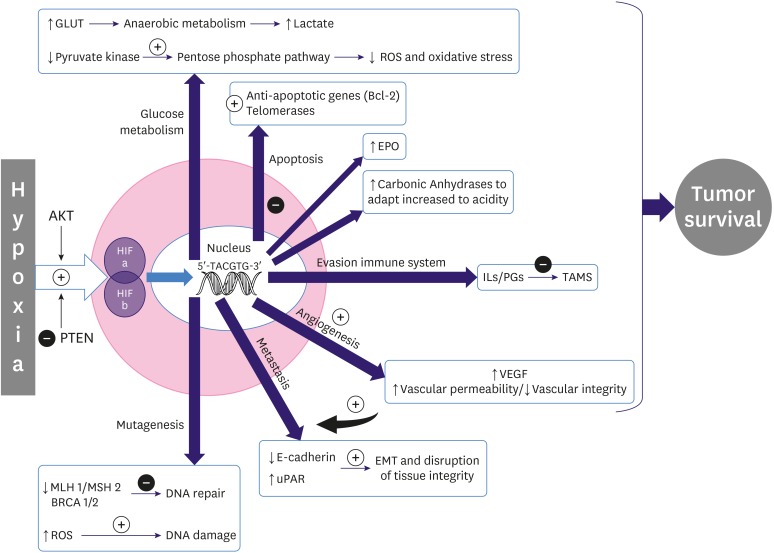
20. Adamaki M, Georgountzou A, Moschovi M. Cancer and the cellular response to hypoxia. Pediatr Therapeut. 2012; S1:002.

21. Gatenby RA, Smallbone K, Maini PK, Rose F, Averill J, Nagle RB, et al. Cellular adaptations to hypoxia and acidosis during somatic evolution of breast cancer. Br J Cancer. 2007; 97:646–653. PMID:
17687336.

22. Leek RD, Talks KL, Pezzella F, Turley H, Campo L, Brown NS, et al. Relation of hypoxia-inducible factor-2 alpha (HIF-2 alpha) expression in tumor-infiltrative macrophages to tumor angiogenesis and the oxidative thymidine phosphorylase pathway in Human breast cancer. Cancer Res. 2002; 62:1326–1329. PMID:
11888900.
23. Carnero A, Lleonart M. The hypoxic microenvironment: a determinant of cancer stem cell evolution. BioEssays. 2016; 38(Suppl 1):S65–S74. PMID:
27417124.

24. Harrison L, Blackwell K. Hypoxia and anemia: factors in decreased sensitivity to radiation therapy and chemotherapy? Oncologist. 2004; 9(Suppl 5):31–40. PMID:
15591420.

25. Terry S, Faouzi Zaarour R, Hassan Venkatesh G, Francis A, El-Sayed W, Buart S, et al. Role of hypoxic stress in regulating tumor immunogenicity, resistance and plasticity. Int J Mol Sci. 2018; 19:E3044. PMID:
30301213.

26. Nardinocchi L, Puca R, Sacchi A, D'Orazi G. Inhibition of HIF-1alpha activity by homeodomain-interacting protein kinase-2 correlates with sensitization of chemoresistant cells to undergo apoptosis. Mol Cancer. 2009; 8:1. PMID:
19128456.

27. De Francesco EM, Maggiolini M, Tanowitz HB, Sotgia F, Lisanti MP. Targeting hypoxic cancer stem cells (CSCs) with Doxycycline: implications for optimizing anti-angiogenic therapy. Oncotarget. 2017; 8:56126–56142. PMID:
28915578.

28. Gray LH, Conger AD, Ebert M, Hornsey S, Scott OC. The concentration of oxygen dissolved in tissues at the time of irradiation as a factor in radiotherapy. Br J Radiol. 1953; 26:638–648. PMID:
13106296.

29. Colliez F, Gallez B, Jordan BF. Assessing tumor oxygenation for predicting outcome in radiation oncology: a review of studies correlating tumor hypoxic status and outcome in the preclinical and clinical settings. Front Oncol. 2017; 7:10. PMID:
28180110.

30. Overgaard J. Hypoxic radiosensitization: adored and ignored. J Clin Oncol. 2007; 25:4066–4074. PMID:
17827455.

31. Vordermark D, Horsman MR. Hypoxia as a biomarker and for personalized radiation oncology. Recent Results Cancer Res. 2016; 198:123–142. PMID:
27318684.

32. Wardman P. Chemical radiosensitizers for use in radiotherapy. Clin Oncol (R Coll Radiol). 2007; 19:397–417. PMID:
17478086.

33. Fleming IN, Manavaki R, Blower PJ, West C, Williams KJ, Harris AL, et al. Imaging tumour hypoxia with positron emission tomography. Br J Cancer. 2015; 112:238–250. PMID:
25514380.

34. Ueda S, Saeki T, Osaki A, Yamane T, Kuji I. Bevacizumab induces acute hypoxia and cancer progression in patients with refractory breast cancer: multimodal functional imaging and multiplex cytokine analysis. Clin Cancer Res. 2017; 23:5769–5778. PMID:
28679773.

35. Quintela-Fandino M, Lluch A, Manso L, Calvo I, Cortes J, García-Saenz JA, et al.
18F-fluoromisonidazole PET and activity of neoadjuvant nintedanib in early HER2-negative breast cancer: a window-of-opportunity randomized trial. Clin Cancer Res. 2017; 23:1432–1441. PMID:
27587436.
36. Cheng J, Lei L, Xu J, Sun Y, Zhang Y, Wang X, et al.
18F-fluoromisonidazole PET/CT: a potential tool for predicting primary endocrine therapy resistance in breast cancer. J Nucl Med. 2013; 54:333–340. PMID:
23401605.
37. Hypoxia-positron emission tomography (PET) and intensity modulated proton therapy (IMPT) dose painting in patients with chordomas. ClinicalTrials.gov Identifier: NCT00713037. 2017. U.S. National Library of Medicine;
https://clinicaltrials.gov/ct2/show/NCT00713037.
38. Reischl G, Dorow DS, Cullinane C, Katsifis A, Roselt P, Binns D, et al. Imaging of tumor hypoxia with [124I]IAZA in comparison with [18F]FMISO and [18F]FAZA--first small animal PET results. J Pharm Pharm Sci. 2007; 10:203–211. PMID:
17706178.
39. Grönroos T, Bentzen L, Marjamäki P, Murata R, Horsman MR, Keiding S, et al. Comparison of the biodistribution of two hypoxia markers [
18F]FETNIM and [
18F]FMISO in an experimental mammary carcinoma. Eur J Nucl Med Mol Imaging. 2004; 31:513–520. PMID:
14722675.
40. Xu Z, Li XF, Zou H, Sun X, Shen B.
18F-Fluoromisonidazole in tumor hypoxia imaging. Oncotarget. 2017; 8:94969–94979. PMID:
29212283.
41. Vāvere AL, Lewis JS. Cu-ATSM: a radiopharmaceutical for the PET imaging of hypoxia. Dalton Trans. 2007; (43):4893–4902. PMID:
17992274.

42. Horsman MR, Mortensen LS, Petersen JB, Busk M, Overgaard J. Imaging hypoxia to improve radiotherapy outcome. Nat Rev Clin Oncol. 2012; 9:674–687. PMID:
23149893.

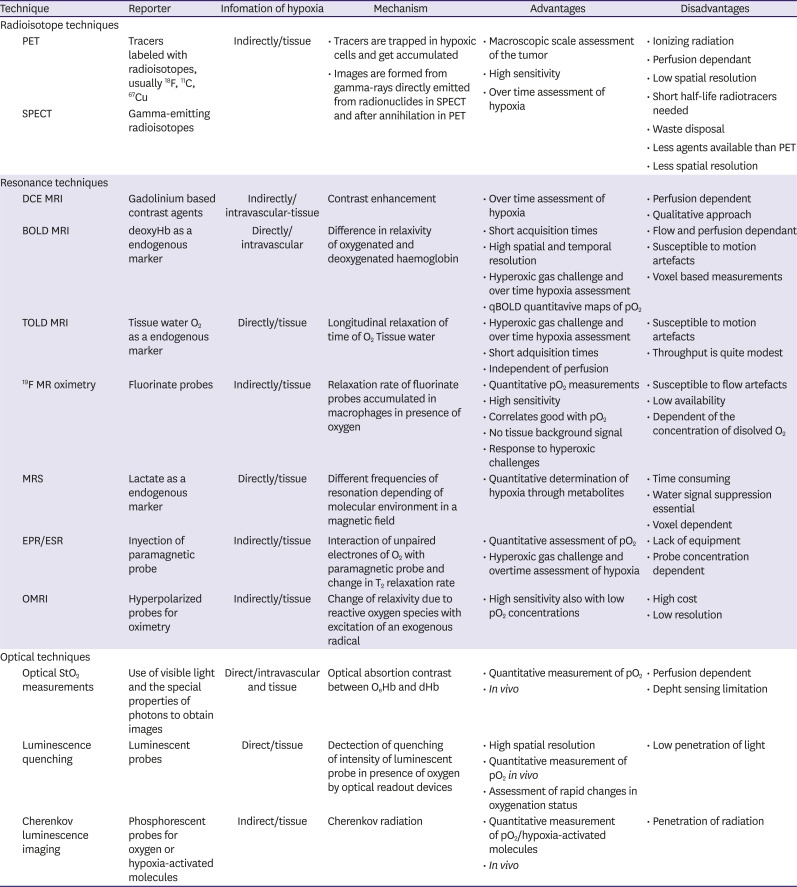
43. Challapalli A, Carroll L, Aboagye EO. Molecular mechanisms of hypoxia in cancer. Clin Transl Imaging. 2017; 5:225–253. PMID:
28596947.

44. Pinker K, Helbich TH, Morris EA. The potential of multiparametric MRI of the breast. Br J Radiol. 2017; 90:20160715. PMID:
27805423.

45. Jensen RL, Mumert ML, Gillespie DL, Kinney AY, Schabel MC, Salzman KL. Preoperative dynamic contrast-enhanced MRI correlates with molecular markers of hypoxia and vascularity in specific areas of intratumoral microenvironment and is predictive of patient outcome. Neuro-oncol. 2014; 16:280–291. PMID:
24305704.

46. Halle C, Andersen E, Lando M, Aarnes EK, Hasvold G, Holden M, et al. Hypoxia-induced gene expression in chemoradioresistant cervical cancer revealed by dynamic contrast-enhanced MRI. Cancer Res. 2012; 72:5285–5295. PMID:
22890239.

47. Baudelet C, Gallez B. How does blood oxygen level-dependent (BOLD) contrast correlate with oxygen partial pressure (pO
2) inside tumors? Magn Reson Med. 2002; 48:980–986. PMID:
12465107.
48. Christen T, Lemasson B, Pannetier N, Farion R, Remy C, Zaharchuk G, et al. Is T2* enough to assess oxygenation? Quantitative blood oxygen level-dependent analysis in brain tumor. Radiology. 2012; 262:495–502. PMID:
22156990.

49. Howe FA, Robinson SP, Rodrigues LM, Griffiths JR. Flow and oxygenation dependent (FLOOD) contrast MR imaging to monitor the response of rat tumors to carbogen breathing. Magn Reson Imaging. 1999; 17:1307–1318. PMID:
10576716.
50. Mason RP, Zhao D, Pacheco-Torres J, Cui W, Kodibagkar VD, Gulaka PK, et al. Multimodality imaging of hypoxia in preclinical settings. Q J Nucl Med Mol Imaging. 2010; 54:259–280. PMID:
20639813.
51. White DA, Zhang Z, Li L, Gerberich J, Stojadinovic S, Peschke P, et al. Developing oxygen-enhanced magnetic resonance imaging as a prognostic biomarker of radiation response. Cancer Lett. 2016; 380:69–77. PMID:
27267808.

52. Ding Y, Mason RP, McColl RW, Yuan Q, Hallac RR, Sims RD, et al. Simultaneous measurement of tissue oxygen level-dependent (TOLD) and blood oxygenation level-dependent (BOLD) effects in abdominal tissue oxygenation level studies. J Magn Reson Imaging. 2013; 38:1230–1236. PMID:
23749420.

53. O'Connor JP, Robinson SP, Waterton JC. Imaging tumour hypoxia with oxygen-enhanced MRI and BOLD MRI. Br J Radiol. 2019; 92:20180642. PMID:
30272998.
54. Maril N, Collins CM, Greenman RL, Lenkinski RE. Strategies for shimming the breast. Magn Reson Med. 2005; 54:1139–1145. PMID:
16217775.

55. Rakow-Penner R, Daniel B, Glover GH. Detecting blood oxygen level-dependent (BOLD) contrast in the breast. J Magn Reson Imaging. 2010; 32:120–129. PMID:
20578018.

56. Liu M, Guo X, Wang S, Jin M, Wang Y, Li J, et al. BOLD-MRI of breast invasive ductal carcinoma: correlation of R2* value and the expression of HIF-1α. Eur Radiol. 2013; 23:3221–3227. PMID:
23835924.

57. Choi HY, Ko ES, Han BK, Kim EJ, Kim SM, Lim Y, et al. Prognostic significance of transverse relaxation rate (R2*) in blood oxygenation level-dependent magnetic resonance imaging in patients with invasive breast cancer. PLoS One. 2016; 11:e0158500. PMID:
27384310.

58. Hunjan S, Zhao D, Constantinescu A, Hahn EW, Antich PP, Mason RP. Tumor oximetry: demonstration of an enhanced dynamic mapping procedure using fluorine-19 echo planar magnetic resonance imaging in the Dunning prostate R3327-AT1 rat tumor. Int J Radiat Oncol Biol Phys. 2001; 49:1097–1108. PMID:
11240252.

59. Zhao D, Jiang L, Hahn EW, Mason RP. Comparison of
1H blood oxygen level-dependent (BOLD) and
19F MRI to investigate tumor oxygenation. Magn Reson Med. 2009; 62:357–364. PMID:
19526495.
60. Le D, Mason RP, Hunjan S, Constantinescu A, Barker BR, Antich PP. Regional tumor oxygen dynamics: 19F PBSR EPI of hexafluorobenzene. Magn Reson Imaging. 1997; 15:971–981. PMID:
9322216.

61. Procissi D, Claus F, Burgman P, Koziorowski J, Chapman JD, Thakur SB, et al.
In vivo
19F magnetic resonance spectroscopy and chemical shift imaging of tri-fluoro-nitroimidazole as a potential hypoxia reporter in solid tumors. Clin Cancer Res. 2007; 13:3738–3747. PMID:
17575240.
62. Zhang C, Moonshi SS, Wang W, Ta HT, Han Y, Han FY, et al. High F-content perfluoropolyether-based nanoparticles for targeted detection of breast cancer by
19F magnetic resonance and optical imaging. ACS Nano. 2018; 12:9162–9176. PMID:
30118590.
63. Makela AV, Foster PJ. Imaging macrophage distribution and density in mammary tumors and lung metastases using fluorine-19 MRI cell tracking. Magn Reson Med. 2018; 80:1138–1147. PMID:
29327789.

64. Bartusik D, Tomanek B, Siluk D, Kaliszan R, Fallone G. The application of
19F magnetic resonance
ex vivo imaging of three-dimensional cultured breast cancer cells to study the effect of δ-tocopherol. Anal Biochem. 2009; 387:315–317. PMID:
19454246.
65. O'Flynn EA, DeSouza NM. Functional magnetic resonance: biomarkers of response in breast cancer. Breast Cancer Res. 2011; 13:204. PMID:
21392409.
66. Velan SS, Spencer RG, Zweier JL, Kuppusamy P. Electron paramagnetic resonance oxygen mapping (EPROM): direct visualization of oxygen concentration in tissue. Magn Reson Med. 2000; 43:804–809. PMID:
10861874.

67. Krohn KA, Link JM, Mason RP. Molecular imaging of hypoxia. J Nucl Med. 2008; 49(Suppl 2):129S–148S. PMID:
18523070.

68. Krishna MC, Matsumoto S, Yasui H, Saito K, Devasahayam N, Subramanian S, et al. Electron paramagnetic resonance imaging of tumor pO
2. Radiat Res. 2012; 177:376–386. PMID:
22332927.
69. Roussakis E, Li Z, Nichols AJ, Evans CL. Oxygen-sensing methods in biomedicine from the macroscale to the microscale. Angew Chem Int Ed Engl. 2015; 54:8340–8362. PMID:
26084034.

70. Shibata T, Giaccia AJ, Brown JM. Development of a hypoxia-responsive vector for tumor-specific gene therapy. Gene Ther. 2000; 7:493–498. PMID:
10757022.

71. Vordermark D, Shibata T, Brown JM. Green fluorescent protein is a suitable reporter of tumor hypoxia despite an oxygen requirement for chromophore formation. Neoplasia. 2001; 3:527–534. PMID:
11774035.

72. Harada H, Kizaka-Kondoh S, Hiraoka M. Optical imaging of tumor hypoxia and evaluation of efficacy of a hypoxia-targeting drug in living animals. Mol Imaging. 2005; 4:182–193. PMID:
16194450.

73. Blackmore KM, Knight JA, Walter J, Lilge L. The association between breast tissue optical content and mammographic density in pre- and post-menopausal women. PLoS One. 2015; 10:e0115851. PMID:
25590139.

74. Wang LV, Hu S. Photoacoustic tomography:
in vivo imaging from organelles to organs. Science. 2012; 335:1458–1462. PMID:
22442475.
75. Lungu GF, Li ML, Xie X, Wang LV, Stoica G.
In vivo imaging and characterization of hypoxia-induced neovascularization and tumor invasion. Int J Oncol. 2007; 30:45–54. PMID:
17143511.
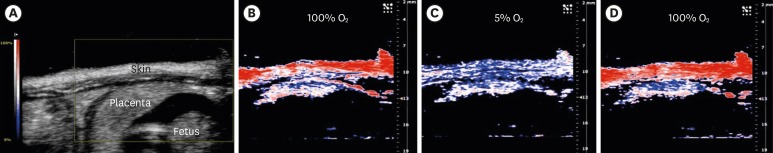
76. Arthuis CJ, Novell A, Raes F, Escoffre JM, Lerondel S, Le Pape A, et al. Real-time monitoring of placental oxygenation during maternal hypoxia and hyperoxygenation using photoacoustic imaging. PLoS One. 2017; 12:e0169850. PMID:
28081216.

77. Nam HS, Yoo H. Spectroscopic optical coherence tomography: a review of concepts and biomedical applications. Appl Spectrosc Rev. 2018; 53:91–111.

78. Reddy N, Nguyen BT. The utility of optical coherence tomography for diagnosis of basal cell carcinoma: a quantitative review. Br J Dermatol. 2019; 180:475–483. PMID:
30216419.

79. Neupane R, Gaudana R, Boddu SH. Imaging techniques in the diagnosis and management of ocular tumors: prospects and challenges. AAPS J. 2018; 20:97. PMID:
30187172.

80. Ha R, Friedlander LC, Hibshoosh H, Hendon C, Feldman S, Ahn S, et al. Optical coherence tomography: a novel imaging method for post-lumpectomy breast margin assessment-a multi-reader study. Acad Radiol. 2018; 25:279–287. PMID:
29174226.
81. Singla N, Dubey K, Srivastava V. Automated assessment of breast cancer margin in optical coherence tomography images via pretrained convolutional neural network. J Biophotonics. 2019; 12:e201800255. PMID:
30318761.

82. Schuman JS. Spectral domain optical coherence tomography for glaucoma (an AOS thesis). Trans Am Ophthalmol Soc. 2008; 106:426–458. PMID:
19277249.
83. Sandhu S, Kydd L, Jaworski J. Luminescent probe based techniques for hypoxia imaging. J Nanomed Res. 2017; 6:00160. PMID:
30417104.

84. Ciarrocchi E, Belcari N. Cerenkov luminescence imaging: physics principles and potential applications in biomedical sciences. EJNMMI Phys. 2017; 4:14. PMID:
28283990.

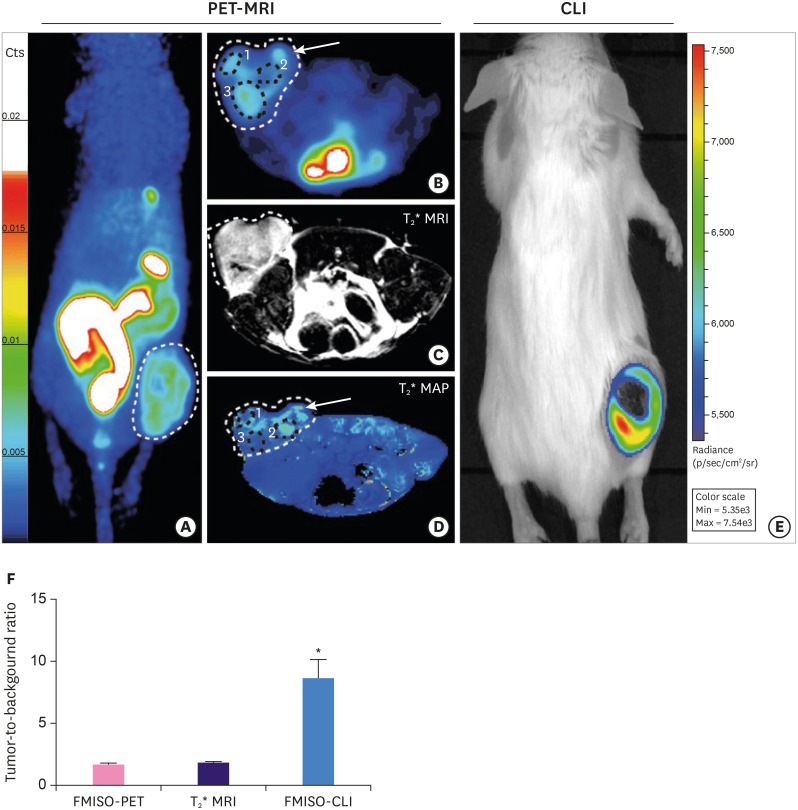
85. Desvaux E, Courteau A, Bellaye PS, Guillemin M, Drouet C, Walker P, et al. Cherenkov luminescence imaging is a fast and relevant preclinical tool to assess tumour hypoxia
in vivo. EJNMMI Res. 2018; 8:111. PMID:
30574662.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download