Abstract
Purpose
To report a case of optic neuritis accompanied by optic perineuritis after retinalamin peribulbar injection.
Case summary
A 46-year-old Kazakhstan woman presented with sudden vision loss, headache, and pain in both eyes which began 2 hours after the peribulbar injection of retinalamin approximately 10 days prior to her initial visit. At the initial visit, the best-corrected visual acuity was light perception in both eyes. A fundus examination showed bilateral optic disc swelling and fluorescein angiography showed late-phase leakage around the optic nerve and optic nerve sheath enhancement. On brain magnetic resonance imaging, the tram track sign and donut sign were seen in both eyes. Steroid pulse therapy was started after the diagnosis of optic neuritis accompanied by optic perineuritis. After 6 months, the patient's visual acuity improved up to 0.8 in the right eye and 1.0 in the left eye. The light reflex was recovered, the relative afferent pupillary defect decreased, and there was no evidence of optic disc swelling.
Figures and Tables
 | Figure 1Fundus fluorescein angiography (FAG) at late phase of both eyes and disc photography showing optic disc swelling. At initial presentation, (A) hyperfluorescence and late staining of the lesions with leakage from the optic disc. (B) Disc photography showing severe disc swelling. Three days after IV steroid pulse therapy, (C) decreased leakage from the optic disc and (D) clarified the margin of optic disc. |
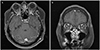 | Figure 2T1 post contrast fat suppression magnetic resonance images showing marked enhancement of the bilateral optic nerve sheath, (A) “tram track” sign and diffuse enhancement of optic nerve (arrows). (B) “donut sign” sign around optic nerve (arrowheads) (A, transverse view; B, coronal view). |
 | Figure 3Retinal nerve fiber layer (RNFL) thickness measurement with OCT, fundus disc photography, late phase fluorescein angiography (FAG) and humphrey visual fields test. (A) At initial presentation, RNFL thickness values exceed normal limit of both eye. The optic disc is swollen and margin of the optic disc is not clear. Late phase FAG showed leakage at optic disc. Visual field showed total defect. (B) Six months after IV steroid pulse therapy, RNFL thickness decreased under the normal limits of both eye, disc margin was finely defined but pale appearance at fundus photography and FAG. Visual field showed remained ceco-inferior scotoma. S = superior; N = nasal; I = inferior; T = temporal; TS = superotemporal; NS = superonasal; G = general; TI = inferotemporal; NI = inferonasal. |
References
1. Beck RW, Gal RL, Bhatti MT, et al. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. Am J Ophthalmol. 2004; 137:77–83.
2. Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Arch Neurol. 2008; 65:727–732.
3. Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol. 2001; 119:1299–1306.
4. Khavinson VK, Kuznik B, Ryzhak G. Peptide bioregulators: a new class of geroprotectors. Message 1: results of experimental studies. Adv Gerontol. 2013; 3:225–235.

5. Khavinson VK, Malinin V, Trofimova S, Zemchikhina VN. Inductive activity of retinal peptides. Bull Exp Biol Med. 2002; 134:482–484.
6. Frisén L. Swelling of the optic nerve head: a backstage view of a staging scheme. J Neuroophthalmol. 2017; 37:3–6.

7. Kennerdell JS, Dresner SC. The nonspecific orbital inflammatory syndromes. Surv Ophthalmol. 1984; 29:93–103.

8. Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the optic neuritis treatment trial. Arch Ophthalmol. 1991; 109:1673–1678.
9. Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL. Bradley's neurology in clinical practice e-book. 1st ed. Kidlington: Elsevier Health Sciences;2015. p. 163–178.
10. Edmunds W, Lawford J. Examination of optic nerve from cases of amblyopia in diabetes. Trans Ophthalmol Soc U K. 1883; 3:160–162.
11. Fay AM, Kane SA, Kazim M, et al. Magnetic resonance imaging of optic perineuritis. J Neuroophthalmol. 1997; 17:247–249.

12. Gordon LK. Orbital inflammatory disease: a diagnostic and therapeutic challenge. Eye (Lond). 2006; 20:1196–1206.

13. Lim HC, Choi HY, Choi JH, Jung JH. Clinical manifestations and treatment of idiopathic optic perineuritis. J Korean Ophthalmol Soc. 2014; 55:891–897.

14. Warren KG, Catz I, Shutt K. Optic neuritis anti-myelin basic protein synthetic peptide specificity. J Neurol Sci. 1992; 109:88–95.

15. Söderström M, Link H, Xu Z, Fredriksson S. Optic neuritis and multiple sclerosis: anti-MBP and anti-MBP peptide antibody-secreting cells are accumulated in CSF. Neurology. 1993; 43:1215–1222.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download