Abstract
Purpose
Intraocular lymphoma can be divided into primary and secondary usually involving B-cell lymphoma. Intraocular T-cell lymphoma is mostly secondary lymphoma while primary intraocular T-cell lymphoma is extremely rare. We report a case of primary T-cell lymphoma.
Case summary
A 62-year-old male without any systemic disease presented with a floater in the right eye. A fundus examination showed multiple whitish retinal infiltrations in the right eye. Intraocular lymphoma was suspected, and systemic examination was performed, but all results were normal. During steroid treatment, previous lesions were enlarged, new lesions developed, and a diagnosis of primary T-cell lymphoma was made by diagnostic vitrectomy. Consecutive intravitreal injections of methotrexate were performed. After eight injections, the vitreous and retinal lesions improved but we decided to terminate the injections due to corneal epitheliopathy. The corneal epitheliopathy was recovered and the patient is currently undergoing periodic follow-ups without progression of the lesion.
Figures and Tables
Figure 1
Fundus findings of a 62-year-old man with primary intraocular T-cell lymphoma. At the initial visit, fundus photography shows a vitreous opacity and retinal infiltrations (A, white arrow). Fluorescein angiography (FA) shows multiple hyperfluorescent dots (B, yellow arrows). Three months later, the lesions were aggravated. Previous lesions were enlarged, and the number of yellowish retinal infiltrations was increased (C, white arrows; D, yellow arrows). A new lesion developed in the inferotemporal area (C, red arrow). Inferotemporal lesion shows a leopard spot pattern on FA (D, green arrow).

Figure 2
Microscopic features of vitreous tap. Hematoxylin and eosin stain reveals scattered small T-lymphocytes (arrows) with macrophages (A, ×400). Immunohistochemical stain of vitreous shows positive for CD3 (B, ×400).

Figure 3
Consecutive findings of toxic keratopathy followed by multiple intravitreal methotrexate (MTX) injections for intraocular T-cell lymphoma. After 8 times intravitreal MTX injection, the patient demonstrated a severe corneal epitheliopathy (A, B). There were severe conjunctival injection, cystic change and limbal haziness causing the loss of palisades of Vogt (A). A month after treatment, the patient had improvement of his corneal epitheliopathy (C).
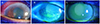
Figure 4
Fundus findings at 10 months after multiple intravitreal methotrexate injections. Fundus photograph shows atrophic and pigmentary changes corresponding to the previous infiltrates lesions (A). Fluorescein angiography (FA) shows a window defect with leopard spot pattern, and mild disk leakage in the late phase (B). Fundus autofluorescence (FAF) shows hypoautofluorescent dot and granular appearance. Hypoautofluorescent spots on FAF are hyperfluorescent on FA (C).

References
1. Hong JT, Chae JB, Lee JY, et al. Ocular involvement in patients with primary CNS lymphoma. J Neurooncol. 2011; 102:139–145.
2. Suh MH, Yu HG. Clinical manifestations of intraocular lymphoma. J Korean Ophthalmol Soc. 2009; 50:78–84.
3. Chaput F, Amer R, Baglivo E, et al. Intraocular T-cell lymphoma: clinical presentation, diagnosis, treatment, and outcome. Ocul Immunol Inflamm. 2017; 25:639–648.
4. Hunyor AP, Harper CA, O'Day J, McKelvie PA. Ocular-central nervous system lymphoma mimicking posterior scleritis with exudative retinal detachment. Ophthalmology. 2000; 107:1955–1959.
5. Saga T, Ohno S, Matsuda H, et al. Ocular involvement by a peripheral T-cell lymphoma. Arch Ophthalmol. 1984; 102:399–402.
6. Lobo A, Larkin G, Clark BJ, et al. Pseudo-hypopyon as the presenting feature in B-cell and T-cell intraocular lymphoma. Clin Exp Ophthalmol. 2003; 31:155–158.
7. Char DH, Ljung BM, Deschênes J, Miller TR. Intraocular lymphoma: immunological and cytological analysis. Br J Ophthalmol. 1988; 72:905–911.
8. Reddy EK, Bhatia P, Evans RG. Primary orbital lymphomas. Int J Radiat Oncol Biol Phys. 1988; 15:1239–1241.
9. Turaka K, Bryan JS, De Souza S, et al. Vitreoretinal lymphoma: changing trends in diagnosis and local treatment modalities at a single institution. Clin Lymphoma Myeloma Leuk. 2012; 12:412–417.
10. Hoffman PM, Mckelvie P, Hall AJ, et al. Intraocular lymphoma: a series of 14 patients with clinicopathological features and treatment outcomes. Eye (Lond). 2003; 17:513–521.
11. Whitcup SM, de Smet MD, Rubin BI, et al. Intraocular lymphoma. Clinical and histopathologic diagnosis. Ophthalmology. 1993; 100:1399–1406.
12. Sagoo MS, Mehta H, Swampillai AJ, et al. Primary intraocular lymphoma. Surv Ophthalmol. 2014; 59:503–516.
13. Smith JR, Rosenbaum JT, Wilson DJ, et al. Role of intravitreal methotrexate in the management of primary central nervous system lymphoma with ocular involvement. Ophthalmology. 2002; 109:1709–1716.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download