Abstract
Case summary
A 64-year-old male presented with abnormal color vision of the left eye, which occurred 6 months prior to his visit. At the initial visit, a funduscopic examination revealed retinal elevation with suspected serous retinal detachment around the optic disc in the left eye. Spectral domain optical coherence tomography showed subretinal fluid on the nasal side of the optic disc and retinoschisis on the temporal side of the optic disc in the left eye. Fluorescein angiography revealed multiple leakages in the left eye. Indocyanine green angiography revealed choroidal vascular hyperpermeability in both eyes. Based on these results, the patient was diagnosed with chronic central serous chorioretinopathy and was treated with argon laser photocoagulation at the leakage points. After 8 weeks of laser therapy, optical coherence tomography indicated that there was no retinoschisis or subretinal fluid in the macula, nasal, or temporal sides of the optic disc.
Figures and Tables
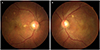 | Figure 1Color fundus photographs at initial visit. (A) Right eye shows retinal pigment epithelial degeneration around the macula. (B) Left eye shows edematous retina between the macula and the optic disc and retinal elevation on the nasal side of the optic disc. |
 | Figure 2Optical coherence tomography images of the left eye at initial visit. (A) Cross-sectional image of the optic nerve head shows subretinal fluid on the nasal side of the optic disc and retinoschisis on the temporal side of the optic disc. (B) Cross-sectional image of the macula by enhanced depth image (EDI) mode shows retinoschisis between the optic disc and the macula. The choroidal thickness was increased and the pachyvessels were observed predominantly between the optic disc and the macula. (C) Cross-sectional image of the optic nerve head by EDI mode. The lamina cribrosa was indicated between the anterior and posterior border of the highly reflective region that was visible beneath the optic disc cup. There was no lesion within the lamina cribrosa. |
 | Figure 3Fluorescein angiography (FAG) and indocyanine green angiography (ICGA) at initial visit. (A, B) FAG of the right eye shows multiple hyperfluorescent lesions. (C, D) FAG of the left eye shows multiple inkblot leakages. (E–H) Compared to the right eye, the ICGA of the left eye showed more dilated choroidal vasculature in the early phase and more patchy hyperfluorescence in the late phase. |
Notes
References
1. Ross A, Ross AH, Mohamed Q. Review and update of central serous chorioretinopathy. Curr Opin Ophthalmol. 2011; 22:166–173.

3. Zakir SM, Shukla M, Simi ZU, et al. Serum cortisol and testosterone levels in idiopathic central serous chorioretinopathy. Indian J Ophthalmol. 2009; 57:419–422.
4. Tittl MK, Spaide RF, Wong D, et al. Systemic findings associated with central serous chorioretinopathy. Am J Ophthalmol. 1999; 128:63–68.
5. Haimovici R, Koh S, Gagnon DR, et al. Risk factors for central serous chorioretinopathy: a case-control study. Ophthalmology. 2004; 111:244–249.
6. Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013; 58:103–126.
7. Lee EJ, Kim TW, Kim M, Choi YJ. Peripapillary retinoschisis in glaucomatous eyes. PLoS One. 2014; 9:e90129.
8. Jin SY, Song MR, Kim MK, Hwang YH. Peripapillary retinoschisis in non-glaucomatous eyes. J Korean Ophthalmol Soc. 2015; 56:80–85.
9. Hwang YH, Kim YY, Kim HK, Sohn YH. Effect of peripapillary retinoschisis on retinal nerve fibre layer thickness measurement in glaucomatous eyes. Br J Ophthalmol. 2014; 98:669–674.
10. Kahook MY, Noecker RJ, Ishikawa H, et al. Peripapillary schisis in glaucoma patients with narrow angles and increased intraocular pressure. Am J Ophthalmol. 2007; 143:697–699.
11. Fortune B, Ma KN, Gardiner SK, et al. Peripapillary retinoschisis in glaucoma: association with progression and OCT signs of Müller cell involvement. Invest Ophthalmol Vis Sci. 2018; 59:2818–2827.
12. Lee JH, Park HY, Baek J, Lee WK. Alterations of the lamina cribrosa are associated with peripapillary retinoschisis in glaucoma and pachychoroid spectrum disease. Ophthalmology. 2016; 123:2066–2076.
13. Phasukkijwatana N, Freund KB, Dolz-Marco R, et al. Peripapillary pachychoroid syndrome. Retina. 2018; 38:1652–1667.
14. Piccolino FC, De La Longrais RR, Manea M, Cicinelli S. Posterior cystoid retinal degeneration in central serous chorioretinopathy. Retina. 2008; 28:1008–1012.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download