Abstract
Despite the increasing number of osteochondral lesions of the talus, there are a lack of definite evidence-based treatment protocols. Several types of treatments are available, each having their advantages and disadvantages. First-line therapy consists of well-conducted conservative treatment. Surgical treatment is the second choice. Treatments are chosen based on the size of the lesion, location, chronicity, and the condition of the neighboring cartilage. This article reviews the current updates in the treatment of osteochondral lesions of the talus to help clinicians use the available treatment strategies more efficiently.
Figures and Tables
Figure 1
Bone marrow stimulation to the osteochondral lesion of talus. (A) Identification of the lesion. (B) Debridement of frayed or fibrillated cartilage. (C) Microfracture on subchondral plate. (D) Release of marrow elements from exiting perforations.
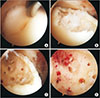
Figure 2
Retrograde drilling for the treatment of subchondral cyst. (A) Computed tomography (CT) image of subchondral cyst. (B) Arthroscopic image of intact overlying cartilage. (C) Retrograde drilling under fluoroscopy. (D) CT image at 12-month follow-up.

Figure 3
Use of matrix in the autologous chondrocyte implantation. (A) Debridement of the lesion. (B) Application of CartiFill® (Sewon Cellontech, Seoul, Korea).
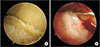
Figure 4
Autologous osteochondral transplacement to an osteochondral lesion of talus using the Osteochondral Autograft Transfer System® (Arthrex, Naples, FL, USA). (A) Identification of the lesion after medial malleolar osteotomy. (B) Debridement of damaged cartilage. (C) Harvest of autograft from the knee. (D) Insertion of autograft into the recipient hole in the talus.

References
1. Hintermann B, Regazzoni P, Lampert C, Stutz G, Gächter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br. 2000; 82:345–351. DOI: 10.1302/0301-620X.82B3.0820345.

2. Zengerink M, Szerb I, Hangody L, Dopirak RM, Ferkel RD, van Dijk CN. Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin. 2006; 11:331–359. viDOI: 10.1016/j.fcl.2006.03.008.

3. Gianakos AL, Yasui Y, Hannon CP, Kennedy JG. Current management of talar osteochondral lesions. World J Orthop. 2017; 8:12–20. DOI: 10.5312/wjo.v8.i1.12.

4. Steele JR, Dekker TJ, Federer AE, Liles JL, Adams SB, Easley ME. Osteochondral lesions of the talus: current concepts in diagnosis and treatment. Foot Ankle Orthop. 2018; 07. 27. DOI: 10.1177/2473011418779559. Published online.
5. Hannon CP, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, et al. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014; 96:164–171. DOI: 10.1302/0301-620X.96B2.31637.
6. Baums MH, Schultz W, Kostuj T, Klinger HM. Cartilage repair techniques of the talus: an update. World J Orthop. 2014; 5:171–179. DOI: 10.5312/wjo.v5.i3.171.

7. Smyth NA, Murawski CD, Fortier LA, Cole BJ, Kennedy JG. Platelet-rich plasma in the pathologic processes of cartilage: review of basic science evidence. Arthroscopy. 2013; 29:1399–1409. DOI: 10.1016/j.arthro.2013.03.004.

8. O'Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010; 38:392–404. DOI: 10.1177/0363546509336336.
9. Henkelmann R, Schmal H, Pilz IH, Salzmann GM, Dovi-Akue D, Südkamp NP. Prospective clinical trial of patients who underwent ankle arthroscopy with articular diseases to match clinical and radiological scores with intra-articular cytokines. Int Orthop. 2015; 39:1631–1637. DOI: 10.1007/s00264-015-2797-4.

10. Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006; 14:1119–1125. DOI: 10.1016/j.joca.2006.05.003.

11. Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G. Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation. Arthroscopy. 2006; 22:1085–1092. DOI: 10.1016/j.arthro.2006.05.016.

12. Choi JI, Lee KB. Comparison of clinical outcomes between arthroscopic subchondral drilling and microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016; 24:2140–2147. DOI: 10.1007/s00167-015-3511-1.

13. Chen H, Sun J, Hoemann CD, Lascau-Coman V, Ouyang W, McKee MD, et al. Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res. 2009; 27:1432–1438. DOI: 10.1002/jor.20905.

14. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008; 24:106–112. DOI: 10.1016/j.arthro.2007.07.022.

15. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009; 37:1974–1980. DOI: 10.1177/0363546509335765.
16. Choi WJ, Choi GW, Kim JS, Lee JW. Prognostic significance of the containment and location of osteochondral lesions of the talus: independent adverse outcomes associated with uncontained lesions of the talar shoulder. Am J Sports Med. 2013; 41:126–133. DOI: 10.1177/0363546512453302.

17. Lee KB, Park HW, Cho HJ, Seon JK. Comparison of arthroscopic microfracture for osteochondral lesions of the talus with and without subchondral cyst. Am J Sports Med. 2015; 43:1951–1956. DOI: 10.1177/0363546515584755.

18. Kelbérine F, Frank A. Arthroscopic treatment of osteochondral lesions of the talar dome: a retrospective study of 48 cases. Arthroscopy. 1999; 15:77–84.

19. Kumai T, Takakura Y, Higashiyama I, Tamai S. Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1999; 81:1229–1235. DOI: 10.2106/00004623-199909000-00004.

20. Becher C, Thermann H. Results of microfracture in the treatment of articular cartilage defects of the talus. Foot Ankle Int. 2005; 26:583–589. DOI: 10.1177/107110070502600801.

21. Choi WJ, Kim BS, Lee JW. Osteochondral lesion of the talus: could age be an indication for arthroscopic treatment? Am J Sports Med. 2012; 40:419–424. DOI: 10.1177/0363546511423739.
22. Kono M, Takao M, Naito K, Uchio Y, Ochi M. Retrograde drilling for osteochondral lesions of the talar dome. Am J Sports Med. 2006; 34:1450–1456. DOI: 10.1177/0363546506287300.

23. Anders S, Lechler P, Rackl W, Grifka J, Schaumburger J. Fluoroscopy-guided retrograde core drilling and cancellous bone grafting in osteochondral defects of the talus. Int Orthop. 2012; 36:1635–1640. DOI: 10.1007/s00264-012-1530-9.

24. van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, van Dijk CN. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am. 2013; 95:519–525. DOI: 10.2106/JBJS.L.00675.
25. Polat G, Erşen A, Erdil ME, Kızılkurt T, Kılıçoğlu Ö, Aşık M. Long-term results of microfracture in the treatment of talus osteochondral lesions. Knee Surg Sports Traumatol Arthrosc. 2016; 24:1299–1303. DOI: 10.1007/s00167-016-3990-8.

26. Baums MH, Heidrich G, Schultz W, Steckel H, Kahl E, Klinger HM. The surgical technique of autologous chondrocyte transplantation of the talus with use of a periosteal graft. Surgical technique. J Bone Joint Surg Am. 2007; 89:Suppl 2. (Pt.2):170–182. DOI: 10.2106/00004623-200709001-00002.

27. Nam EK, Ferkel RD, Applegate GR. Autologous chondrocyte implantation of the ankle: a 2-to 5-year follow-up. Am J Sports Med. 2009; 37:274–284. DOI: 10.1177/0363546508325670.
28. Mitchell ME, Giza E, Sullivan MR. Cartilage transplantation techniques for talar cartilage lesions. J Am Acad Orthop Surg. 2009; 17:407–414. DOI: 10.5435/00124635-200907000-00001.

29. Beris AE, Lykissas MG, Kostas-Agnantis I, Manoudis GN. Treatment of full-thickness chondral defects of the knee with autologous chondrocyte implantation: a functional evaluation with long-term follow-up. Am J Sports Med. 2012; 40:562–567. DOI: 10.1177/0363546511428778.

30. Harris JD, Siston RA, Brophy RH, Lattermann C, Carey JL, Flanigan DC. Failures, re-operations, and complications after autologous chondrocyte implantation--a systematic review. Osteoarthritis Cartilage. 2011; 19:779–791. DOI: 10.1016/j.joca.2011.02.010.

31. Giannini S, Buda R, Ruffilli A, Cavallo M, Pagliazzi G, Bulzamini MC, et al. Arthroscopic autologous chondrocyte implantation in the ankle joint. Knee Surg Sports Traumatol Arthrosc. 2014; 22:1311–1319. DOI: 10.1007/s00167-013-2640-7.

32. Kwak SK, Kern BS, Ferkel RD, Chan KW, Kasraeian S, Applegate GR. Autologous chondrocyte implantation of the ankle: 2- to 10-year results. Am J Sports Med. 2014; 42:2156–2164. DOI: 10.1177/0363546514540587.
33. Niemeyer P, Salzmann G, Schmal H, Mayr H, Südkamp NP. Autologous chondrocyte implantation for the treatment of chondral and osteochondral defects of the talus: a meta-analysis of available evidence. Knee Surg Sports Traumatol Arthrosc. 2012; 20:1696–1703. DOI: 10.1007/s00167-011-1729-0.

34. Lee KT, Lee YK, Young KW, Park SY, Kim JS. Factors influencing result of autologous chondrocyte implantation in osteochondral lesion of the talus using second look arthroscopy. Scand J Med Sci Sports. 2012; 22:510–515. DOI: 10.1111/j.1600-0838.2010.01262.x.

35. Brittberg M, Peterson L, Sjögren-Jansson E, Tallheden T, Lindahl A. Articular cartilage engineering with autologous chondrocyte transplantation. A review of recent developments. J Bone Joint Surg Am. 2003; 85-A:Suppl 3. 109–115. DOI: 10.2106/00004623-200300003-00017.
36. Giza E, Sullivan M, Ocel D, Lundeen G, Mitchell ME, Veris L, et al. Matrix-induced autologous chondrocyte implantation of talus articular defects. Foot Ankle Int. 2010; 31:747–753. DOI: 10.3113/FAI.2010.0747.

37. Schneider TE, Karaikudi S. Matrix-Induced Autologous Chondrocyte Implantation (MACI) grafting for osteochondral lesions of the talus. Foot Ankle Int. 2009; 30:810–814. DOI: 10.3113/FAI.2009.0810.

38. Aurich M, Bedi HS, Smith PJ, Rolauffs B, Mückley T, Clayton J, et al. Arthroscopic treatment of osteochondral lesions of the ankle with matrix-associated chondrocyte implantation: early clinical and magnetic resonance imaging results. Am J Sports Med. 2011; 39:311–319. DOI: 10.1177/0363546510381575.

39. Magnan B, Samaila E, Bondi M, Vecchini E, Micheloni GM, Bartolozzi P. Three-dimensional matrix-induced autologous chondrocytes implantation for osteochondral lesions of the talus: midterm results. Adv Orthop. 2012; 2012:942174. DOI: 10.1155/2012/942174.

40. Giannini S, Buda R, Grigolo B, Vannini F. Autologous chondrocyte transplantation in osteochondral lesions of the ankle joint. Foot Ankle Int. 2001; 22:513–517. DOI: 10.1177/7110070102200612.

41. Kennedy JG, Murawski CD. The treatment of osteochondral lesions of the talus with autologous osteochondral transplantation and bone marrow aspirate concentrate: surgical technique. Cartilage. 2011; 2:327–336. DOI: 10.1177/1947603511400726.

42. Kim YS, Park EH, Kim YC, Koh YG, Lee JW. Factors associated with the clinical outcomes of the osteochondral autograft transfer system in osteochondral lesions of the talus: second-look arthroscopic evaluation. Am J Sports Med. 2012; 40:2709–2719. DOI: 10.1177/0363546512461132.

43. Haleem AM, Ross KA, Smyth NA, Duke GL, Deyer TW, Do HT, et al. Double-plug autologous osteochondral transplantation shows equal functional outcomes compared with single-plug procedures in lesions of the talar dome: a minimum 5-year clinical follow-up. Am J Sports Med. 2014; 42:1888–1895. DOI: 10.1177/0363546514535068.

44. Emre TY, Ege T, Cift HT, Demircioğlu DT, Seyhan B, Uzun M. Open mosaicplasty in osteochondral lesions of the talus: a prospective study. J Foot Ankle Surg. 2012; 51:556–560. DOI: 10.1053/j.jfas.2012.05.006.

45. Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003; 85:Suppl 2. 25–32. DOI: 10.2106/00004623-200300002-00004.

46. Scranton PE Jr, Frey CC, Feder KS. Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br. 2006; 88:614–619. DOI: 10.1302/0301-620x.88b5.17306.

47. Valderrabano V, Leumann A, Rasch H, Egelhof T, Hintermann B, Pagenstert G. Knee-to-ankle mosaicplasty for the treatment of osteochondral lesions of the ankle joint. Am J Sports Med. 2009; 37:1_suppl. 105S–111S. DOI: 10.1177/0363546509351481.

48. Fraser EJ, Harris MC, Prado MP, Kennedy JG. Autologous osteochondral transplantation for osteochondral lesions of the talus in an athletic population. Knee Surg Sports Traumatol Arthrosc. 2016; 24:1272–1279. DOI: 10.1007/s00167-015-3606-8.

49. McGahan PJ, Pinney SJ. Current concept review: osteochondral lesions of the talus. Foot Ankle Int. 2010; 31:90–101. DOI: 10.3113/FAI.2010.0090.

50. Sammarco GJ, Makwana NK. Treatment of talar lesions using local osteochondral graft. Foot Ankle Int. 2002; 23:693–698. DOI: 10.1177/107110070202300803.
51. Yoon HS, Park YJ, Lee M, Choi WJ, Lee JW. Osteochondral autologous transplantation is superior to repeat arthroscopy for the treatment of osteochondral lesions of the talus after failed primary arthroscopic treatment. Am J Sports Med. 2014; 42:1896–1903. DOI: 10.1177/0363546514535186.

52. Fraser EJ, Savage-Elliott I, Yasui Y, Ackermann J, Watson G, Ross KA, et al. Clinical and MRI donor site outcomes following autologous osteochondral transplantation for talar osteochondral lesions. Foot Ankle Int. 2016; 37:968–976. DOI: 10.1177/1071100716649461.

53. Gaul F, Tírico LEP, McCauley JC, Bugbee WD. Long-term follow-up of revision osteochondral allograft transplantation of the ankle. Foot Ankle Int. 2018; 39:522–529. DOI: 10.1177/1071100717750578.

54. Enneking WF, Campanacci DA. Retrieved human allografts: a clinicopathological study. J Bone Joint Surg Am. 2001; 83:971–986. DOI: 10.2106/00004623-200107000-00001.
55. Enneking WF, Mindell ER. Observations on massive retrieved human allografts. J Bone Joint Surg Am. 1991; 73:1123–1142. DOI: 10.2106/00004623-199173080-00002.

56. Williams SK, Amiel D, Ball ST, Allen RT, Wong VW, Chen AC, et al. Prolonged storage effects on the articular cartilage of fresh human osteochondral allografts. J Bone Joint Surg Am. 2003; 85:2111–2120. DOI: 10.2106/00004623-200311000-00008.

57. Soomekh DJ. Using platelet-rich plasma in the foot and ankle. Foot Ankle Spec. 2010; 3:88–90. DOI: 10.1177/1938640010364483.

58. Mei-Dan O, Carmont MR, Laver L, Mann G, Maffulli N, Nyska M. Platelet-rich plasma or hyaluronate in the management of osteochondral lesions of the talus. Am J Sports Med. 2012; 40:534–541. DOI: 10.1177/0363546511431238.

59. Fortier LA, Barker JU, Strauss EJ, McCarrel TM, Cole BJ. The role of growth factors in cartilage repair. Clin Orthop Relat Res. 2011; 469:2706–2715. DOI: 10.1007/s11999-011-1857-3.

60. Smyth NA, Haleem AM, Murawski CD, Do HT, Deland JT, Kennedy JG. The effect of platelet-rich plasma on autologous osteochondral transplantation: an in vivo rabbit model. J Bone Joint Surg Am. 2013; 95:2185–2193. DOI: 10.2106/JBJS.L.01497.

61. Guney A, Yurdakul E, Karaman I, Bilal O, Kafadar IH, Oner M. Medium-term outcomes of mosaicplasty versus arthroscopic microfracture with or without platelet-rich plasma in the treatment of osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016; 24:1293–1298. DOI: 10.1007/s00167-015-3834-y.

62. Görmeli G, Karakaplan M, Görmeli CA, Sarikaya B, Elmali N, Ersoy Y. Clinical effects of platelet-rich plasma and hyaluronic acid as an additional therapy for talar osteochondral lesions treated with microfracture surgery: a prospective randomized clinical trial. Foot Ankle Int. 2015; 36:891–900. DOI: 10.1177/1071100715578435.

63. Castillo TN, Pouliot MA, Kim HJ, Dragoo JL. Comparison of growth factor and platelet concentration from commercial platelet-rich plasma separation systems. Am J Sports Med. 2011; 39:266–271. DOI: 10.1177/0363546510387517.

64. Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of leukocyte concentration on the efficacy of platelet-rich plasma in the treatment of knee osteoarthritis. Am J Sports Med. 2016; 44:792–800. DOI: 10.1177/0363546515580787.

65. Osterman C, McCarthy MB, Cote MP, Beitzel K, Bradley J, Polkowski G, et al. Platelet-rich plasma increases anti-inflammatory markers in a human coculture model for osteoarthritis. Am J Sports Med. 2015; 43:1474–1484. DOI: 10.1177/0363546515570463.

66. Cassano JM, Kennedy JG, Ross KA, Fraser EJ, Goodale MB, Fortier LA. Bone marrow concentrate and platelet-rich plasma differ in cell distribution and interleukin 1 receptor antagonist protein concentration. Knee Surg Sports Traumatol Arthrosc. 2018; 26:333–342. DOI: 10.1007/s00167-016-3981-9.

67. Fortier LA, Potter HG, Rickey EJ, Schnabel LV, Foo LF, Chong LR, et al. Concentrated bone marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. J Bone Joint Surg Am. 2010; 92:1927–1937. DOI: 10.2106/JBJS.I.01284.

68. Saw KY, Hussin P, Loke SC, Azam M, Chen HC, Tay YG, et al. Articular cartilage regeneration with autologous marrow aspirate and hyaluronic Acid: an experimental study in a goat model. Arthroscopy. 2009; 25:1391–1400. DOI: 10.1016/j.arthro.2009.07.011.

69. Hannon CP, Ross KA, Murawski CD, Deyer TW, Smyth NA, Hogan MV, et al. Arthroscopic bone marrow stimulation and concentrated bone marrow aspirate for osteochondral lesions of the talus: a case-control study of functional and magnetic resonance observation of cartilage repair tissue outcomes. Arthroscopy. 2016; 32:339–347. DOI: 10.1016/j.arthro.2015.07.012.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download