INTRODUCTION
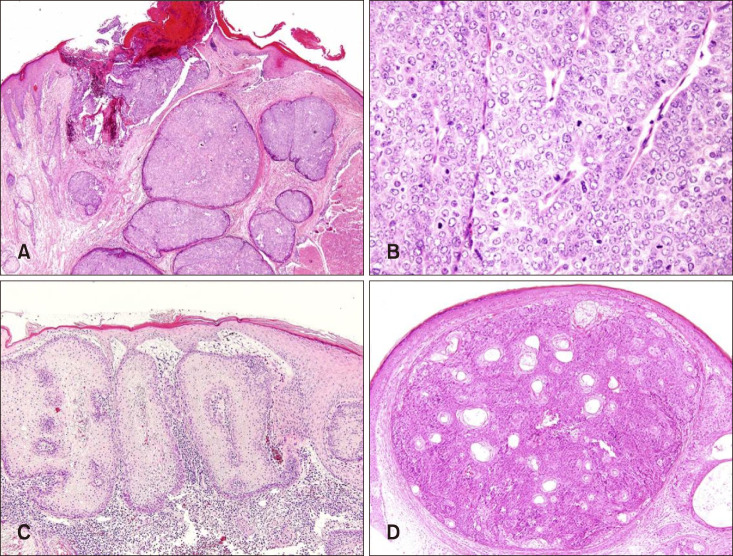
Sebaceous neoplasm is a rare subgroup of appendageal tumor that differentiates towards sebaceous adnexal structures of the skin. Appendageal tumors with sebaceous differentiation are widely classified into 3 subgroups according to the gradient of decreasing differentiation: (1) hyperplasias and hamartomas - nevus sebaceous and sebaceous hyperplasia, (2) benign neolplasms - sebaceous adenoma and sebaceoma and (3) malignant neoplasms - sebaceous carcinoma (SC)
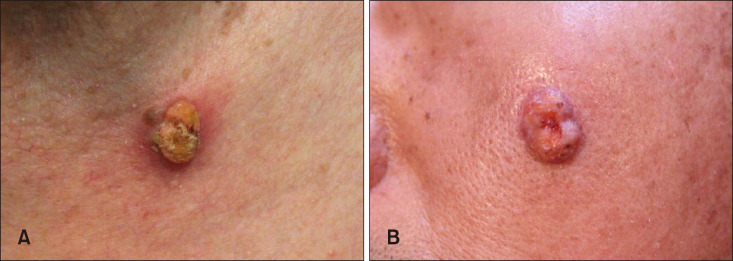
1. Sebaceous neoplasms may occur at any age but usually affect elderly population. These tumors most commonly present on the head and neck, and due to their heterogeneous clinical features, are often difficult to distinguish from other cutaneous neoplasms such as basal cell carcinoma and squamous cell carcinoma. Therefore, histopathologic examination is required for definitive diagnosis
2. Despite advances in understanding the histopathologic features of sebaceous neoplasms, relatively little is known about the clinical features of patients with sebaceous neoplasms, especially in those with benign sebaceous neoplasm (BSN). Additionally, sebaceous adenomas are known to be associated with visceral malignancy
1, However, there are few published studies assessing the clinical features of associated visceral malignancy such as the frequency and location in the patients with Muir-Torre syndrome (MTS) and there are no previous studies assessing associated visceral malignancy in patients with sebaceous neoplasm without MTS. Information regarding associated visceral malignancy in patients with sebaceous neoplasm would be helpful in the diagnosis of visceral malignancy considering that sebaceous neoplasms are visible lesions which can be easily diagnosed with skin biopsy.
Therefore, in this study we examined the basic demographic data, presenting clinical features and characteristics of associated visceral malignancies in Korean patients diagnosed with sebaceous neoplasms.
Go to :

MATERIALS AND METHODS
Study subjects
This retrospective case review was performed at two tertiary referral-based hospitals, Severance Hospital and Gangnam Severance Hospital, affiliated with Yonsei University Health System (YUHS). Consecutive patients who visited the departments of Dermatology and Ophthalmology between June 2007 and May 2017 who were histologically diagnosed as SC, sebaceous adenoma and sebaceoma were included and their medical records from the electronic health record (EHR) system of YUMC were reviewed.
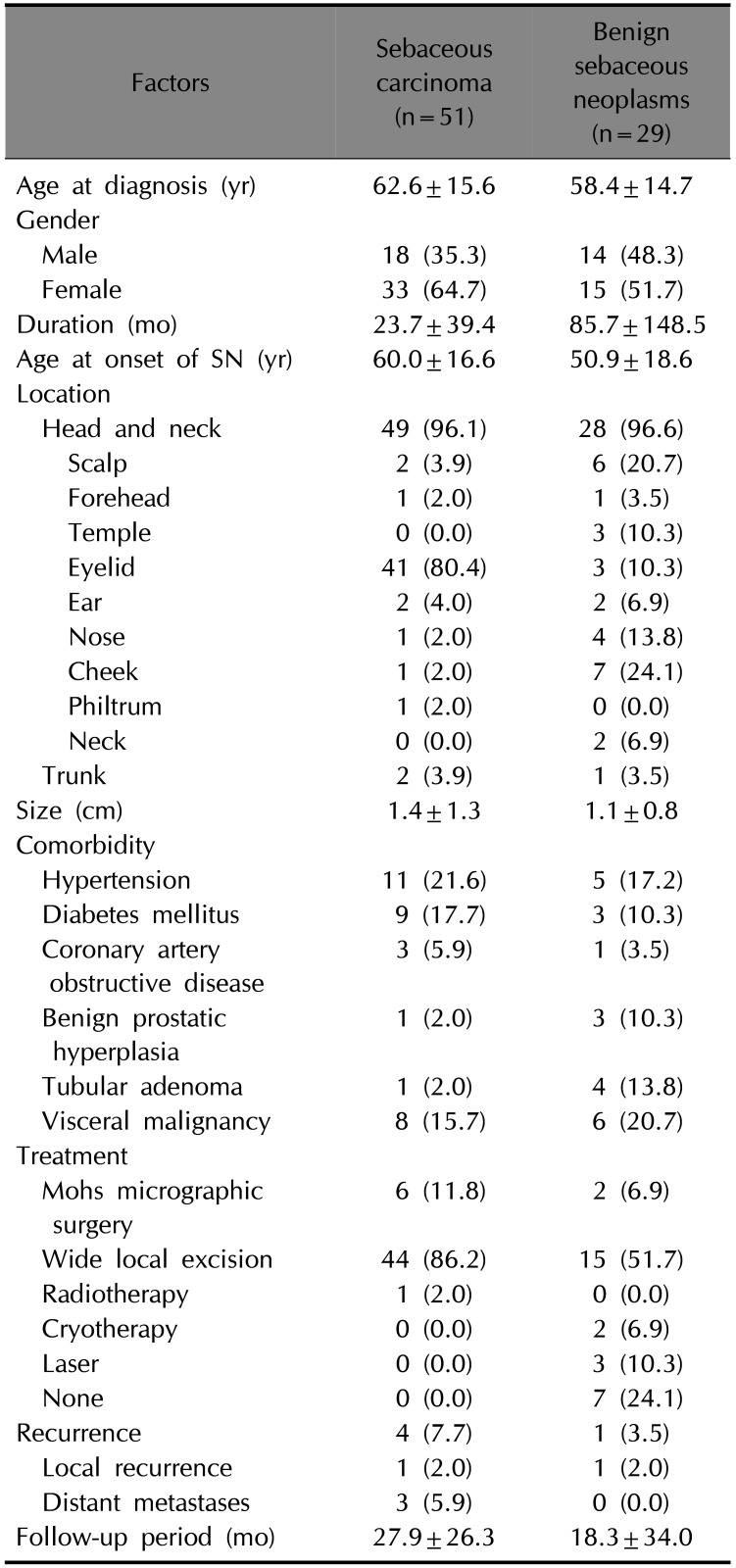
Analysis of clinical data
Patients were divided into two groups: the SC group and the BSN group, which included sebaceous adenomas and sebaceomas. We compared the basic clinical data obtained for all patients between the two groups including age, sex, duration, location of the primary tumor, tumor size, comorbidity, treatment, recurrence and presence of distant metastases. Among the patients with presence of associated visceral malignancies, we obtained and compared further additional clinical data including the age at diagnosis of visceral malignancies and the number of associated visceral malignancies. We received the patient's consent form about publishing all photographic materials.
Statistical analysis
The SC group and the BSN group were compared statistically. Statistical analyses were performed using SPSS software ver. 23.0 (IBM Co., Armonk, NY, USA). The results were expressed as means±standard deviations. The unpaired t-test was performed for continuous variables. To compare the categorical data, the chi-square test or the Fisher exact test was used. p-value<0.05 were considered to be statistically significant.
Ethics statement
This study was reviewed and approved by the Institutional Review Board of the Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea (IRB no. 3-2018-0014) and adhered to the tenets of the Declaration of Helsinki.
Go to :

DISCUSSION
Sebaceous neoplasms are widely classified into 3 types of tumors; SC, sebaceous adenomas and sebaceomas. SC is a rare malignant neoplasm of the sebaceous glands, commonly diagnosed in older adults and with no known gender predilections
3. SC is divided into extraocular and ocular types according to the location of the tumor. The ocular type, which is located on the periorbital area, account for 75% of SC
3. Typically, SC presents as a pink or yellow nodule or plaque. BSN includes sebaceous adenoma and sebaceoma. Sebaceous adenomas typically presents as solitary or multiple nodules less than 1 cm in size with tan, pink or yellow coloring. The clinical presentation of sebaceoma is not distinct, with appearance of papular, nodular, keratotic or ulcerated lesions. These two neoplasms are distinguished with histological features. Sebaceoma is diagnosed when it is composed with greater than 50% of germinative basaloid cells. Otherwise the diagnosis of sebaceous adenoma can be made
3. In this study, we sought to assess the clinical features of patients with SC and BSN. We also evaluated the incidence and clinical characteristics of associated visceral malignancies. In our study, the mean age at diagnosis was 62.6 years, which was at a younger age compared with previously published studies. Additionally, our results showed a female predilection (64.7%). The ocular type occupied 80.4% of the total SC, which was similar to previously published data. The differences in these results may be due to several factors. First, our data is based on the Korean population. According to Park et al.'s report
4, which analyzed the clinicopathologic data of Korean SC patients, the mean age of ocular SC was found to be 69.19 and extraocular SC was 67.46 which was also younger than other previously published studies based of other ethnic populations. This study also revealed a slight female predilection. Second, as SC is a rare tumor with a prevalence of 1 per 1,000,000, the total number of subjects and small differences may not be large enough to effectively power a statistically significant comparison. However, while further studies with larger number of subjects and multivariate analysis are needed, we believe our study is still meaningful and contributes significantly as there are not enough previously published statistical data regarding SC in Korean patients.
There is little currently known fact regarding BSN, with insufficient demographic data concerning BSN separatedly from SC. In our study, the mean age at diagnosis of BSN was 58.4 years and there were no gender predilections. The most common location of the tumors was the head and neck (96.6%), but only 3 cases (10.3%) occurred in the ocular area. Overall, we found no significant differences between the SC group and the BSN group except for the location of the tumors.
While the standard treatment for SC is WLE, recently, MMS has emerged as an adequate alternative treatment. Considering that location of SC is most frequently in cosmetically sensitive areas such as the eyelids and face, MMS would be advantageous because of its superior tumor margin control and preservation of normal skin. Furthermore, there are studies reporting that MMS has a lower local recurrence rate than WLE
567. We also consider WLE and MMS as first line treatments in our medical centers, and therefore in our study, surgical excision was the first line treatment except for one patient who was unable to undergo surgery. Among the 44 patients who were treated with WLE, only one patient showed local recurrence. There was no local recurrence in patients (n=6) who were treated with MMS.
MTS is a rare autosomal-dominant disorder characterized by the association of sebaceous gland tumors or other skin tumors with one or multiple visceral malignancies. The most commonly associated skin neoplasm is sebaceous adenoma with a frequency of 68%, followed by SC and sebaceoma
8. The most commonly associated visceral malignancy is colorectal adenocarcinoma. The diagnosis of MTS can be confirmed by immunohistochemistry on lesions which shows loss of staining for MMR gene products with high sensitivity
8.
However, detailed clinical data is sparse with few reports including the MTS portion of all patients with sebaceous neoplasms. Such information would be valuable for clinicians in guiding decisions on whether further evaluation for MTS should be required in patients with sebaceous neoplasm.
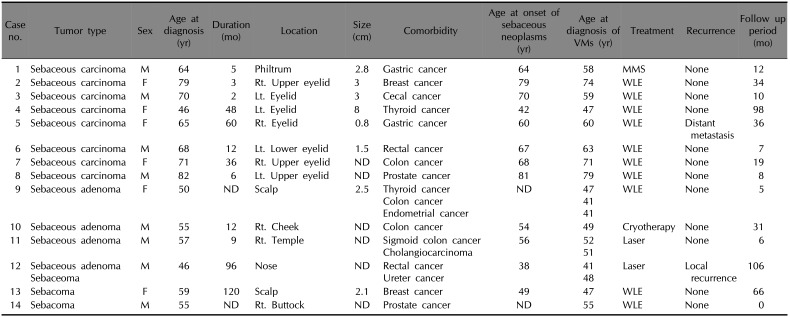
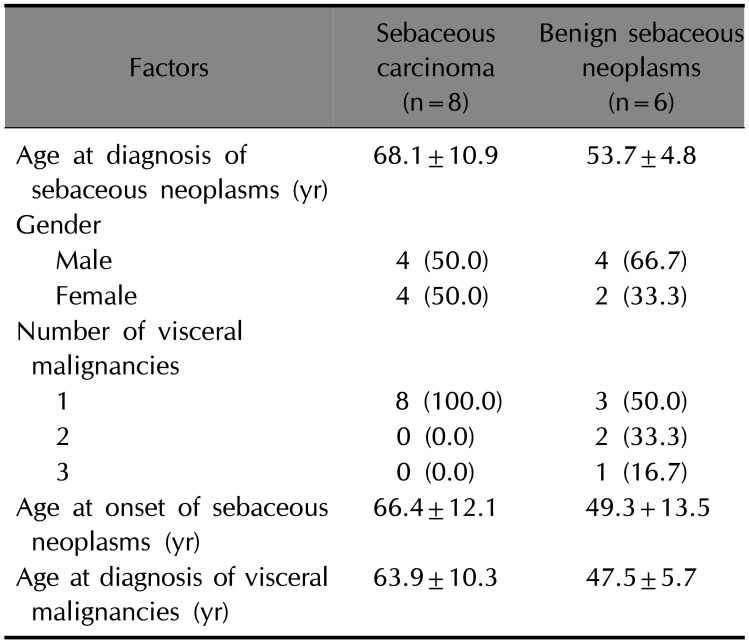
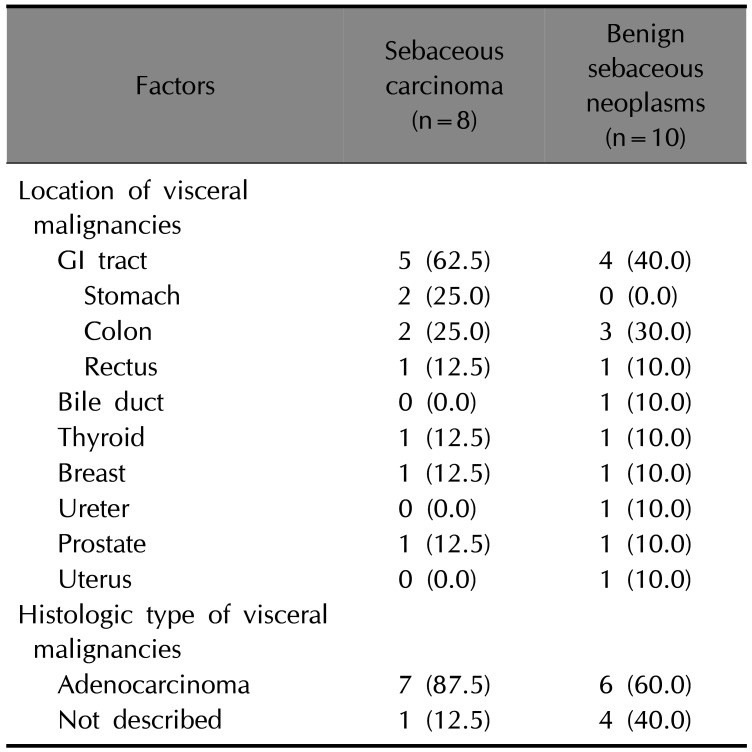
In our study, 14 patients (17.5%) were found to have associated visceral malignancies: 8 patients (15.7%) in the SC group and 6 patients (20.7%) in the BSN group. The proportion of patients associated with visceral malignancies is not statistically significant but is greater in the BSN group than in the SC group. Interestingly, SC group was also highly associated with visceral malignancy despite the lower incidence of SC associated with MTS compared with BSN
8. Among these patients, 3 patients in the BSN group (50.0%) had multiple visceral malignancies. Among the 18 visceral malignancies noted, 50% were of GI tract origin. According to the Korean National Cancer Center, the total cancer prevalence rate was 2.9%, with 0.6% and 0.5% prevalence rates in gastric cancers and colorectal cancers, respectively
9. Compared to this data, the patients in our study showed meaningfully high incidence rates of visceral malignancies, especially for GI tract cancers. However, patients with visceral malignancy would have had regular follow-up on outpatient clinic, and those with skin lesions would have been referred to the department of dermatology. This could be one of the reasons for a higher incidence of visceral malignancy in patients with sebaceous neoplasm. Additionally, in the BSN group, the mean age at diagnosis of visceral malignancy was 47.5 years; for the colorectal cancers, the mean age was 45.8 years. According to the American Cancer Society, colorectal cancer is commonly diagnosed after the age of 50 in the majority of people, with a similar tendency noted in Asian ethnic groups
10. When we compare these data, we note that the patients in our study developed visceral malignancies at a much younger age. We also checked the order of the incidence of sebaceous neoplasms and visceral malignancies in 14 patients. Although a distinct relationship was not found, the diagnosis of sebaceous neoplasms preceded that of visceral malignancy by 4.2 and 6.4 years in average in SC and BSN, respectively. In addition, among the 14 patients, 2 patients with SC had subsequently discovered visceral malignancy during the process of work-up for surgery of SC. These results suggest that screening for visceral malignancy, especially for the GI tract cancers, may be beneficial for patients with sebaceous neoplasms. Based on our results, we cautiously recommend immunohistochemistry for MMR gene products
811, and additionally, esophagogastroduodenoscopy or colonoscopy could be recommended for the patients with sebaceous neoplasms
12. Considering that sebaceous neoplasms are visible lesions which can be easily diagnosed with skin biopsy, it would be efficient if this process contribute to finding visceral malignancies.
This study has several limitations. First, it was a retrospective study with inherent limitations. Second, its study population was limited to Korean patients in a tertiary university hospital setting. Third, the number of subjects is small and may not effectively power statistical analysis for significance. Nevertheless, the strengths of this study are that it provides information regarding the clinical characteristics of previously little-known sebaceous neoplasms and associated visceral malignancies. In particular, this study suggests the necessity of screening for visceral malignancy, especially of the GI tract, in patients with sebaceous neoplasms.
Although further studies with a big sample sizes and additional studies about the efficacy of the screening for the visceral malignancies would be needed, we expect this study to contribute to comprehending and working-up of sebaceous neoplasms.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download