INTRODUCTION
Transnasal endoscopic marsupialization via inferior meatal antrostomy (IMA) and middle meatal antrostomy (MMA) is gaining popularity as a standard surgical method to treat postoperative maxillary mucocele. Although MMA is more physiologic, IMA is preferred because the mucocele is mostly located near the lower part of the lateral nasal wall, with bulging into the nasal cavity. Even with contracted and fibrotic sinus, which is common after the Caldwell-Luc (C-L) operation, IMA can be performed easily and effectively without major complications, such as bleeding, facial numbness, and nasolacrimal duct injury.1)2)3)4)5)
The authors experienced a rare case of facial neuralgia that developed after IMA to treat postoperative maxillary mucocele. The patient was successfully treated by surgically narrowing the IMA ostium. The diagnosis, surgical method, results, and possible pathophysiologic mechanism are discussed.
CASE REPORT
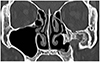
A 52-year-old woman reported a 6-year history of left-sided facial and ocular pain that developed after left-sided IMA to treat postoperative mucocele. She had undergone a C-L operation 20 years earlier. The pain was sharp and electric aggravated in cold air. When there's acute pain attack, visual analogue score (VAS) was 9 out of 10. Previously she had tried conservative treatment for years including pain reliever, intranasal ointment, and saline irrigation of nasal cavity which was unsuccessful. Anticonvulsant drug responded a little but couldn't keep taking it because of side effect. Instead, her nasal symptom was much relieved when the nostril was partially blocked with cotton pledget. She did not report other rhinologic symptoms, such as nasal obstruction, rhinorrhea, or hyposmia. Endoscopic examination showed a patent antrostomy inlet, about 1.0 cm in diameter, at the anterior-most part of the left inferior meatus. The shape and mucosa of inferior turbinate were intact, and the nasal cavity was normal. OMU computed tomography (CT) scan showed a contracted, small maxillary sinus due to new bone formation and fibrosis and a relatively large antrostomy (Fig. 1). The infraorbital nerve (ION) canal was sagging downward in the contracted sinus. Because she demonstrated pain relief with nasal blockage, we planned to narrow the IMA inlet to prevent cold air from directly entering and stimulating the sinus wall.
Operation (Fig. 2). An inferior vestibular incision was made in the left nostril from floor to lateral wall. The submucosal flap was elevated to the antrostomy inlet while preserving mucosa and skin integrity. Meticulous dissection was done around the antrostomy anteriorly, inferiorly, and superiorly. Harvested septal cartilage and conchal cartilage pieces were inserted into the submucosal pocket to obstruct the antrostomy inlet, with approximately 80% obstruction achieved.
The patient immediately noticed improvement of symptoms after the operation (VAS score from 9 to 2) and this improvement persisted thereafter. She could breathe painlessly even in cold weather without nostril blockage with much decreased pain. On endoscopic examination, well-maintained IMA inlet narrowing was observed at 6 months after operation (Fig. 3). We believe this is the first case report of successful treatment of facial neuralgia that developed after IMA.
DISCUSSION
Considering the character of the patient's pain—sharp, shock like, and sudden—we could assume that the pain is neuropathic in origin. Trigeminal neuralgia is uncommon disorder characterized by recurrent attacks of lancinating pain in the nerve distribution, and brief attacks are triggered by talking, chewing, teeth brushing, or cold breeze typically. 6) The pain is nearly always unilateral and occur repeatedly throughout the day. We supposed that cold air directly entering the sinus of the patient may have triggered neuralgic pain in the left side of the face. Although cold air is known as a common triggering factor for trigeminal neuralgia, the exact pathophysiologic mechanism of how the cold ambient air caused neuralgic pain in the left side of the patient's face is not clear.
The diagnosis is typically determined clinically, so the patient's history is the most critical in the evaluation although imaging studies may be necessary to rule out other disease.6) CT scan of this patient showed the ION sagging into the sinus during its course on the orbital floor, suggesting a possible clue to the neuralgic origin of the patient's pain. The ION travels anteriorly on the orbit floor through the thin infraorbital canal and exits from the infraorbital foramen into the face, reaching the skin. Not all sinus mucosa exposed to cold air would induce facial pain, but nerve irritation may happen, especially when the nerve is exposed from the canal. According to anatomic study, ION canal thickness is only 0.2 mm, and the incidence of partial or complete dehiscence of the infraorbital canal is between 12% and 20% in dry skull specimens.7)8)9) Moreover, unexpected variations of the nerve course in the maxillary sinus or canal dehiscence can increase the possibility of iatrogenic injury during C-L surgery. The mechanism of pain development by the dehiscent infraorbital canal is still unclear. But Facial pain in the distribution of the ION is often labelled “vacuum maxillay sinusitis” and treated empirically by intranasal antrostomy to enlarge the inlet.10) Some authors have suggested alterations in atmospheric pressure as a barotrauma, and others have suggested a vasodilation effect of the antral mucosal blood vessel.11)12) However, these assumptions are mostly related to small antral ostium size and do not correlate to our patient, who has a large IMA inlet. Sessle et al.13) suggested that the trigeminal primary afferent fibers terminated in the nasal mucosa as a free nerve ending were activated by noxious stimuli, including mechanical and chemical irritants.
Another possible factor contributing to neuralgic pain development in our case is the location and size of the IMA opening. IMA is usually performed at the inferior portion of the inferior meatus where the maxillary cyst that developed after C-L operation bulges most. Thus, the neo-ostium location depends on the location of the cyst in general. The IMA opening tends to become smaller with fibrotic changes of the opening, although the opening is large as created initially. Lund et al.5) reported that 53% of the IMA opening had closed with a mean follow-up time of 26 months, and adequate initial hole size should be as large as 1×2 cm to prevent its closure. In this case, the neo-ostium had remained mostly open at 6 years after surgery. In addition, it was located too anteriorly which inferior turbinate anterior head was not able to block it even after outfracture. This situation allowed non-humidified, cold air to easily enter the sinus and irritate exposed nerve. Our treatment of blocking the IMA inlet was based on these theories and was successful.
Blocking the IMA inlet with conchal cartilage graft via an endonasal approach is not technically challenging. However, the mucosa needs to be protected, and the ostium should not be destroyed to prevent recurrence of mucocele. An endoscope helped us to dissect precisely around the ostium and to place grafts exactly to surround the ostium. The initial narrowing of up to 80% of the ostium size was maintained at 6 months after surgery. Slight resorption of the cartilage with widening of the narrowed ostium is expected with time, and long-term follow-up is warranted.
CONCLUSION
We report a case of successful treatment of facial neuralgia that developed after IMA by endoscopically narrowing the ostium with cartilage graft. The neuralgia was triggered by cold air directly entering the maxillary sinus, and we believe that the exposed ION was a contributing factor in the neuralgia.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download