Abstract
Background and Objectives
Upper airway obstruction can occur at the soft palate, tongue base, or epiglottis among obstructive sleep apnea (OSA) patients. Detection of these obstruction sites is very important for choosing a treatment modality for OSA. The purpose of this study was to evaluate the obstruction site of OSA patients and its association with mouth opening and head position.
Subjects and Method
Forty-eight consecutive patients with suspicion of OSA were enrolled and underwent videofluoroscopy to evaluate the obstruction site, as well as polysomnography. Obstruction site, mouth opening, and head position were evaluated on videofluoroscopy, and their association was analyzed.
Results
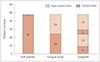
According to the videofluoroscopy, 47 (97.9%) of 48 patients showed an obstruction in the soft palate, while 24 (50.0%) were located in the tongue base and 14 (29.2%) in the epiglottis. Multiple obstructions were observed in many patients. Mean apnea-hypopnea index was higher among patients with tongue base obstruction (42.3±26.7) compared to those without obstruction (26.4±21.2, p=0.058). However, epiglottis obstruction did not influence apnea-hypopnea index. Mouth opening did not show any association with tongue base obstruction (p=0.564), while head flexion was highly associated (p<0.001).
Figures and Tables
 | Fig. 1A: Angle of head position. It is defined by the intersection of two lines. One connects the midpoint of the pituitary fossa to the nasion and the other line is posteriorly tangent to the cervical vertebra through the second and the fourth. B: Angle of mouth opening. It is formed by the intersection of lines drawn from the maxillary incisor to the glenoid fossa and from the glenoid fossa to the mandibular incisor. |
References
1. Owens RL, Eckert DJ, Yeh SY, Malhotra A. Upper airway function in the pathogenesis of obstructive sleep apnea: a review of the current literature. Curr Opin Pulm Med. 2008; 14:519–524.

2. Pang KP, Siow JK, Tseng P. Safety of multilevel surgery in obstructive sleep apnea: a review of 487 cases. Arch Otolaryngol Head Neck Surg. 2012; 138:353–357.

3. Pirklbauer K, Russmueller G, Stiebellehner L, Nell C, Sinko K, Millesi G, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea syndrome: a systematic review. J Oral Maxillofac Surg. 2011; 69:e165–e176.

4. Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010; 33:1396–1407.

5. Holty JE, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and metaanalysis. Sleep Med Rev. 2010; 14:287–297.

6. Stuck BA, Maurer JT. Airway evaluation in obstructive sleep apnea. Sleep Med Rev. 2008; 12:411–436.

7. Osnes T, Rollheim J, Hartmann E. Effect of UPPP with respect to site of pharyngeal obstruction in sleep apnoea: follow-up at 18 months by overnight recording of airway pressure and flow. Clin Otolaryngol Allied Sci. 2002; 27:38–43.

8. Aktas O, Erdur O, Cirik AA, Kayhan FT. The role of drug-induced sleep endoscopy in surgical planning for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2015; 272(8):2039–2043.

9. Huntley C, Chou D, Doghramji K, Boon M. Preoperative Drug Induced Sleep Endoscopy Improves the Surgical Approach to Treatment of Obstructive Sleep Apnea. Ann Otol Rhinol Laryngol. 2017; 126(6):478–482.

10. Kim JH, Chung TS, Kim NH, Seong SY, Lee GB, Kim KS. Relationship between Upper Airway Computed Tomography in the Awake State and Polysomnograpy in Obstructive Sleep Apnea Patients. J Rhinol. 2011; 18(1):20–28.
11. Choi JH, Jun YJ, Oh JI, Jung JY, Hwang GH, Yum GH, et al. Impact of Open-Mouth Breathing on Upper Airway Anatomy in Patients with Sleep-Disordered Breathing. J Rhinol. 2012; 19(1):55–59.
12. Jung H, Choi JM, Jeong YS, Hong SC, Kim JK, Cho JH. Analysis of snoring sound in obstructive sleep apnea patients based on obstruction site. Korean J Otorhinolaryngol-Head Neck Surg. 2012; 55:493–497.

13. Kim JS, Kim JK, Hong SC, Cho JH. Changes in the upper airway after counterclockwise maxillomandibular advancement in young Korean women with class II malocclusion deformity. J Oral Maxillofac Surg. 2013; 71:1603.e1–1603.e6.

14. Lee CH, Mo JH, Seo BS, Kim DY, Yoon IY, Kim JW. Mouth opening during sleep may be a critical predictor of surgical outcome after uvulopalatopharyngoplasty for obstructive sleep apnea. J Clin Sleep Med. 2010; 6:157–162.

15. Lee CH, Hong SL, Rhee CS, Kim SW, Kim JW. Analysis of upper airway obstruction by sleep videofluoroscopy in obstructive sleep apnea: a large population-based study. Laryngoscope. 2012; 122:237–241.

16. Lee SH, Choi JH, Shin C, Lee HM, Kwon SY, Lee SH. How does open-mouth breathing influence upper airway anatomy? Laryngoscope. 2007; 117(6):1102–1106.

17. Anegawa E, Tsuyama H, Kusukawa J. Lateral cephalometric analysis of the pharyngeal airway space affected by head posture. Int J Oral Maxillofac Surg. 2008; 37:805–809.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download