Abstract
Cases of simultaneously occurring medullary thyroid carcinoma (MTC) and lymphoma are extremely rare. An 84-year-old woman visited the hospital due to dyspnea, resulting from rapidly aggravated enlarged neck mass. Ultrasonography revealed two lesions in the thyroid and they were diagnosed as concurrent medullary thyroid carcinoma and diffuse large B cell lymphoma after total thyroidectomy. A few cases simultaneously diagnosed with MTC and systemic lymphoma have been reported. However, the coexistence of MTC and primary thyroid lymphoma is extremely rare.
Medullary thyroid carcinoma (MTC) and primary thyroid lymphoma (PTL) occupy small proportions of thyroid malignancies (MTC <2 to 3%, PTL <5%).1234) MTC can exhibit extensive local tumor growth, resulting in upper airway obstruction and dysphagia.1) PTL also can exhibit rapidly enlarging neck mass accompanied by hoarseness, dyspnea.1) The most common type of PTL is diffuse large B-cell lymphoma (DLBCL), followed by extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma).1) As mentioned above, PTL is rare and a few cases with concurrent papillary thyroid carcinoma (PTC) have been reported.5678) To the best of our knowledge, cases of simultaneously occurring MTC and lymphoma are extremely rare. Herein, we report a case of concurrent MTC and DLBCL in the thyroid.
An 84-year-old female visited the hospital due to dyspnea that developed 10 days previously, and a rapidly aggravated enlarged neck mass. She had a history of diabetes mellitus, hypertension, coronary 2 vessel disease, and severe dementia. Neck CT revealed about a 4.3×6.6×8.3 cm thyroid mass involving the left lobe, isthmus and medial portion of the right lobe and resulting in tracheal deviation to the right side without tracheal stenosis (Fig. 1A) Ultrasonography showed two lesions. The first lesion was a 1.64 cm sized, hypoechoic mass at the right upper pole (Fig. 1B), and the second lesion was a 6.85 cm sized hypoechogenic thyroid mass involving the left thyroid lobe, isthmus and medial portion of the right lobe with intrathoracic extension (Fig. 1C). Several enlarged lymph nodes were noted in the left neck level III, and level IV, but the lymph node image findings favored benign reactive hyperplasia. Laboratory findings showed normal thyroid hormone levels (T3: <0.40 ng/mL, fT4: 0.85 ng/dL, TSH: 1.02 uIU/mL), increased levels of procalcitonin (1.52 ng/mL) and slightly increased serum CEA levels (5.4 ng/mL). Ultrasound-guided needle biopsies were done on the lesions of both thyroid lobes. Based on the findings of the needle biopsy, the MTC and atypical lymphoid proliferation were suspected. Total thyroidectomy was done.
On the operative field, there was gross extension of the lesion to the esophagus, recurrent laryngeal nerve, tracheal, and sternothyroid muscle. The surgeon thought complete resection was unattainable, and he decided to perform a debulking total thyroidectomy, instead.
On the gross examination, the resected specimen
(Fig. 2A) revealed 2 lesions: (A), a well-demarcated ovoid, tan, yellowish solid mass at the right mid pole (1.2×1.1 cm) (Fig. 2B), and (B) a large solid mass with patchy or multinodular cut surface with ill define margin and focal necrosis (9×7 cm) involving almost the entire left lobe and extending to the right lobe (Fig. 2C). Microscopically, lesion of right mid pole was a relatively well-defined solid mass composed of plasmacytoid cells, and the tumor was transected by dense fibrous tissue (Fig. 3A [left] and 3B). Lesion of left lobe exhibited a relatively well-demarcated mass showing diffuse growth of large atypical cells with frequent mitoses and apoptotic bodies (Fig. 3A [right] and 3C, D). The diagnoses of MTC for mass of right lobe and high-grade lymphoma for lesion of left lobe were made. Further immunohistochemical studies were performed on both lesions. The mass of right lobe showed strong positivity for calcitonin (Fig. 4), and the mass of left lobe revealed strong reactivity for CD20 and MUM-1 with high proliferative index (90%) and are negative for Bcl-2, CD10, and Bcl-6 (Fig. 5A–F). Finally, diagnosis of concurrent medullary thyroid carcinoma and DLBCL was made. Besides the thyroid specimens, bilateral paratracheal lymph nodes were sent separately and shows partial involvement of malignant lymphoma in one paratracheal node (Fig. 6A, B).
After the surgery, the patient was discharged, according to the legal guardian's request. About three months later, patient was readmitted to the hospital due to general weakness and increased sputum. Chest CT showed tumor recurrence at the operative bed with direct invasion of the mediastinal structures and tracheo-esophageal fistula at the T2 level. Due to the tracheo-esophageal fistula, bronchoscopy was performed, and bronchial washing cytology revealed only necrotic inflammatory cells without malignant cells. Despite administration of antibiotics accompanied by conservative treatment, aspiration pneumonia developed, and the patient expired four months after the surgery.
MTC comprises less than 2 to 3% of thyroid malignancies, and PTL is less than 5 percent.1234) The most common histological type of PTL is non-Hodgkin's lymphoma. Considering the low incidences of both diseases in the thyroid, a combination of both malignancies in the thyroid would be very rare, unlike the combination of PTC and lymphoma.
According to the literature, six cases of co-occurring MTC and lymphoma have been described. Four cases of MTC coexisting with systemic lymphoma have been reported, including cases with Hodgkin's lymphoma in the bilateral neck nodes, splenic marginal zone lymphoma (SMZL), and mesenteric DLBCL and small lymphocytic lymphoma (SLL).391011) Two cases of SMZL and mesenteric DLBCL included MTC incidentally found on the work-up for lymphoma by 18F-fluorodeoxyglucose-positron emission tomography (F-18 FDG PET).39) The case with SLL (B-cell type) had a simultaneous occurrence of both medullary and papillary carcinomas of the thyroid gland with metastases of a papillary carcinoma.11) Two cases with MTC and lymphoma that developed metachronously also were reported; one case was diagnosed with MTC after treatment for Hodgkin's lymphoma, and the other case with MTC due to multiple endocrine neoplasia (MEN) type II, later developed mantle cell lymphoma.1213) Among the six cases diagnosed with both MTC and lymphoma, either synchronously or metachronously, only one case revealed thyroid involvement of the lymphoma.10) Yet, to our best knowledge, cases of simultaneously occurring MTC and PTL are rarely found. The six cases diagnosed with both MTC and lymphoma are shown in Table 1.
There should be some consideration whether DLBCL in this case could be of primary thyroid origin. It is reasonable that it is PTL with involvement of regional nodes, rather than systemic lymphoma involving the thyroid gland because the size of the DLBCL in the thyroid (9×7 cm in the largest cut section) was overwhelming and the lymph node was partially involved. Plus, the size of the involvement of the left paratracheal lymph node was relatively small, measuring 1.2 cm in the total size of 2 cm. Acosta-Ortega et al.10) reported a case in which, Hodgkin's lymphoma partially involved the thyroid, but the size of the neck dissection specimens were overwhelming (10×10×4 cm on the right side and 8×6×3 cm on the left side). In contrast, in our case, the size of the thyroid mass was overwhelming (9×7 cm), and the involved lymph node was small, which supports our opinion concerning the primary thyroid lymphoma.
One more point needs to be considered in this case. Considering the association of Hashimoto's thyroiditis (HT) with thyroid malignancy,14) it is possible that the patient in our case developed lymphoma from HT. However, the evidence for HT was not definitive, as almost entire thyroid was replaced by DLBCL. An association between HT and lymphoma, and between HT and PTC have been documented by previous studies. Specifically, Resende de Paiva et al.14) generated their association by a systematic review, and no association was found between HT and follicular, medullary, or anaplastic thyroid cancers.14) Nevertheless, a few cases of MTC developed in the background of HT have been reported, and some of them occurred on the background of MEN type II.151617)
In conclusion, a few cases have been reported of patients diagnosed with both MTC and lymphoma, however the coexistence of MTC and primary thyroid lymphoma is extremely rare. We present one such case here.
Figures and Tables
 | Fig. 1(A) Neck CT reveals about 4.3×6.6×8.3 cm thyroid mass involving the left lobe, isthmus and medial portion of the right lobe and resulting in tracheal deviation. (B, C) Thyroid ultrasonography reveals 1.64 cm sized, hypoechoic mass at the right upper pole (B) and on the left lobe, there is a 6.85 cm sized hypoechogenic mass (C), which shows extension to the isthmus, medial portion of the right lobe and intrathoracic area. |
 | Fig. 2(A) Specimen from total thyroidectomy. The right lobe measures 3×4.5×1.5 cm and the left lobe is markedly enlarged by the mass, measures 7×9×3.5 cm. (B) On cut section of right lobe, there is a well-circumscribed ovoid, tan, yellowish solid mass, measuring 1.2×1.1 cm. (C) Cut sections of left lobe of thyroid gland reveals multiple iirregular, patchy or nodular, gray lesions occupying almost entire left lobe and extending to the right lobe with focal necrosis. |
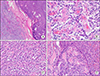 | Fig. 3(A) Border of medullary thyroid carcinoma (left side) abutting with primary thyroid lymphoma (right side). The left side reveals a well-defined solid mass (detailed view is presented in (B)), and the right side lesion shows diffuse growth pattern of lymphoid cells (detailed view is presented in (C)) (H&E, ×40). (B) The mass of right lobe consists of plasmacytoid cells on the fibrous background, suggesting medullary thyroid carcinoma (H&E, ×400). (C) The large lesion of left lobe shows diffuse growth of large atypical cells with frequent mitoses and apoptotic bodies (H&E, ×400). (D) At the peripheral portion of lesion in left lobe, destruction of thyroid follicles with infiltrate of large atypical lymphoid cells is noted (H&E, ×200). |
 | Fig. 4Immunohistochemical staining of medullary thyroid carcinoma. Right mid pole mass shows positivity for calcitonin (Calcitonin, ×200). |
 | Fig. 5Immunohistochemical staining of primary thyroid lymphoma. Mass shows diffuse strong positivity for CD20 (A, ×200). It shows 90% proliferative rate on Ki-67 (B, ×200). It is negative for Bcl-2 (C, ×200), Bcl-6 (D, ×200) and CD-10 (E, ×200). It is positive for MUM-1 (F, ×200). |
References
1. Lloyd RV, Osamura RY, Kloppel G, Rosai J. WHO classification of tumours of endocrine organs. WHO classification of tumors. 4th ed. International Agency for Research on Cancer (IARC);2017.
2. Ahmed M, Al-Saihati B, Greer W, Al-Nuaim A, Bakheet S, Abdulkareem AM, et al. A study of 875 cases of thyroid cancer observed over a fifteen-year period (1975-1989) at the King Faisal Specialist Hospital and Research Centre. Ann Saudi Med. 1995; 15(6):579–584.

3. Papajik T, Myslivecek M, Sedova Z, Buriankova E, Prochazka V, Raida L, et al. Synchronous second primary neoplasms detected by initial staging F-18 FDG PET/CT examination in patients with non-Hodgkin lymphoma. Clin Nucl Med. 2011; 36(7):509–512.

4. Catana R, Boila A, Borda A. Thyroid cancer profile in Mures County (Romania): a 20 years study. Rom J Morphol Embryol. 2012; 53(4):1007–1012.
5. Lan XB, Cao J, Zhu XH, Han Z, Huang YQ, Ge MH, et al. Concomitant papillary thyroid carcinoma and mucosa-associated lymphoid tissue thyroid lymphoma in the setting of Hashimoto thyroiditis. Int J Clin Exp Pathol. 2018; 11(6):3076–3083.
6. Cheng V, Brainard J, Nasr C. Co-occurrence of papillary thyroid carcinoma and primary lymphoma of the thyroid in a patient with long-standing Hashimoto’s thyroiditis. Thyroid. 2012; 22(6):647–650.

7. Shen G, Ji T, Hu S, Liu B, Kuang A. Coexistence of papillary thyroid carcinoma with thyroid MALT lymphoma in a patient with Hashimoto's thyroiditis: A clinical case report. Medicine (Baltimore). 2015; 94(52):e2403.
8. Mathai C, Ruby E. Case Report: Coexistence of papillary thyroid cancer and thyroid lymhoma. The Medicine Forum. 2018; 19:15–16.

9. Paschali A, Moonim M, Hubbard J, Mohan H. 18F-FDG PET detection of a medullary thyroid carcinoma in a patient with SMZL. Clin Nucl Med. 2016; 41(10):e447–e448.

10. Acosta-Ortega J, Montalban-Romero S, Garcia-Solano J, Sanchez-Sanchez C, Perez-Guillermo M. Simultaneous medullary carcinoma of the thyroid gland and Hodgkin's lymphoma in bilateral lymph nodes of the neck: a potential pitfall in fine-needle aspiration cytology. Diagn Cytopathol. 2004; 31(4):255–258.

11. Bocian A, Kopczynski J, Rieske P, Piaskowski S, Sluszniak J, Kupnicka D, et al. Simultaneous occurrence of medullary and papillary carcinomas of the thyroid gland with metastases of papillary carcinoma to the cervical lymph nodes and the coinciding small B-cell lymphocytic lymphoma of the lymph nodes--a case report. Pol J Pathol. 2004; 55(3):23–30.
12. Willard EM. Medullary carcinoma of the thyroid in a patient treated for Hodgkin's disease. Am J Med. 1990; 89(5):690.

13. Machaczka M. Mantle cell lymphoma successfully treated in a patient with multiple endocrine neoplasia type 2: a rare combination of two malignancies. Med Oncol. 2012; 29(3):2174–2175.

14. Resende de, Gronhoj C, Feldt-Rasmussen U, von Buchwald C. Association between Hashimoto's thyroiditis and thyroid cancer in 64,628 patients. Front Oncol. 2017; 7:53.

15. Dasgupta S, Chakrabarti S, Mandal PK, Das S. Hashimoto's thyroiditis and medullary carcinoma of thyroid. JNMA J Nepal Med Assoc. 2014; 52(194):831–833.

16. Gaskin D, Parai SK, Parai MR. Hashimoto's thyroiditis with medullary carcinoma. Can J Surg. 1992; 35(5):528–530.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download