1. Odvina CV, Zerwekh JE, Rao DS, et al. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005; 90:1294–1301.

2. Yang KH, Min BW, Ha YC. Atypical femoral fracture: 2015 Position statement of the Korean Society for Bone and Mineral Research. J Bone Metab. 2015; 22:87–91.

3. Allen MR, Burr DB. Three years of alendronate treatment results in similar levels of vertebral microdamage as after one year of treatment. J Bone Miner Res. 2007; 22:1759–1765.

4. Lenart BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med. 2008; 358:1304–1306.

5. Koh JS, Goh SK, Png MA, et al. Femoral cortical stress lesions in long-term bisphosphonate therapy: a herald of impending fracture? J Orthop Trauma. 2010; 24:75–81.

6. Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010; 25:2267–2294.

7. Unnanuntana A, Saleh A, Mensah KA, et al. Atypical femoral fractures: what do we know about them?: AAOS Exhibit Selection. J Bone Joint Surg Am. 2013; 95:e8 1–e8 13.
8. Aspenberg P, Schilcher J. Atypical femoral fractures, bisphosphonates, and mechanical stress. Curr Osteoporos Rep. 2014; 12:189–193.

9. Rizzoli R, Akesson K, Bouxsein M, et al. Subtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group Report. Osteoporos Int. 2011; 22:373–390.

10. Wang Z, Ward MM, Chan L, et al. Adherence to oral bisphosphonates and the risk of subtrochanteric and femoral shaft fractures among female medicare beneficiaries. Osteoporos Int. 2014; 25:2109–2116.

11. Koh JS, Goh SK, Png MA, et al. Distribution of atypical fractures and cortical stress lesions in the femur: implications on pathophysiology. Singapore Med J. 2011; 52:77–80.
12. Koeppen VA, Schilcher J, Aspenberg P. Dichotomous location of 160 atypical femoral fractures. Acta Orthop. 2013; 84:561–564.

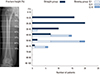
13. Schilcher J, Howe TS, Png MA, et al. Atypical fractures are mainly subtrochanteric in Singapore and diaphyseal in Sweden: A cross-sectional study. J Bone Miner Res. 2015; 30:2127–2132.

14. Sasaki S, Miyakoshi N, Hongo M, et al. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J Bone Miner Metab. 2012; 30:561–567.

15. Marcano A, Taormina D, Egol KA, et al. Are race and sex associated with the occurrence of atypical femoral fractures? Clin Orthop Relat Res. 2014; 472:1020–1027.

16. Oh Y, Wakabayashi Y, Kurosa Y, et al. Potential pathogenic mechanism for stress fractures of the bowed femoral shaft in the elderly: Mechanical analysis by the CT-based finite element method. Injury. 2014; 45:1764–1771.

17. Hyodo K, Nishino T, Kamada H, et al. Location of fractures and the characteristics of patients with atypical femoral fractures: analyses of 38 Japanese cases. J Bone Miner Metab. 2017; 35:209–214.

18. Kim JW, Kim JJ, Byun YS, et al. Factors affecting fracture location in atypical femoral fractures: a cross-sectional study with 147 patients. Injury. 2017; 48:1570–1574.

19. Oh Y, Fujita K, Wakabayashi Y, et al. Location of atypical femoral fracture can be determined by tensile stress distribution influenced by femoral bowing and neck-shaft angle: a CT-based nonlinear finite element analysis model for the assessment of femoral shaft loading stress. Injury. 2017; 48:2736–2743.

20. Chen LP, Chang TK, Huang TY, et al. The correlation between lateral bowing angle of the femur and the location of atypical femur fractures. Calcif Tissue Int. 2014; 95:240–247.

21. Soh HH, Chua IT, Kwek EB. Atypical fractures of the femur: effect of anterolateral bowing of the femur on fracture location. Arch Orthop Trauma Surg. 2015; 135:1485–1490.

22. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.

23. Park YC, Song HK, Zheng XL, et al. Intramedullary nailing for atypical femoral fracture with excessive anterolateral bowing. J Bone Joint Surg Am. 2017; 99:726–735.

24. Martelli S, Pivonka P, Ebeling PR. Femoral shaft strains during daily activities: implications for atypical femoral fractures. Clin Biomech (Bristol, Avon). 2014; 29:869–876.

25. Akman A, Demirkan F, Sabir N, et al. Femoral bowing plane adaptation to femoral anteversion. Indian J Orthop. 2017; 51:49–54.

26. Im GI, Jeong SH. Pathogenesis, management and prevention of atypical femoral fractures. J Bone Metab. 2015; 22:1–8.

27. Prasarn ML, Ahn J, Helfet DL, et al. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res. 2012; 470:2295–2301.

28. van de Laarschot DM, Smits AA, Buitendijk SK, et al. Screening for atypical femur fractures using extended femur scans by DXA. J Bone Miner Res. 2017; 32:1632–1639.

29. McKenna MJ, McKiernan FE, McGowan B, et al. Identifying incomplete atypical femoral fractures with single-energy absorptiometry: Declining prevalence. J Endocr Soc. 2017; 1:211–220.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download