1. Elfishawi MM, Zleik N, Kvrgic Z, Michet CJ Jr, Crowson CS, Matteson EL, et al. The rising incidence of gout and the increasing burden of comorbidities: a population-based study over 20 years. J Rheumatol. 2018; 45(4):574–579.

2. Kim JW, Kwak SG, Lee H, Kim SK, Choe JY, Park SH. Prevalence and incidence of gout in Korea: data from the national health claims database 2007–2015. Rheumatol Int. 2017; 37(9):1499–1506.

3. Smith E, Hoy D, Cross M, Merriman TR, Vos T, Buchbinder R, et al. The global burden of gout: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014; 73(8):1470–1476.

4. Kellgren JH, Jeffery MR, Ball J. The Epidemiology of Chronic Rheumatism. Oxford, United Kingdom: Blackwell Scientific Publications;1963.
5. Decker JL. Report from the subcommittee on diagnostic criteria for gout. In : In : Bennett PH, Wood PHN, editors. Population Studies of the Rheumatic Diseases. Proceedings of the Third International Symposium; 1966 Jun 5–10; New York, NY. Amsterdam, The Netherlands: Excerpta Medica Foundation;1968. p. 385–387.
6. Wallace SL, Robinson H, Masi AT, Decker JL, McCarty DJ, Yü TF. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977; 20(3):895–900.

7. Peláez-Ballestas I, Hernández Cuevas C, Burgos-Vargas R, Hernández Roque L, Terán L, Espinoza J, et al. Diagnosis of chronic gout: evaluating the American College of Rheumatology proposal, European League Against Rheumatism recommendations, and clinical judgment. J Rheumatol. 2010; 37(8):1743–1748.

8. Janssens HJ, Fransen J, van de Lisdonk EH, van Riel PL, van Weel C, Janssen M. A diagnostic rule for acute gouty arthritis in primary care without joint fluid analysis. Arch Intern Med. 2010; 170(13):1120–1126.

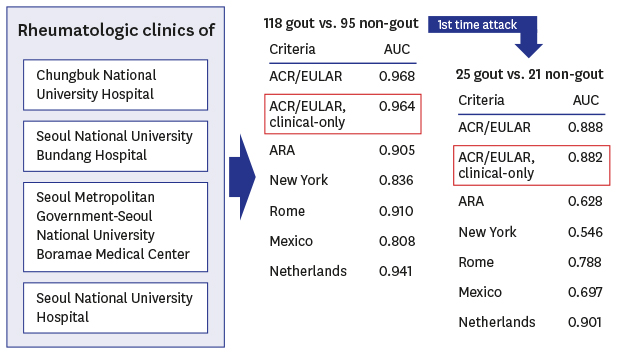
9. Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D, et al. 2015 Gout Classification Criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2015; 74(10):1789–1798.

10. Taylor WJ, Fransen J, Jansen TL, Dalbeth N, Schumacher HR, Brown M, et al. Study for Updated Gout Classification Criteria (SUGAR): identification of features to classify gout. Arthritis Care Res (Hoboken). 2015; 67(9):1304–1315.
11. Janssens HJ, Fransen J, Janssen M, Neogi T, Schumacher HR, Jansen TL, et al. Performance of the 2015 ACR-EULAR classification criteria for gout in a primary care population presenting with monoarthritis. Rheumatology (Oxford). 2017; 56(8):1335–1341.

12. Louthrenoo W, Jatuworapruk K, Lhakum P, Pattamapaspong N. Performance of the 2015 American College of Rheumatology/European League Against Rheumatism gout classification criteria in Thai patients. Rheumatol Int. 2017; 37(5):705–711.

13. Taylor WJ, Fransen J, Dalbeth N, Neogi T, Ralph Schumacher H, Brown M, et al. Diagnostic arthrocentesis for suspicion of gout is safe and well tolerated. J Rheumatol. 2016; 43(1):150–153.

14. Berendsen D, Neogi T, Taylor WJ, Dalbeth N, Jansen TL. Crystal identification of synovial fluid aspiration by polarized light microscopy. An online test suggesting that our traditional rheumatologic competence needs renewed attention and training. Clin Rheumatol. 2017; 36(3):641–647.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download