Abstract
Purpose
To investigate the rate of neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy in the hydroimplantation intraocular lens (IOL) technique.
Methods
This retrospective study was comprised of 6,192 eyes in 3,790 patients who underwent surgery from January 2013 to September 2017 and then were followed up for at least 1 year. The eyes of these patients were divided into two groups: either viscoimplantation or hydroimplantation. The follow-up examinations were carried out on the 1st day, 4th day, 1st month, and 3 months to 1 year postoperatively. The Nd:YAG capsulotomy rates were evaluated by the different IOL implantation techniques and IOL materials.
Results
The mean follow-up duration of the patients was in the viscoimplantation group 14.85 ± 2.43 and 15.05 ± 1.93 months in the hydroimplantation group. The Nd:YAG capsulotomy rate was significantly lower in the hydroimplantation group compared with the viscoimplantation group for the entire hydrophilic IOL model (p < 0.001). In addition, the Nd:YAG rate was lower in the hydroimplantation group that used a hydrophilic IOL than it was in the viscoimplantation group, which used a hydrophobic IOL.
Posterior capsular opacification (PCO) remains the most frequent complication of cataract surgery despite the development of preventative surgical techniques and several different types of intraocular lenses (IOLs) [1]. This complication can occur in up to 50% of eyes from a few months after to many years following cataract extraction. The incidence and severity of PCO correlate to many factors, including surgical technique, IOL materials, IOL designs, patient age, ocular or systemic disease, and drug use [2].
PCO results from metaplasia of lens e pithelial c ells (LECs) that remain after cataract surgery; LECs may proliferate, transform into fibroblasts, or migrate behind the optic of the IOL implant a few months to a few years after an uneventful cataract surgery [3]. Inflammatory mediators (interleukin 1, interleukin 6, and tumor necrosis factor) and complement activation stimulate LEC proliferation [4]. An inflammatory response may be exacerbated by the presence of the IOL, a foreign material.
With the recognition of the role of the LECs in PCO, many techniques have been developed that are directed at removing residual cells during cataract surgery. These include simple aspiration, capsule polishing, cryocoagulation, ultrasound aspiration, and osmolysis [5]. The fact that none of these techniques has been utilized as a routine surgical procedure reflects the difficulty of completely removing all LECs.
The hydroimplantation technique for inserting a foldable IOL without viscoelastic was first described by Tak [6]. In this method, only the irrigation cannula from the side port is used to form the capsular bag and anterior chamber to allow for implantation of the IOL; viscoelastic is not required. In this study, we investigated the rate of neodymium-doped yttrium aluminum garnet (Nd:YAG) laser used to treat PCO in the hydroimplantation IOL technique.
Patients with uneventful cataract surgeries and no postoperative complications who underwent surgery at Kırıkkale University Medical Faculty Department of Ophthalmology, Kırıkkale, Turkey, were included in this retrospective observational clinical study. The study was approved by the institutional review board at our institution (2018-11-04) and was conducted in accordance with the Declaration of Helsinki. The written informed consent was waived because this study is retrospective.
All patient files were retrospectively reviewed. Patients who underwent surgery from January 2013 to September 2017 and were followed up for at least one year were included in the study. Exclusion criteria were complicated intraoperative cases with posterior capsular rupture, eyes with ocular preoperative associated inflammatory pathology (uveitis) or trauma, and complicated postoperative cases with endophthalmitis or inflammation of a different etiology.
All surgeries were performed under topical anesthesia by two surgeons (OT and ÖK) with ultrasound technology (Pentasys 2, Germany). The eyes of the patients were divided into two groups: the viscoimplantation and hydroimplantation groups. In both groups, a two-sided port and a main temporal incision were used in all eyes. Following the injection of viscoelastic in both groups, continuous curvilinear capsulorhexis, hydrodissection, phacoemulsification of the nucleus, and cortex aspiration were performed. The anterior and posterior lens capsule was mechanically polished as a standard technique. In the hydroimplantation group, no viscoelastic was injected into the eye. The IOL was then loaded onto a cartridge with a predetermined amount of balanced salt solution. Next, the irrigation cannula was introduced into the anterior chamber through a left side of the port with irrigation. After the tip of the cartridge was inserted into the main port in the direction of the capsular bag, the IOL was slowly introduced. The aspiration cannula was placed through the other side port, and then the optic and haptic were introduced into the capsular bag by pressing lightly on the bimanual cannula. In the viscoimplantation group, the capsular bag was expanded with an assigned viscoelastic agent, and the foldable acrylic IOL was implanted into the capsular bag. The viscoelastic material was aspirated completely from the anterior chamber, the capsule fornix, and the retrolental space through bimanual irrigation/aspiration using what is called the two-compartment technique. Finally, in both groups, all corneal incisions were hydrated. Each patient received a posterior chamber IOL that was either spherical or aspheric and either hydrophilic or hydrophobic.
All patients experienced the same postoperative treatment: non-steroid anti-inflammatory drugs and an antibiotic and steroid combination five times a day for 2 weeks followed by steroid and non-steroid anti-inf lammatory drug drops four times a day for another 2 weeks.
The follow-up examinations were scheduled on the 1st day, 4th day, 1st month, and between the 3rd month up to 1 year postoperatively depending on the patient's ocular status. Further examinations (at every 3, 6, or 12 months) up to after more than 3 years of follow-up were scheduled based upon the ocular features or due to the physician's requests or the patients' visual complaints/demands.
The best-corrected visual acuity (BCVA) was assessed along with a biomicroscopic examination at each subsequent visit; tonometry was also performed. The PCO was evaluated subjectively with the retro-illumination of a slit lamp. PCO was considered when Elschnig' pearls or fibrosis were noted on the posterior capsule and corresponded to the capsulorhexis opening.
Nd:YAG laser treatment was performed when the BCVA decreased by at least 20% due to PCO occurrence. The Nd:YAG rates were evaluated for the different IOL implantation techniques and IOL materials included in the present study.
Statistical analysis was performed using the SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Pearson chi-squared tests were applied to compare the rates for hydrophilic/hydrophobic and spherical/aspheric IOLs. Statistical significance was considered when p < 0.05.
We enrolled 6,192 eyes of 3,790 patients in this study. The participants included 1,893 female (mean age, 71.49 ± 10.37 years) and 1,897 male (mean age, 68.56 ± 10.31 years). The difference between the two groups was not statistically significant in terms of age or sex (p > 0.05). The mean follow-up duration of the patients in the viscoimplantation and hydroimplantation groups were 14.85 ± 2.43 and 15.05 ± 1.93 months, respectively. The demographic characteristics of the patients are shown in Table 1.
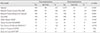
The type of PCO was 43.9% Elschnig's pearls and 55.1% f ibrosis in the hydroimplantation group and 53.8% Elschnig's pearls and 46.2% fibrosis in the viscoimplantation group. There was no statistically significant difference between the two groups in terms of PCO type (p = 0.115). Pre- and post-capsulotomy BCVA values were 0.485 ± 0.255 and 0.943 ± 0.943 in the hydroimplantation group and 0.416 ± 0.315 and 0.916 ± 0.335 in the viscoimplantation group, respectively. Overall, 95% of the eyes were implanted with hydrophilic IOLs. The Nd:YAG capsulotomy rates were significantly lower in eyes implanted with hydrophobic IOLs than in those that received hydrophilic IOLs (p < 0.001). Table 2 shows the number of eyes included in each of the two groups according to IOL model.
In addition, the Nd:YAG capsulotomy rate was significantly lower in the hydroimplantation group when compared with the viscoimplantation group for the entire hydrophilic IOL model (p < 0.001). The Nd:YAG rate was also lower in the hydroimplantation group with hydrophilic IOLs than it was in the viscoimplantation group with hydrophobic IOLs (p < 0.001). Fig. 1 shows the Nd:YAG rates for all IOL types and models.
The results of the present study demonstrate a low Nd:YAG capsulotomy rate in patients who underwent phacoemulsification and hydroimplantation using the IOL technique. Our results confirmed the previous results of studies [78] that reported lower incidence proportions of the Nd:YAG capsulotomy rate for hydrophobic acrylic IOLs than for hydrophilic acrylic IOLs.
The main reason for the development of PCO is a combination of the processes of proliferation, migration, and transdifferentiation of residual LECs on the lens capsule, which commonly occurs after cataract surgery [9]. There are two morphological types of PCO: the fibrosis type and the pearl type. The pathogenesis of the fibrosis type is the proliferation and migration of LECs, which undergo an epithelial-to-mesenchymal transition. Pearl-type PCO is caused by subcapsular LECs located at the lens bow, which cause regeneration of crystallin-expressing lenticular fibers and form Elschnig pearls.
Complete lens extractions should include the removal of residual LECs, but sometimes this ideal may not be possible. Even small amounts of residual LECs may lead to PCO development; therefore, complete removal of the LECs is essential [10]. Previous studies have also shown that phacoemulsification and cortical irrigation and aspiration lead to less residual concentrations of LECs on the inner surfaces of the capsules than extracapsular cataract extraction [11]. Nishi and Nishi [12] reported that phacoemulsification significantly reduced the need for laser capsulotomy when compared to extracapsular cataract extraction (10.8% vs. 3.7%, respectively). In addition, the continuous curvilinear capsulorhexis used in phacoemulsification reduces the amount of capsular space available for the proliferation and migration of any residual LECs [13].
The definitive solution intended to prevent PCO is to remove all epithelial cells from the capsular bag. Therefore, the intraoperative removal of the LECs from the capsular bag is becoming increasingly important in cataract surgery. Several prior studies have investigated the rates of formation of PCO using various surgical techniques, including hydrodissection combined with rotation, cortical cleaving hydrodissection, in-the-bag IOL fixation, anterior capsule overlap of the IOL optic, and polishing (scraping) the anterior capsule [1415161718]. In other words, many methods have been tried to prevent the formation of PCO which often causes a second process. The hydroimplantation may be an alternative method for this purpose.
The hydroimplantation technique is an improved method for avoiding negative conditions associated with viscoelastic material, such as postoperative inflammation and intraocular pressure elevation [6]. Several studies have reported its safety using the mean of postoperative endothelial cell density [1920].
In this study, we found that the hydroimplantation technique has the lowest rate of PCO development out of all the different hydrophilic IOL models. Moreover, the Nd:YAG capsulotomy rate was lower in the hydroimplantation group that used a hydrophilic IOL than it was in the viscoimplantation group, which used a hydrophobic IOL. In this technique, the irrigation fluid is forced between the IOL and the posterior capsule, which creates a jet flow and allows for the removal of LECs. Additionally, the rotational movement created within the bag to position contributes to the removal of LECs because these movements act directly on the surface of the posterior capsule without the involvement of viscoelastic.
Another advantage of the hydroimplantation technique is that it makes it easier for the IOL to adhere to the capsule (particularly the hydrophobic material) due to minimal remaining viscoelastic between the IOL and the posterior capsule. The adhesion between the IOL and the posterior capsule may reduce the possibility of PCO by preventing the migration of epithelial cells at the equator of the center of the capsule. However, it may not be possible to remove all viscoelastic material that remains behind the IOL, which could leave some LECs behind in patients where the viscoimplantation technique is used for cataract surgery.
The limitations of our study were that the patients' follow-up interval was less than three years, and the amount and grade of posterior capsule opacification could not be evaluated exactly.
In conclusion, this retrospective study revealed that the hydroimplantation technique may reduce Nd:YAG capsulotomy rates for hydrophilic IOLs, since there was no significant difference in PCO development in hydrophobic IOLs. Long-term prospective studies on this issue will strengthen the findings of this study.
Figures and Tables
 | Fig. 1The number of intraocular lens models and the neodymium-doped yttrium aluminum garnet (YAG) capsulotomy ratio of these two groups. |
References
1. Schriefl SM, Menapace R, Stifter E, et al. Posterior capsule opacification and neodymium:YAG laser capsulotomy rates with 2 microincision intraocular lenses: four-year results. J Cataract Refract Surg. 2015; 41:956–963.

2. Menapace R. After-cataract following intraocular lens implantation. Part I. Genesis and prevention by optimizing conventional lens implants and surgical techniques. Ophthalmologe. 2007; 104:253–262.
3. Apple DJ, Solomon KD, Tetz MR, et al. Posterior capsule opacification. Surv Ophthalmol. 1992; 37:73–116.

4. Apple DJ, Mamalis N, Brady SE, et al. Biocompatibility of implant materials: a review and scanning electron microscopic study. J Am Intraocul Implant Soc. 1984; 10:53–66.

5. Nishi O. Incidence of posterior capsule opacification in eyes with and without posterior chamber intraocular lenses. J Cataract Refract Surg. 1986; 12:519–522.

6. Tak H. Hydroimplantation: foldable intraocular lens implantation without an ophthalmic viscosurgical device. J Cataract Refract Surg. 2010; 36:377–379.

7. Hayashi K, Hayashi H, Nakao F, Hayashi F. Changes in posterior capsule opacification after poly (methyl methacrylate), silicone, and acrylic intraocular lens implantation. J Cataract Refract Surg. 2001; 27:817–824.
8. Ernest PH. Posterior capsule opacification and neodymium: YAG capsulotomy rates with AcrySof acrylic and PhacoFlex II silicone intraocular lenses. J Cataract Refract Surg. 2003; 29:1546–1550.

9. Buehl W, Sacu S, Findl O. Association between intensity of posterior capsule opacification and contrast sensitivity. Am J Ophthalmol. 2005; 140:927–930.

10. Montenegro GA, Marvan P, Dexl A, et al. Posterior capsule opacification assessment and factors that influence visual quality after posterior capsulotomy. Am J Ophthalmol. 2010; 150:248–253.

11. Davidson MG, Morgan DK, McGahan MC. Effect of surgical technique on in vitro posterior capsule opacification. J Cataract Refract Surg. 2000; 26:1550–1554.

12. Nishi O, Nishi K. Intracapsular cataract surgery with lens epithelial cell removal. Part III: Long-term follow-up of posterior capsular opacification. J Cataract Refract Surg. 1991; 17:218–220.
13. Mamalis N, Crandall AS, Linebarger E, et al. Effect of intraocular lens size on posterior capsule opacification after phacoemulsification. J Cataract Refract Surg. 1995; 21:99–102.

14. Vasavada AR, Raj SM, Johar K, Nanavaty MA. Effect of hydrodissection alone and hydrodissection combined with rotation on lens epithelial cells: surgical approach for the prevention of posterior capsule opacification. J Cataract Refract Surg. 2006; 32:145–150.
15. Peng Q, Apple DJ, Visessook N, et al. Surgical prevention of posterior capsule opacification. Part 2: Enhancement of cortical cleanup by focusing on hydrodissection. J Cataract Refract Surg. 2000; 26:188–197.
16. Tan DT, Chee SP. Early central posterior capsular fibrosis in sulcus-fixated biconvex intraocular lenses. J Cataract Refract Surg. 1993; 19:471–480.

17. Trivedi RH, Werner L, Apple DJ, et al. Post cataract-intraocular lens (IOL) surgery opacification. Eye (Lond). 2002; 16:217–241.

18. Menapace R, Wirtitsch M, Findl O, et al. Effect of anterior capsule polishing on posterior capsule opacification and neodymium:YAG capsulotomy rates: three-year randomized trial. J Cataract Refract Surg. 2005; 31:2067–2075.

19. Studeny P, Hyndrak M, Kacerovsky M, et al. Safety of hydroimplantation: a foldable intraocular lens implantation without the use of an ophthalmic viscosurgical device. Eur J Ophthalmol. 2014; 24:850–856.

20. Ogurel T, Ogurel R, Onaran Z, Ornek K. Safety of hydroimplantation in cataract surgery in patients with pseudoexfoliation syndrome. Int J Ophthalmol. 2017; 10:723–727.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download