Abstract
Purpose
To determine the frequency of ocular diseases in infants visiting the ophthalmology department of a tertiary care hospital.
Methods
This was a cross-sectional descriptive study conducted in the department of ophthalmology, Abbasi Shaheed Hospital, from January 2015 to May 2016. The study included 377 infants ranging in age from 1 day to less than 1 year who were, selected by a nonprobability consecutive sampling technique. A detailed history was taken, and a complete ocular examination was performed. Descriptive statistics were used to calculate the mean and standard deviation for age. Frequencies were calculated for ocular diseases along with the percentages. Outcome variables included various congenital and acquired diseases such as conjunctivitis, congenital cataract, glaucoma, nasolacrimal duct blockage, squint, trauma, and fundus abnormalities.
Results
The mean age of infants was 5.0 ± 3.7 months. There were 196 (52%) males and 181 (48%) females. The sample included 330 (87.5%) full term infants. Acquired ocular diseases occurred in 230 (61%) infants; and congenital diseases, in 147 (39%). The most common ocular disease was conjunctivitis, which occurred in 173 (46%) infants, followed by congenital blocked nasolacrimal duct, which occurred in 57 (15 %) infants. Conjunctivitis was more common among neonates than infants.
Globally, congenital anomalies are responsible for a considerable number of still births, infant deaths, and disabilities in young children [1]. It is estimated that congenital anomalies account for approximately 15% to 20% of cases of blindness and severe visual impairment in children worldwide [2].
Neonates should undergo an ocular examination soon after birth. This examination plays a positive role in promoting pediatric eye health among pediatricians and parents [3]. The American Academy of Pediatrics recommends red ref lex testing shortly after birth [4]. Formal testing of recognition of visual acuity typically begins around the age of three years. The failure to detect and appropriately manage disorders of vision in early childhood can have long-term consequences for visual development and affects the child's self-confidence and realization of potential [5]. Infants are unable to express their complaints, and parents and caretakers may be unaware of important facts about visual development. The first year of life is a crucial period when the visual system develops and binocular vision is formed. Amblyopia and permanent visual deficit can occur if a visual deficit at this age is not treated appropriately. Therefore, early diagnosis and prompt treatment are critically important [6].
Conjunctivitis is the most common ocular disease worldwide among neonates [7]. It remains a major problem in underdeveloped countries. Inadequate maternal care and the lack of widespread use of prophylactic treatment to prevent infections immediately after birth are major causative factors in third world countries [8]. Retinopathy of prematurity (ROP) is responsible for up to 15% of cases of blindness in developed countries and up to 60% of cases in middle income countries [9].
Several studies have examined ocular health of children in Pakistan, but none has specifically focused on infants [10111213]. Indeed, studies of infants less than 1 year old are lacking. The prevalence of ocular abnormalities, transient and permanent, is largely unknown. It is important to establish frequencies of various congenital and acquired ocular diseases in this part of the world. Our study assessed the frequencies of ocular diseases in infants in a tertiary care hospital to aid in the assessment and application of preventive strategies in Pakistan.
This prospective, cross-sectional descriptive study was conducted in the Department of Ophthalmology, Abbasi Shaheed Hospital, Karachi—a tertiary care hospital. The study began in January 2015 after approval from the ethical and scientific research committees of Karachi Medical and Dental College (approval no. 0034/14) and was completed by June 2016.
Using Raosoft, we calculated a sample size of 377 infants, with a 95% confidence interval and 5% margin of error [14]. All infants between 1 day and 1 year of age who were seen at an outpatient department of ophthalmology or who were referred from the pediatrics and obstetrics department were included by a nonprobability consecutive sampling technique. Babies previously diagnosed and seen for follow ups were not included in the study.
Written inform consent, along with permission for publication of the research details of the patient, were obtained from parents. A detailed history regarding the presenting complaint, birth history, and family history was taken. Examination of the infant included visual assessment by fixating on and following a flashing-light, external inspection of the lids, ocular adnexa, and anterior segment; pupil examination with a torch; and red reflex examination with a distant direct ophthalmoscope. The red reflex of the fundus was used to rule out congenital cataract, persistent hyperplastic primary vitreous, retinal detachment, and other causes of leukocoria. Indirect ophthalmoscopy was performed after pupil dilation where fundus examination was required. In most cases, diagnosis was based on clinical grounds. A few infants, for whom diagnosis could not be made by a simple torch examination, were examined under general anesthesia and managed accordingly. These children were followed up in an eye outpatient department for observation and medical and surgical management. Infants were referred to the Pediatrics Department for systemic evaluation when necessary. Data were collected and analyzed with the IBM SPSS Statistics ver. 21 (IBM Corp., Armonk, NY, USA). Descriptive statistics were used to calculate the mean and standard deviation of age. Frequencies were calculated for ocular diseases, along with percentages. Outcome variables included various congenital and acquired ocular diseases. Congenital diseases included congenital cataract, congenital glaucoma, congenital nasolacrimal duct blockage, primary optic atrophy, and squint. Acquired ocular diseases included conjunctivitis, cornel ulcer, trauma, stye, and other fundus abnormalities.
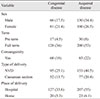
The mean age of infants was 5.0 ± 3.7 months, with a range of 1 day to 11.3 months. Among the 377 infants, 196 (52%) were males and 181 (48%) were females. Full-term infants were more common 330; (87.5%) than preterm infants. Consanguinity occurred in 151 (40%) infants, and mode of delivery was normal vaginal delivery in 248 (66%) infants (Table 1).
Acquired ocular diseases were present in 230 (61%) infants; and congenital diseases, in 147 (39%). The most common ocular disease was conjunctivitis, which occurred in 173 (46%) infants, followed by congenital blocked nasolacrimal duct, which occurred in 57 (15%) infants. Congenital glaucoma and retinopathy of prematurity occurred in 3 (0.8%) infants each (Table 2). Skin lesions were observed in 30 (8%) infants and included, preseptal cellulitis (4), stye (3), periorbital abscess (2), external angular dermoid cyst (2), capillary hemangioma (2), dermolipoma (2), port wine stain (2), upper lid coloboma (2), herpes simplex blepharitis (2), and others (Table 3). Miscellaneous diseases occurred in 44 (11.7%) infants and included diseases such as iris coloboma (3), heterochromia iridis (3), microphthalmia (3), aniridia (2), albinism (2), conjunctival nevus (2), and rare diseases such as Peter's anomaly (1), Axenfeld Riegers anomaly (1), megalocornea (1), sclerocornea (1) and others (Table 4).
The most common ocular surface disease, especially in children, is conjunctivitis [15]. In the United States alone, more than 6 million patients are diagnosed with acute conjunctivitis each year. The cost of treating bacterial conjunctivitis alone is estimated at 380 million to 860 million US dollars per year [16]. A previous study documented a prevalence of conjunctivitis of 17% among nearly 1,000 newborn babies in Pakistan [9]. However, these statistics have not previously been documented in babies or infants of less than 1 year of age. In the current study, the most common acquired disease was conjunctivitis (46%) in both infants and neonates. The results are similar to those of previous studies, which have reported conjunctivitis as 26.8% [13], 41.3% [11], and 42.5% [12] of the study sample [13]. However, these studies included children up to 12 years of age and did not specifically mention infants or neonates. Fortunately, conjunctivitis is self-limiting and generally resolves within a few days. However, earlier resolution of symptoms, avoidance of complications, and reduction in the risk of contagion can be achieved by a short course of topical antibiotics [17].
We found congenital ocular diseases in 39% of patients and acquired ocular diseases in 61%. Congenital problems may present at birth, or they may be developmental. They are usually secondary to genetic conditions or due to the intrauterine effect of drugs, alcohol, or maternal blood sugar [18]. The parents were in consanguineous marriages in 40% of cases in our study, which might have led to congenital disorders. Consanguineous marriages increase the likelihood of autosomal recessive diseases, like anophthalmos, microphthalmos, coloboma and Aniridia [19]. In our study, the most common congenital disease and the second most common ocular disease in infants was congenital nasolacrimal duct obstruction, which occurred in 15% of cases. The prevalence of congenital nasolacrimal duct obstruction was 12.9% in a Nigerian study [12] and 25.8% [11] and 4.05% [13] in other studies. These results vary across studies because most have included older children, whereas congenital nasolacrimal duct block presents in the first year of life.
Leukocoria is an abnormal white pupillary light reflex and is the predominant symptom of congenital cataracts, vitreoretinal disorders, retinopathy of prematurity, trauma associated diseases, ocular toxocariasis, Norrie disease, Coats' disease, and retinal hamartomas [20]. Congenital cataract remains the most common treatable cause of visual disability in infancy and childhood [21]. Parents and family members generally detect leukocoria and help in initiating diagnosis [20]. The birth prevalence of cataract ranges from 3 of 1,000 live births to 5 of 1,000 live births [22]. It occurred in 5% of cases in our study, compared to 19% [23], 2.18% [24], and 5.68% [13] in other studies. These previous studies included children of varying age groups, including neonates, infants and children up to 16 years, but none specifically focused on babies of less than 1 year.
In our study, ocular trauma occurred in 2.7% of infants, compared to 8.45% [24] and 6.8% [13] in other studies. Trauma or injury is more common in school going children than infants. We found that congenital glaucoma and ROP each occurred in about 0.8% of patients. ROP is responsible for up to 15% of all cases of blindness in industrialized countries and up to 60% in middle income countries [9]. Its incidence has been reported at 32.5% of premature infants in a local study [25], which was conducted in a private sector teaching hospital, well equipped with the latest technology. In Pakistan, for the last 6 years, more than 60% of deaths under 5 years have occurred during the neonatal period (55 of 1,000 live births) [26]. Not only is the survival rate poor in our country, but the screening programs for preterm infants with ROP are deficient. Our study included only 47 (12.5%) preterm babies, whereas ROP is specifically diagnosed in preterm and low birth weight babies, which may explain why we found a lower prevalence of ROP than other studies. Appropriate screening protocols ensure early detection in the first weeks of life so that treatment (peripheral ablation of avascular retina) with a laser or cryotherapy can be provided [27].
Severe visual impairment occurred in 17 (4.5%) infants and included both treatable and untreatable diseases. Mature cataract, optic atrophy, advanced glaucoma, anophthalmos, retinal detachment, ROP, optic atrophy, keratomalacia with perforation, corneal opacities, and myopia were observed. Childhood visual impairment is a serious global issue, predominantly in developing countries. Illiteracy, poor socioeconomic conditions, and lack of basic health facilities all contribute to the already large issue of visual impairment in children of third world countries. All of these factors can lead to irreversible blindness despite preventable conditions in many cases [28].
In children, ocular diseases vary from place to place. Climatic conditions, malnourishment, and lack of treatment services play an essential role in the pattern of occurrence of ocular diseases [24]. However, greater emphasis should be placed on improving eye health, recognizing and treating common eye diseases, and preventing development of blindness among infants, in collaboration with a primary health care worker, ophthalmologist, and pediatrician. These children will be carrying the burden of our country on their shoulders in the future.
This study had some limitations. For example, the sample size was relatively small, and it was a single center study. Increasing the sample size and collecting data from other hospitals at different localities would provide valuable information on infant ocular morbidity. Also, in the future, babies of less than 7 days of life should be screened for ocular infections.
In conclusion, acquired ocular diseases were more common than congenital ocular diseases in a sample of infants from Pakistan. The most common ocular pathology was conjunctivitis, followed by congenital nasolacrimal duct obstruction. Conjunctivitis was more common in neonates than infants of less than 1 year of age.
Figures and Tables
 | Fig. 1Ocular diseases in neonates and infants. NLD = nasolacrimal duct; ROP = retinopathy of prematurity; RD = retinal detachment. |
References
1. Petrini J, Damus K, Russell R, et al. Contribution of birth defects to infant mortality in the United States. Teratology. 2002; 66:S3–S6.

2. Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: the right to sight. Bull World Health Organ. 2001; 79:227–232.
3. Li LH, Li N, Zhao JY, et al. Findings of perinatal ocular examination performed on 3573, healthy full-term newborns. Br J Ophthalmol. 2013; 97:588–591.

4. American Academy of Pediatrics. Section on Ophthalmology. American Association for Pediatric Ophthalmology and Strabismus. . Red reflex examination in neonates, infants, and children. Pediatrics. 2008; 122:1401–1404.
5. Davidson S, Quinn GE. The impact of pediatric vision disorders in adulthood. Pediatrics. 2011; 127:334–339.

6. Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999; 83:387–388.

7. Kakar S, Bhalla P, Maria A, et al. Chlamydia trachomatis causing neonatal conjunctivitis in a tertiary care center. Indian J Med Microbiol. 2010; 28:45–47.

8. De Schryver A, Meheus A. Epidemiology of sexually transmitted diseases: the global picture. Bull World Health Organ. 1990; 68:639–654.
9. Gilbert C, Fielder A, Gordillo L, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005; 115:e518–e525.

10. Gul SS, Jamal M, Khan N. Ophthalmia neonatorum. J Coll Physicians Surg Pak. 2010; 20:595–598.
11. Fatima K, Shahid E, Shaikh A. Frequency of common eye diseases in pediatric outpatient department of a tertiary care hospital. Pak J Ophthalmol. 2015; 31:154–157.
12. Sethi S, Sethi MJ, Saeed N, Kundi NK. Pattern of common eye diseases in children attending outpatient eye department Khyber Teaching Hospital. Pak J Ophthalmol. 2008; 24:166–170.
13. Fasih U, Rahman A, Shaikh A, et al. Pattern of common paediatric diseases at Spencer Eye Hospital. Pak J Ophthalmol. 2014; 30:10–14.
14. Raosoft. Sample size calculator [Internet]. [place unknown]: Raosoft;2014. cited 2014 Dec 17. Available from: http://www.raosoft.com/samplesize.html.
15. Bremond-Gignac D, Mariani-Kurkdjian P, Beresniak A, et al. Efficacy and safety of azithromycin 1.5% eye drops for purulent bacterial conjunctivitis in pediatric patients. Pediatr Infect Dis J. 2010; 29:222–226.

16. Smith AF, Waycaster C. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmol. 2009; 9:13.

17. Rose PW, Ziebland S, Harnden A, et al. Why do general practitioners prescribe antibiotics for acute infective conjunctivitis in children? Qualitative interviews with GPs and a questionnaire survey of parents and teachers. Fam Pract. 2006; 23:226–232.

18. Gogate P, Gilbert C, Zin A. Severe visual impairment and blindness in infants: causes and opportunities for control. Middle East Afr J Ophthalmol. 2011; 18:109–114.

19. Garg P, Qayum S, Dhingra P, Sidhu HK. Congenital ocular deformities-leading cause of childhood blindness: a clinical profile study. Indian J Clin Exp Ophthalmol. 2016; 2:21–26.
20. Balmer A, Munier F. Leukokoria in a child: emergency and challenge. Klin Monbl Augenheilkd. 1999; 214:332–335.
22. Rahi JS, Dezateux C. British Congenital Cataract Interest Group. Measuring and interpreting the incidence of congenital ocular anomalies: lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci. 2001; 42:1444–1448.
23. Adegbehingbe BO, Ajite KO, Adegbehingbe OO. Incidence of ocular congenital anomalies in a Nigerian Teaching Hospital. Orient J Med. 2005; 17:31–36.

24. Mehta S, Singh M, Chawla A, Agarwal A. Pattern of ocular diseases in children attending outpatient department of a rural medical college in Central India. Int J Sci Study. 2015; 3:57–60.
25. Taqui AM, Syed R, Chaudhry TA, et al. Retinopathy of prematurity: frequency and risk factors in a tertiary care hospital in Karachi, Pakistan. J Pak Med Assoc. 2008; 58:186–190.
26. National Institute of Population Studies. ICF International. Pakistan demographic and health survey 2012-13. Islamabad: National Institute of Population Studies;2013. p. 18–19.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download