INTRODUCTION
Pregnancy has been considered as a contraindication in pulmonary arterial hypertension (PAH) patients because of the high morbidity and mortality rates of both mother and fetus.
1)2)3) Even though doctors do not recommend pregnancy and provide repeated warnings and education on avoiding pregnancy in PAH women, there are always some cases of pregnancy maintained by chance or intentionally. Therefore, a doctor's recommendation has limitations in real world communication, and clinicians should be aware of pregnancy in PAH and how to help patients to achieve a better outcome.
Although the data on the pregnancies of PAH patients are limited, clinical management has been attempted to save the patients and their fetuses.
4) During the past decades, the treatment of PAH has been rapidly developed with the introduction of targeted therapy for PAH and advances in intensive fetal care, and clinical experiences about maternal care in patients with PAH have been shared.
5)6) Also, multidisciplinary team approach treatment with obstetricians, cardiologist, anesthesiologists, and neonatologists for pregnancy in PAH patients provided improvements to the morbidity and mortality of the patients.
5) As a result, the survival of PAH patients has been improved compared with the previous era.
3)
We report on a single center's successful experience in 10 cases of pregnant patients with PAH and discuss their comprehensive management.
Methods
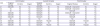
The study was conducted as a pulmonary hypertension registry in a single center (Samsung Medical Center, Seoul, Korea) from 2011 to 2017. All pregnant women with diagnoses of PAH who decided to maintain their pregnancies after comprehensive familial consultations with physicians were included.
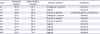
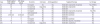
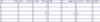
Clinical data were collected as follows: age, cause of PAH, underlying cardiovascular disease, and New York Heart Association (NYHA) functional classification at first visit. Laboratory tests included hemoglobin, hematocrit, creatinine, and N-terminal pro brain natriuretic peptide (NT-proBNP). The 6-minute walk test (6MWT) distance (m) and oximetry were also collected. Echocardiographic data were collected, including tricuspid annular plane systolic excursion (TAPSE), presence of pericardial effusion, right ventricular systolic pressure (RVSP) by Doppler tracing of tricuspid regurgitation, and mean pulmonary arterial pressure (PAP) by Mahan's equation. Obstetric data included gravidity and parity, gestational age at first visit and delivery, delivery methods, anesthesia during delivery, preterm labor, and any obstetrical complications. Fetal events, birth weight, and Apgar score were recorded. Medication during pregnancy and the peripartum period were described. Lengths of hospital stay and time in the intensive care unit (ICU) were also recorded. Pregnancy and peripartum complications were classified into cardiac and non-cardiac events. Cardiac events were defined as an aggravation of heart failure that required additional medication or admission, uncontrolled arrhythmia, and cardiac arrest. Non-cardiac events were defined as venous thromboembolism, major bleeding, and infection. Each patient gave informed consent to participate and the research was approved by the Institutional Review Board at Samsung medical center (IRB No. 2018-08-123).
Statistics
Baseline characteristics, obstetric data, and maternal and fetal outcomes were described as numbers and percentages for all PAH patients. Continuous variables were presented as medians and interquartile ranges. All statistical analyses were performed using SPSS Statistics 23.0 (SPSS, Chicago, IL, USA).
Discussion
In this retrospective study from a single center registry, 9 pregnant women with PAH were included. Because PAH is a rare disease, this is a relatively large study of pregnancy in patients with PAH. Although 10 cases of pregnancy have been reviewed, our study included a broad spectrum of PAH patients in terms of the PAH cause and severity. Moreover, reporting on successful pregnancy outcomes in PAH patients in the current era of PAH-specific therapies has important significance.
Previous systematic reviews showed that pregnancy in women with pulmonary hypertension is associated with a high maternal mortality, estimated at between 30% and 56%.
7) After the induction of the target therapy, maternal mortality for parturients with PAH has decreased over the past decades as compared with the previous era. Bedard et al. reported a systematic review of all cases of parturients with PAH published in a past decade (1997–2007), in which mortality decreased to 17–33% according to cause or type of PAH.
8) Moreover, data from the Registry of Pregnancy and Cardiac Disease of the European Society of Cardiology was published in 2016. This cohort study included 151 women with pulmonary hypertension. Of these women, 39 (26%) had PAH, categorized into 3 subgroups: IPAH, PAH associated with CHD, or PAH associated with other diseases. No patients died during pregnancy, only 5 women (3.3%) died peripartum up to 1 week after delivery, and 2 additional deaths (2.6%) occurred within 6 months after delivery. Death occurred most frequently in the IPAH group.
6) Because there were 7 patients in the IPAH group, and 3 deaths occurred in that group, the maternal mortality of IPAH was approximately 35%. Only 9 of 39 patients were treated with targeted therapy for PAH. It is not clear that maternal death occurred among those patients who were treated with targeted therapy. In our study population, all of the patients were group 1 PAH, and all of the patients were treated with PAH-specific drugs (8 of them before their peripartum periods and one of them immediately after delivery and in the postpartum period). The better outcomes of our patients were possibly related with targeted therapy.
The high maternal and fetal mortality in PAH patients is related to changes in cardiovascular physiology during pregnancy. The most remarkable hemodynamic change is expanded plasma volume.
5) The plasma volume progressively increases starting at the early phase of pregnancy (6–8 weeks).
9) Until the third trimester of pregnancy, blood volume increases to reach a maximum level of 50–70% above the patient's pre-pregnancy level.
10)11)12) In addition, cardiac output (CO) increases in the first trimester and then gradually rises to peak values of 30–50% above the pre-pregnancy level.
13) Multifactorial effects including expanded plasma volume, decreased afterload, eccentric hypertrophy, increased contractility, and heart rate are related to rising CO during pregnancy.
2)14)15) To compensate for this blood flow requirement, pregnancy-related hormonal changes cause vasodilation. As a result, systemic vascular resistance and pulmonary vascular resistance (PVR) are decreased.
1)2) Generally, the increase in plasma volume and CO and the decrease in PVR result in a grossly unchanged mean PAP. However, in the pregnant patients with PAH, these compensatory mechanisms have already been destroyed, resulting in a significant afterload stress on the right ventricle.
5) Therefore, for women with PAH, the causes of poor maternal outcomes are variable, from worsening PAH and right heart failure to cardiogenic shock.
2)16) Furthermore, the risk of these cardiac events is particularly high not only during the third trimester of pregnancy, but also in the delivery and postpartum period. During labor, additional blood volume is diverted from the uterus to the maternal circulation at each contraction, while blood loss due to hemorrhage and vasovagal response may lower the venous return.
16) These opposing physiological changes cause significant, acute increases in CO (15–80%).
17) In addition, anesthesia, infection, and thromboembolism in the postpartum period may put considerable stress on the maternal cardiovascular system. Therefore, postpartum care should be carefully performed under a multidisciplinary approach, and it would be better to share the patient's information before delivery. In our center, the cardiologist and obstetrician had a discussion immediately after each patient's decision to maintain the pregnancy, and this was shared with the anesthesiologist after 20 weeks of gestational age.
Current guidelines have declared that PAH patients should be counselled against pregnancy and therapeutic abortion should be recommended.
3) However, pregnancy in the real world cannot be completely avoided, because patients do not always follow medical guidelines. As for inevitable case of continuing pregnancy, the medical team should do their best to reduce the morbidity and mortality. It would better than to leave the patients from clinics and returns at almost full term. The clinical outcomes of our center are remarkable results in consideration of previously reported studies in which the mortality rate of pregnant patients with PAH reached 28–56%.
7)18)
The improvement of the clinical outcomes of our patients with PAH may be explained in several ways. First, 9 pregnancies received advanced pulmonary hypertension medication. A phosphodiesterase type 5 inhibitor (sildenafil) was given in all patients. Moreover, 3 of these 9 pregnant patients were administered a prostacyclin analogue (treprostinil). All of the patients were treated with dual therapy during the postpartum period. Second, a multidisciplinary team approach was applied during the peripartum period. Before delivery, the cardiologist, anesthesiologists, and obstetricians discussed the appropriate surgical procedure and anesthetic methods. In the case of high-risk pregnancy, invasive hemodynamic monitoring was performed. Defibrillator and percutaneous cardiopulmonary support were prepared for hemodynamic instability during operation. Third, the ICU was aggressively used for the management of high-risk pregnant patients with PAH. High risk patients were admitted to hospital in the third trimester for monitoring until postpartum and were sent to the critical care unit immediately after delivery for postpartum care.
However, there are several limitations in this study. First, this study was conducted in a single center, so the number of pregnant patients with PAH was relatively small. Second it is also notable that our patients were mostly NYHA functional class II, and had NT-proBNP levels less than 1,400. Low to intermediate risk patients, according to European Society of Cardiology guidelines, were the majority of this study. Pregnancy in more severely symptomatic PAH patients could have led to completely different consequences.
Although it is remarkable that no mortality occurred in the mothers or fetuses, more than half of patients were underwent cardiac events. Severe cardiac complications including cardiac arrest and recurrent VT also occurred in 2 cases of patients with Eisenmenger syndrome. Also, prematurity and low birth weight still remained significant neonatal complications. Therefore, pregnancy of patients with PAH should still not be allowed because of the high risk to mother and fetus. However, there is a possibility to improve the prognosis when applying maximal PAH targeted treatment in advance, multidisciplinary team management, and intensive care during the peripartum period in case of unavoidable pregnancy. Also, this management should be performed in the PAH specialized expert center.
In conclusion, the outcomes of pregnant patients with PAH have a possibility to be improved with PAH targeted therapy when compared to the previous era of hopelessness without treatment methods. However, it is remained unchanged that the women with PAH should be advice against pregnancy and therapeutic abortion should be recommended. The best medical support should be provided on an individual basis, only if a patient is determined to maintain her pregnancy in spite of medical advice. Multidisciplinary team approach management and intensive care were strongly recommended in case of inevitable pregnancy. Further experiences should be shared to improve the survival of mother and fetus.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download