INTRODUCTION
METHODS
Study population
Percutaneous coronary intervention procedure and proximal optimization technique
Data collection and quantitative coronary angiographic analysis
Definitions and outcomes
Statistical analysis
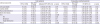
Table 1
Baseline patient characteristics

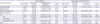
Table 2
Angiographic and procedural characteristics

Table 3
Quantitative coronary angiographic analysis

RESULTS
Clinical, angiographic, and procedural characteristics
Quantitative coronary angiographic data
Clinical outcomes
Table 4
Clinical outcomes in POT group compared with non-POT group during follow-up period
 | Figure 1Cumulative incidence functions in POT versus non-POT groups from a competing risk proportional hazard model for MACE. (A) Cumulative incidence functions for MACEs in POT (solid line) versus non-POT groups (dashed line) in all patients. (B) Cumulative incidence functions for MACEs in POT versus non-POT groups in propensity-matched populations.MACE = major adverse cardiac event; POT = proximal optimization technique; PS = propensity-score.
|
Subgroup analysis
 | Figure 2Comparative unadjusted HRs of MACE for subgroups in all population. The association of POT with better TLR outcomes was consistent across various subgroups without a significant interaction.HR = hazard ratio; FKB = final kissing ballooning; MACE = major adverse cardiac event; POT = proximal optimization technique; TLR = target lesion revascularization.
|
 | Figure 3Comparative unadjusted HRs of TLR for subgroups in all population. There was a significant interaction between the use of POT and TLR according to the presence or absence of final kissing ballooning.HR = hazard ratio; FKB = final kissing ballooning; POT = proximal optimization technique; TLR = target lesion revascularization.
|
The impact of POT in patients treated without kissing ballooning
Table 5
Clinical outcomes in patients without kissing ballooning during follow-up period




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download