1. Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res. 1988; (230):83–97.

2. Anglen JO, Burd TA, Hendricks KJ, Harrison P. The “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. 2003; 17:625–634. PMID:
14574190.
3. Bhandari M, Matta J, Ferguson T, Matthys G. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br. 2006; 88:1618–1624. PMID:
17159175.

4. Kreder HJ, Rozen N, Borkhoff CM, et al. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006; 88:776–782. PMID:
16720773.

5. Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999; 7:128–141. PMID:
10217820.

6. Guerado E, Cano JR, Cruz E. Fractures of the acetabulum in elderly patients: an update. Injury. 2012; 43(Suppl 2):S33–S41. PMID:
23622990.

7. Sierra RJ, Mabry TM, Sems SA, Berry DJ. Acetabular fractures: the role of total hip replacement. Bone Joint J. 2013; 95-B(11 Suppl A):11–16. PMID:
24187344.
8. De Bellis UG, Legnani C, Calori GM. Acute total hip replacement for acetabular fractures: a systematic review of the literature. Injury. 2014; 45:356–361. PMID:
24112700.

9. Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Joint Surg Am. 2002; 84:1–9.
10. Malhotra R, Singh DP, Jain V, Kumar V, Singh R. Acute total hip arthroplasty in acetabular fractures in the elderly using the Octopus System: mid term to long term follow-up. J Arthroplasty. 2013; 28:1005–1009. PMID:
23523497.
11. Saterbak AM, Marsh JL, Turbett T, Brandser E. Acetabular fractures classification of Letournel and Judet--a systematic approach. Iowa Orthop J. 1995; 15:184–196. PMID:
7634031.
12. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755. PMID:
5783851.
13. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973; 55:1629–1632. PMID:
4217797.
14. Grubor P, Krupic F, Biscevic M, Grubor M. Controversies in treatment of acetabular fracture. Med Arch. 2015; 69:16–20. PMID:
25870470.

15. Zha GC, Sun JY, Dong SJ. Predictors of clinical outcomes after surgical treatment of displaced acetabular fractures in the elderly. J Orthop Res. 2013; 31:588–595. PMID:
23192663.

16. Moed BR, WillsonCarr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002; 84:752–758. PMID:
12004016.

17. Carpintero P, Caeiro JR, Carpintero R, Morales A, Silva S, Mesa M. Complications of hip fractures: a review. World J Orthop. 2014; 5:402–411. PMID:
25232517.

18. O'Toole RV, Hui E, Chandra A, Nascone JW. How often does open reduction and internal fixation of geriatric acetabular fractures lead to hip arthroplasty? J Orthop Trauma. 2014; 28:148–153. PMID:
23719343.
19. Berry DJ. Antiprotrusio cages for acetabular revision. Clin Orthop Relat Res. 2004; (420):106–112.

20. Carroll FA, Hoad-Reddick DA, Kerry RM, Stockley I. The survival of support rings in complex acetabular revision surgery. J Bone Joint Surg Br. 2008; 90:574–578. PMID:
18450621.

21. Hipfl C, Janz V, Löchel J, Perka C, Wassilew GI. Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Joint J. 2018; 100-B:1442–1448. PMID:
30418066.
22. Hanssen AD, Lewallen DG. Modular acetabular augments: composite void fillers. Orthopedics. 2005; 28:971–972. PMID:
16190073.

23. Ballester Alfaro JJ, Sueiro Fernández J. Trabecular Metal buttress augment and the Trabecular Metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. Hip Int. 2010; 20(Suppl 7):S119–S127. PMID:
20512783.

24. Kellet CF, Gross AE, Backstein D, Safir O. Massive acetabular bone loss: the cup-cage solution. Semin Arthroplast. 2010; 21:57–61.
25. Kosashvili Y, Backstein D, Safir O, Lakstein D, Gross AE. Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br. 2009; 91:870–876. PMID:
19567849.

26. Abolghasemian M, Tangsaraporn S, Drexler M, et al. The challenge of pelvic discontinuity: cup-cage reconstruction does better than conventional cages in mid-term. Bone Joint J. 2014; 96-B:195–200. PMID:
24493184.
27. Amenabar T, Rahman WA, Hetaimish BM, Kuzyk PR, Safir OA, Gross AE. Promising mid-term results with a cup-cage construct for large acetabular defects and pelvic discontinuity. Clin Orthop Relat Res. 2016; 474:408–414. PMID:
25712864.

28. Paprosky WG, O'Rourke M, Sporer SM. The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res. 2005; 441:216–220. PMID:
16331006.

29. Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006; 21(6 Suppl 2):87–90. PMID:
16950068.

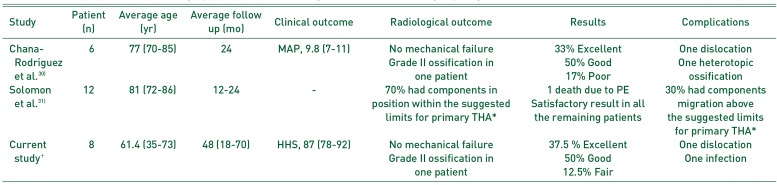
30. Chana-Rodríguez F, Villanueva-Martínez M, Rojo-Manaute J, Sanz-Ruíz P, Vaquero-Martín J. Cup-cage construct for acute fractures of the acetabulum, re-defining indications. Injury. 2012; 43(Suppl 2):S28–S32. PMID:
23622988.

31. Solomon LB, Studer P, Abrahams JM, et al. Does cup-cage reconstruction with oversized cups provide initial stability in THA for osteoporotic acetabular fractures? Clin Orthop Relat Res. 2015; 473:3811–3819. PMID:
26194560.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download