1. Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord. 2015; 16:229. PMID:
26316274.

2. Støen RØ, Lofthus CM, Nordsletten L, Madsen JE, Frihagen F. Randomized trial of hemiarthroplasty versus internal fixation for femoral neck fractures: no differences at 6 years. Clin Orthop Relat Res. 2014; 472:360–367. PMID:
23975250.

3. Chammout GK, Mukka SS, Carlsson T, Neander GF, Stark AW, Skoldenberg OG. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: a randomized long-term follow-up study. J Bone Joint Surg Am. 2012; 94:1921–1928. PMID:
23014835.
4. Leonardsson O, Kärrholm J, Åkesson K, Garellick G, Rogmark C. Higher risk of reoperation for bipolar and uncemented hemiarthroplasty. Acta Orthop. 2012; 83:459–466. PMID:
22998529.

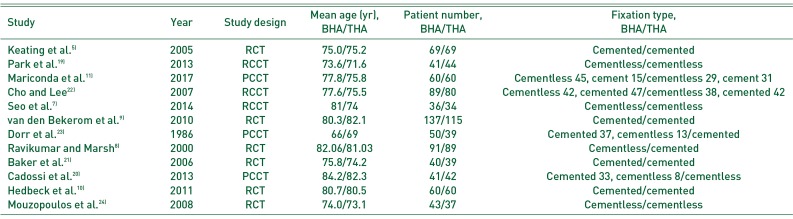
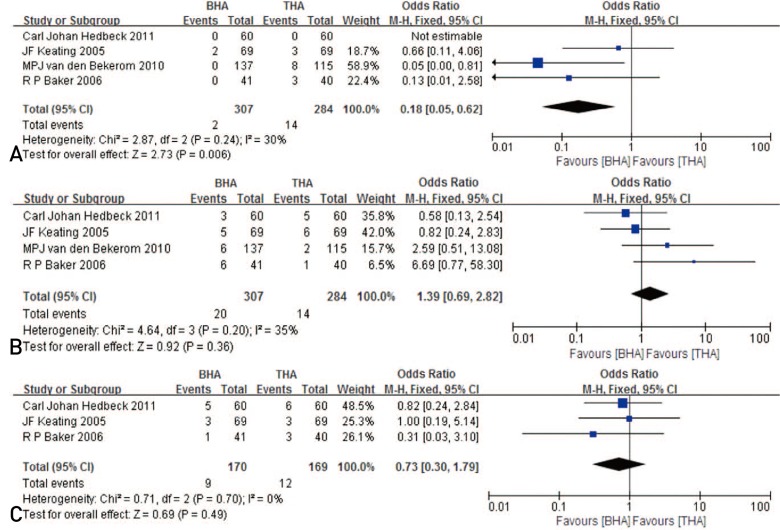
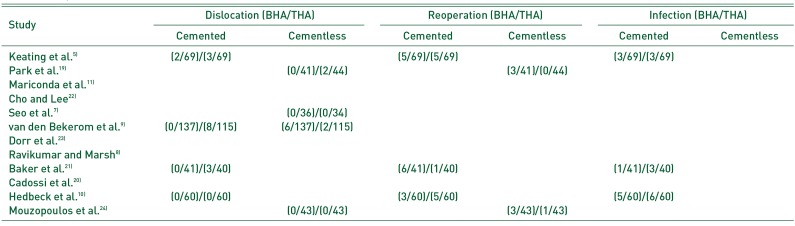
5. Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess. 2005; 9:iii–iv. ix–x. 1–65.

6. Avery PP, Baker RP, Walton MJ, et al. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: a seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011; 93:1045–1048. PMID:
21768626.
7. Seo JS, Shin SK, Jun SH, Cho CH, Lim BH. The early result of cementless arthroplasty for femur neck fracture in elderly patients with severe osteoporosis. Hip Pelvis. 2014; 26:256–262. PMID:
27536590.

8. Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur--13 year results of a prospective randomised study. Injury. 2000; 31:793–797. PMID:
11154750.
9. van den Bekerom MP, Hilverdink EF, Sierevelt IN, et al. A comparison of hemiarthroplasty with total hip replacement for displaced intracapsular fracture of the femoral neck: a randomised controlled multicentre trial in patients aged 70 years and over. J Bone Joint Surg Br. 2010; 92:1422–1428. PMID:
20884982.
10. Hedbeck CJ, Enocson A, Lapidus G, et al. Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011; 93:445–450. PMID:
21368076.
11. Mariconda M, Costa G, Misasi M, Recano P, Balato G, Rizzo M. Ambulatory ability and personal independence after hemiarthroplasty and total arthroplasty for intracapsular hip fracture: a prospective comparative study. J Arthroplasty. 2017; 32:447–452. PMID:
27546471.

12. Tice A, Kim P, Dinh L, Ryu JJ, Beaulé PE. A randomised controlled trial of cemented and cementless femoral components for metal-on-metal hip resurfacing: a bone mineral density study. Bone Joint J. 2015; 97-B:1608–1614. PMID:
26637673.
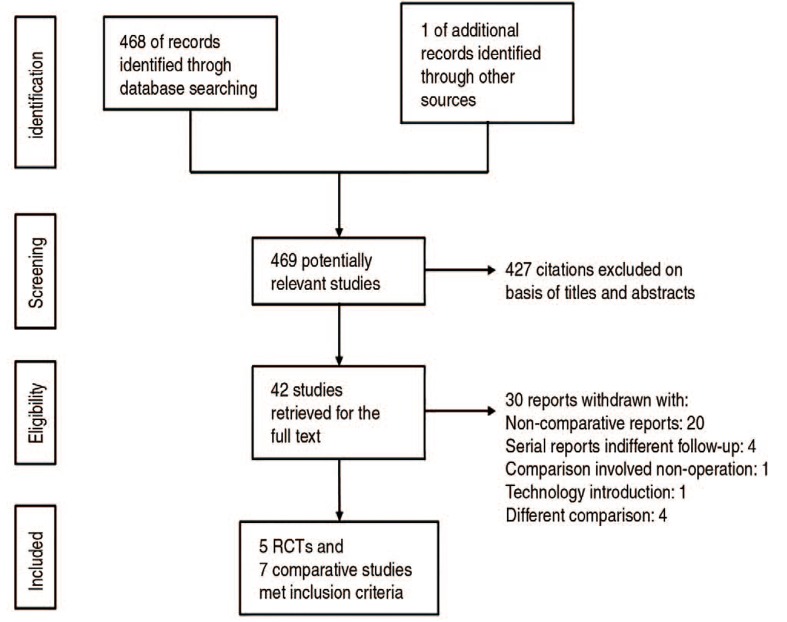
13. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009; 62:e1–e34. PMID:
19631507.

14. Sendtner E, Renkawitz T, Kramny P, Wenzl M, Grifka J. Fractured neck of femur--internal fixation versus arthroplasty. Dtsch Arztebl Int. 2010; 107:401–407. PMID:
20589205.
15. Beaudet K. The cochrane collaboration and meta-analysis of clinical data. Am Orthopt J. 2010; 60:6–8. PMID:
21061877.

16. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13. PMID:
15840177.

17. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25:603–605. PMID:
20652370.

18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID:
12958120.

19. Park KS, Oh CS, Yoon TR. Comparison of minimally invasive total hip arthroplasty versus conventional hemiarthroplasty for displaced femoral neck fractures in active elderly patients. Chonnam Med J. 2013; 49:81–86. PMID:
24010071.

20. Cadossi M, Chiarello E, Savarino L, et al. A comparison of hemiarthroplasty with a novel polycarbonate-urethane acetabular component for displaced intracapsular fractures of the femoral neck: a randomised controlled trial in elderly patients. Bone Joint J. 2013; 95-B:609–615. PMID:
23632669.
21. Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006; 88:2583–2589. PMID:
17142407.
22. Cho MR, Lee HS. Early results after the treatment with total hip arthroplasty with larger diameter femoral head versus bipolar arthroplasty in patients with femoral neck fractures. J Korean Hip Soc. 2007; 19:463–467.

23. Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986; 1:21–28. PMID:
3559574.

24. Mouzopoulos G, Stamatakos M, Arabatzi H, et al. The four-year functional result after a displaced subcapital hip fracture treated with three different surgical options. Int Orthop. 2008; 32:367–373. PMID:
17431621.

25. Vidović D, Punda M, Darabošs N, Bekavac-Bešslin M, Bakota B, Matejčcić A. Regional bone loss following femoral neck fracture: a comparison between cemented and cementless hemiarthroplasty. Injury. 2015; 46(Suppl 6):S52–S56.

26. Langslet E, Frihagen F, Opland V, Madsen JE, Nordsletten L, Figved W. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014; 472:1291–1299. PMID:
24081667.

27. Bezwada HP, Shah AR, Harding SH, Baker J, Johanson NA, Mont MA. Cementless bipolar hemiarthroplasty for displaced femoral neck fractures in the elderly. J Arthroplasty. 2004; 19(7 Suppl 2):73–77.

28. Vidovic D, Matejcic A, Punda M, et al. Periprosthetic bone loss following hemiarthroplasty: a comparison between cemented and cementless hip prosthesis. Injury. 2013; 44(Suppl 3):S62–S66. PMID:
24060022.

29. Weingarten S, Riedinger M, Conner L, et al. Hip replacement and hip hemiarthroplasty surgery: potential opportunities to shorten lengths of hospital stay. Am J Med. 1994; 97:208–213. PMID:
8092168.

30. Sierra RJ, Timperley JA, Gie GA. Contemporary cementing technique and mortality during and after Exeter total hip arthroplasty. J Arthroplasty. 2009; 24:325–332. PMID:
18534404.

31. Gavaskar AS, Tummala NC, Subramanian M. Cemented or cementless THA in patients over 80 years with fracture neck of femur: a prospective comparative trial. Musculoskelet Surg. 2014; 98:205–208. PMID:
23912215.
32. Burgers PT, Van Geene AR, Van den Bekerom MP, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop. 2012; 36:1549–1560. PMID:
22623062.

33. Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ. 2010; 340:c2332. PMID:
20543010.

34. Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010; (6):CD001706. PMID:
20556753.

35. Assi C, El-Najjar E, Samaha C, Yammine K. Outcomes of dual mobility cups in a young Middle Eastern population and its influence on life style. Int Orthop. 2017; 41:619–624. PMID:
28074257.

36. Kim YT, Yoo JH, Kim MK, Kim S, Hwang J. Dual mobility hip arthroplasty provides better outcomes compared to hemiarthroplasty for displaced femoral neck fractures: a retrospective comparative clinical study. Int Orthop. 2018; 42:1241–1246. PMID:
29344700.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download