Abstract
Purpose
Thyroid reoperations are surgically challenging because of significant anatomical variance. Visual and functional identification of the external branch of the superior laryngeal nerve (EBSLN) were studied in 2 groups of patients who underwent primary and redo thyroid surgery.
Methods
This study was conducted on 200 patients: 100 patients with redo and 100 patients with primary thyroid surgery. In addition to visual identification, nerve branches were functionally identified by intraoperative nerve monitoring (IONM). Visual, functional, and total identification rates of the EBSLN in both primary and redo surgery were determined and compared between the 2 groups.
Results
We attempted to identify 138 and 170 EBSLNs at risk in redo and primary surgery, respectively. Visual identification rates were 65.3% and 30.4% (P < 0.001) in primary and redo surgery groups, respectively. In total, 164 (96.5%) and 97 EBSLNs (70.3%) were identified in primary and redo surgery, respectively (P < 0.001), including the use of IONM. In primary surgery group, 53 nonvisualized EBSLNs of 164 identified nerves (32.3%) were determined by IONM alone. In redo surgery group, 55 of 97 identified nerves (56.7%) were determined by IONM alone (P < 0.001).
Conclusion
Both visual and total identification rates of the EBSLN are significantly decreased in reoperative thyroidectomy. IONM increases the total identification rate of the EBSLN in primary and redo thyroid surgery. Electrophysiological monitoring makes a substantial contribution to the identification of the EBSLN both in primary and especially in redo thyroid surgery.
Anatomical and electrophysiological identification of the external branch of the superior laryngeal nerve (EBSLN) is an important step during thyroidectomy. Visual identification and anatomical exposure of the EBSLN and its functional identification rate by intraoperative nerve monitoring (IONM) have been studied in primary thyroid surgery [12345]. However, we could not find any publication in the English literature on visual and electrophysiological identification of the EBSLN during redo thyroid surgery. Thyroid reoperations are surgically challenging because of scarring, significant distortion, and anatomical changes in the thyroid bed [6].
The EBSLN innervates the cricothyroid muscle (CTM) which is important in adjusting the tension and length of the vocal cords, which provide voice quality [78]. CTM electroneuromyography is the most accurate tool in diagnosing abnormal EBSLN conductivity. But it is technically difficult and barely applicable in routine practice. Recommended approaches to prevent injury include visual identification of the nerve and its trajectory, and electrostimulation with observation of CTM twitch, which may be a useful intraoperative tool in determining functional integrity of the EBSLN. IONM bears the additional benefits of prognostication, quantification, and documentation of neural function [4910]. However, nerve visualization is not easy while dissecting scar tissue during thyroid reoperations. Therefore, the risk of injury to both superior and inferior laryngeal nerves is a major concern of redo surgery [1011].
We hypothesized that nerve monitoring provides additional findings for the identification of the EBSLN and establishment of its functional integrity during both primary and redo thyroid surgery. In this study, we aimed to determine the visual and electrophysiological identification rates of the EBSLN during both primary and redo thyroid surgery. The EBSLN identification rates between patients with primary and redo thyroid surgery were also compared to establish the effect of reoperations in the thyroid bed on both visual and functional identification of the EBSLN.
Hospital records of thyroidectomy cases were retrospectively reviewed to determine thyroid reoperations with IONM in the last six years. A total of 100 patients with thyroid reoperations were retrieved after chart review. We aimed to study the effects of recurrent thyroid pathology and previous surgery on the visual and functional identification rates of the EBSLN during redo thyroid surgery. The present study was approved by institutional review board (approval number: 2018-09-01) of Department of Surgery, Duzce University, Medical Faculty. Written informd consent was obtained from each patient before surgery.
A total of 138 EBSLNs were at risk in 100 patients with redo thyroid surgery. Visual and functional identification of these nerves by IONM was attempted during reoperations. The functional integrity of the EBSLNs was confirmed and evaluated using IONM by observing the transmission of electricity to the CTM in which twitches were created by electrophysiological stimulus.
To compare the results of thyroid reoperations with those of primary thyroid surgery, we conducted the same study on the last 100 consecutive patients who underwent primary thyroid surgery. A total of 170 EBSLNs were at risk in these patients. Anatomical identification and electrophysiological monitoring of the EBSLN were attempted during primary thyroid surgery. The functional integrity of EBSLNs was evaluated and confirmed using IONM by observing CTM contractions after electrophysiological stimulus.
Dissection was performed using a binocular loupe (magnification, ×2.5). The sternothyroid muscle was retracted upwards and laterally. After lateral and caudal traction of the upper pole of the thyroid, a dissection window was opened between the gland and inferior constrictor muscle. Upper thyroidal vessels were ligated close to the glandular tissue in the sternothyroid–laryngeal triangle under guidance of nerve monitoring. During and after full mobilization of the upper pole, we attempted to visually identify the EBSLN and assess its motor function by IONM in the triangle and on the constrictor muscle. The nerve branch was generally identified parallel to the insertion line of the sternothyroid muscle onto the thyroid cartilage. The visual and functional identification rates of the EBSLN were determined at the end of lobe dissection.
The dissection plane between the upper pole of the thyroid and inferior constrictor muscle was carefully observed to visually identify the EBSLN, and functional identification was then performed using IONM before ligation of vascular branches. After full mobilization of the upper pole and at the end of surgery, functional integrity of the EBSLN was examined by IONM. The stimulator probe was directly applied on the EBSLN if it was visualized. If the nerve was not clearly visualized, then the nerve tract on the constrictor muscle was indirectly stimulated to create and observe the physiological response of the CTM.
Functional evaluation of the EBSLN after electrophysiological stimulation was performed using 1 of the following 2 alternatives:
(1) Stimulation of the EBSLN produced contractions of the CTM whose muscular twitch was macroscopically observed. OR (2) Any response was not observed after EBSLN stimulation. Contraction of the CTM represents the functional integrity of the EBSLN.
We studied the following aspects: (1) Visual identification rate of the EBSLN and the results of IONM of visualized nerves, (2) functional identification rate of nonvisualized EBSLNs by IONM, (3) contribution of functional identification of the EBSLN by IONM to its visual identification.
Female patients constituted 94.4% and 78% of redo surgery and primary surgery cases, respectively. The average age of patients with reoperative thyroidectomy was 46.4 years (Table 1). Mean time between primary and secondary thyroid surgery was 26 years (range, 11–47 years).
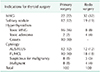
A total of 100 patients with recurrent disease were surgically treated in this study. The main indication for surgery was multinodular goiter in 32 patients (32%). Their results were compared with those of 100 primary thyroid surgery cases of which indications for surgery was multinodular goiter in 22 patients (22%). In addition to physical examination and imaging findings, the results of cytology from thyroid nodules indicated surgery in 37 patients (37%) of the redo surgery and in 38 patients (38%) of the primary surgery group. Cytological diagnosis included atypia of undetermined significance, indeterminate, suspicious or malignant results (Table 2).
Among patients with recurrent disease, 138 lateral lobes (86 right and 52 left) were explored, dissected, and completely excised in redo thyroid surgery. Among the patients with primary thyroid surgery, 170 lateral lobes (82 right and 88 left) were excised. Therefore, the total number of EBSLNs at risk was 170 and 138 in primary and recurrent cases, respectively (Table 3).
We first tried to visually identify the EBSLN during upper pole dissection. Visual identification rates were 30.4% and 65.3% in redo and primary surgery cases, respectively (P < 0.001). Electrophysiological stimulation of all visually identified nerve branches generated CTM contractions that showed functional integrity. In addition to visual identification, nonvisualized nerve branches were functionally discovered in 53 (31.2%) and 55 nerves (39.9%) by IONM alone in the primary and redo surgery groups, respectively. In total, 164 (96.5%) and 97 (70.3%) EBSLNs (P < 0.001) were identified with contribution of IONM in the primary and redo surgery groups, respectively (Table 4). We compared contribution of the IONM to EBSLN identification between the two groups. In primary surgery group, 53 nonvisualized EBSLNs (32.3%) of 164 identified nerves were determined by IONM alone. In redo surgery group, 55 (56.7%) of 97 identified nerves were determined by IONM alone (P < 0.001) (Table 5).
Total thyroidectomy provides radical excision of the gland without leaving any tissue behind so that the risk of recurrent disease is completely eliminated. Unfortunately, subtotal thyroidectomy carries a considerable lifelong risk of recurrence for some patients after a long interval; more than mean 25 years in our present series. The surgical treatment of such recurrences is affected by higher morbidity than primary thyroidectomy [12131415]. The best management of recurrent thyroid pathology is its prevention by primary total thyroidectomy, which is considered the preferred surgical approach as it abolishes the risk of recurrence and need for future revision intervention [1314]. Preservation of functional integrity of EBSLN is important for proper vocal cord (VC) function and voice quality. In our present work, we attempted to assess the visual and functional identification rates, and establish motor integrity of EBSLNs by nerve monitoring during both primary and redo thyroid surgery.
Our results demonstrated that visual identification of the EBSLN in primary thyroid surgery was possible in the great majority of patients during upper pole dissection of the gland. Appropriate dissection close to the thyroidal tissue allowed the identification of the EBSLN running distally on the pharyngeal constrictor muscle, parallel to insertion of the sternothyroid muscle on the thyroid cartilage. The nerve branches were established until CTM in approximately 2/3 of patients. Lennquist et al. [16] reported a visualization rate of up to 80%, and 20% of EBSLNs run distally through the pharyngeal constrictor muscle. Friedman et al. [17] reported an EBSLN visualization rate of 85.1%, and they found that the remaining branches run deep into the inferior constrictor muscle fibers. Recent studies have reported that the EBSLN can be visually identified in up to 93% of thyroidectomy cases [131819202122]. Despite anatomical integrity, adequate motor function of the nerve branch may not always be confirmed. In the present study, IONM was used to confirm functional integrity of visually identified nerve branches in which contractions of CTM were observed after direct application of the stimulator probe on the nerve branches. CTM twitch inspection could be a useful intraoperative tool to determine functional integrity of the EBSLN [4]. Some nonvisualized nerve branches lying under the constrictor muscle fibers may be discovered by electrophysiological monitoring. Our results showed that stimulation of the nerve tract in constrictor muscle provided functional identification of nonvisualized external branches. In our primary surgery cases, an additional identification rate of 31.2% of nonvisualized branches by IONM revealed the significant contribution of nerve monitoring to EBSLN identification during upper pole dissection. Recent studies have reported an IONM contribution rate of up to 50% [13181920232425]. Therefore, on the basis of our results in primary thyroid surgery, functional identification rates of the EBSLN could exceed 95% due to appropriate anatomical dissection and proper use of electrophysiological monitoring. Previous studies have reported the successful identification of the EBSLN with the assistance of IONM [118192021222627]. After significant advances and improvements in anatomical knowledge, surgical technique, and electrophysiological monitoring, the EBSLN identification rate has been reported to reach more than 90% in recent studies [34222328].
Disturbed anatomy due to primary surgery significantly affects results of anatomical dissection during redo surgery. The neural structures are vulnerable to injury in thyroid reoperations because of the presence of scar tissue and displacement of the nerve from its normal position [6101314]. In the present study, we noted obvious changes in the identification rate of the EBSLN in our reoperative surgery series. Our visual identification rate (65.3%) in the primary thyroid surgery group significantly decreased (30.4%) in the redo surgery. This result revealed the effect of local changes after previous surgical intervention. Our observations during redo surgery showed that wound contracture, fibrosis, and scar tissue significantly affected structural anatomy in the thyroid bed including neural anatomy. Contrary to studies on visual and functional identification of the EBSLN in primary thyroid surgery, we could not find any publication in the literature about EBSLN identification in redo thyroid surgery. Our results on the anatomical identification rate of the EBSLN during secondary operations were lower than those during primary thyroid surgery. Total identification rates of the EBSLN also decreased (96.5% vs. 70.3%) in patients with redo surgery. IONM makes a considerable and important contribution to the identification of the EBSLN in both primary and secondary surgery. The contribution of IONM becomes significant to such a degree that when comparing the 2 groups for functionally identified nerves, 53 of 164 EBSLNs (32.3%) in primary surgery group and 55 of 97 EBSLNs (56.7%) in redo group were identified by IONM alone (P < 0.001). In the literature, many studies have investigated RLN identification, dissection, and exposition in thyroid reoperations. In redo surgery, anatomy, anatomical changes, monitoring, morbidity, complication rate, and IONM have been studied regarding only the RLN [61011122930]. Contrary to identification of the EBSLN in primary cases, we could not find any publication about visual and functional identification and electrophysiological monitoring of the EBSLN in redo thyroid surgery. Therefore, we were unable to compare our results of EBSLN identification and monitoring in redo surgery with those of other researchers. In addition to primary cases, the functional integrity of the nerve should also be confirmed with IONM in secondary operations. We used nerve monitoring in all thyroid surgery cases regardless of primary or redo status of surgery. IONM seems as a good adjunct to the usual anatomical identification and exposure of neural structures, which is the gold standard of thyroid surgery. However, extensive experience in thyroid surgery should still be considered the most important factor for approaching redo thyroid surgery.
The present study has some limitations: In the current study all primary and redo surgeries were performed by the same surgeon and surgical team under guidance of IONM. Additionally, primary surgery of patients with thyroid reoperations were performed many years ago at different institutions, and by various surgeons. Therefore, factors related to previous surgical procedures and the surgical skill and experience of the surgeons were difficult to identify. Many years ago, primary surgeries on patients with recurrent goiter were performed without IONM. We have no information about neural identification rates during primary surgery and postoperative course of these patients.
In conclusion, EBSLN could be visually identified in the majority of cases during primary thyroid surgery by experienced surgeons. Functional identification of external branches by IONM makes a considerable contribution to anatomical identification during upper pole dissection of the gland. However, some unfavorable developments after primary surgery make both visual and functional identification of the EBSLN challenging in redo thyroid surgery. Electrophysiological monitoring also makes a substantial contribution to identification rates of nerve branches in secondary operations. IONM should be used, as a good adjunct to anatomical dissection and exposure, both in primary and redo surgery to identify the EBSLN and to confirm its functional integrity. In cases of disturbed anatomy after primary surgery, support of ancillary electrophysiological technology is beneficial in justifying the neural functional status during redo surgery.
Figures and Tables
Table 2
Preoperative diagnosis and indications for thyroid surgery in patients with primary and redo thyroid surgery
References
1. Hurtado-Lopez LM, Diaz-Hernandez PI, Basurto-Kuba E, Zaldivar-Ramirez FR, Pulido-Cejudo A. Efficacy of intraoperative neuro-monitoring to localize the external branch of the superior laryngeal nerve. Thyroid. 2016; 26:174–178.

2. Barczynski M, Randolph GW, Cernea C. International Neural Monitoring Study Group in Thyroid and Parathyroid Surgery. International survey on the identification and neural monitoring of the EBSLN during thyroidectomy. Laryngoscope. 2016; 126:285–291.
3. Gurleyik E, Gurleyik G. Intraoperative monitoring of external branch of the superior laryngeal nerve: functional identification, motor integrity, and its role on vocal cord function. J Invest Surg. 2017; 09. 27. 1–6. DOI: 10.1080/08941939.2017.1362489. [Epub].

4. Sung ES, Chang JH, Kim J, Cha W. Is cricothyroid muscle twitch predictive of the integrity of the EBSLN in thyroid surgery? Laryngoscope. 2018; 128:2654–2661.

5. Liddy W, Barber SR, Cinquepalmi M, Lin BM, Patricio S, Kyriazidis N, et al. The electrophysiology of thyroid surgery: electrophysiologic and muscular responses with stimulation of the vagus nerve, recurrent laryngeal nerve, and external branch of the superior laryngeal nerve. Laryngoscope. 2017; 127:764–771.

6. Gurleyik E, Cetin F, Dogan S, Yekenkurul E, Onsal U, Gursoy F, et al. Displacement of the recurrent laryngeal nerve in patients with recurrent goiter undergoing redo thyroid surgery. J Thyroid Res. 2018; 2018:4763712.

7. Sakorafas GH, Kokoropoulos P, Lappas C, Sampanis D, Smyrniotis V. External branch of the superior laryngeal nerve: applied surgical anatomy and implications in thyroid surgery. Am Surg. 2012; 78:986–991.

8. Hwang SB, Lee HY, Kim WY, Woo SU, Lee JB, Bae JW, et al. The anatomy of the external branch of the superior laryngeal nerve in Koreans. Asian J Surg. 2013; 36:13–19.

9. Potenza AS, Araujo Filho VJF, Cernea CR. Injury of the external branch of the superior laryngeal nerve in thyroid surgery. Gland Surg. 2017; 6:552–562.

10. Wojtczak B, Barczynski M. Intermittent neural monitoring of the recurrent laryngeal nerve in surgery for recurrent goiter. Gland Surg. 2016; 5:481–489.

11. Sopinski J, Kuzdak K, Hedayati M, Kolomecki K. Role of intraoperative neuromonitoring of the recurrent laryngeal nerves during thyroid reoperations of recurrent goiter. Pol Przegl Chir. 2017; 89:11–15.

12. Barczynski M, Konturek A, Pragacz K, Papier A, Stopa M, Nowak W. Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: results of a retrospective cohort study. World J Surg. 2014; 38:599–606.

13. Cappellani A, Zanghi A, Cardi F, Cavallaro A, Piccolo G, Palmucci S, et al. Total thyroidectomy: the first, the best. The recurrent goiter issue. Clin Ter. 2017; 168:e194–e198.
14. Barczynski M, Konturek A, Hubalewska-Dydejczyk A, Gołkowski F, Nowak W. Tenyear follow-up of a randomized clinical trial of total thyroidectomy versus dunhill operation versus bilateral subtotal thyroidectomy for multinodular non-toxic goiter. World J Surg. 2018; 42:384–392.

15. Miccoli P, Frustaci G, Fosso A, Miccoli M, Materazzi G. Surgery for recurrent goiter: complication rate and role of the thyroid-stimulating hormone-suppressive therapy after the first operation. Langenbecks Arch Surg. 2015; 400:253–258.

16. Lennquist S, Cahlin C, Smeds S. The superior laryngeal nerve in thyroid surgery. Surgery. 1987; 102:999–1008.
17. Friedman M, LoSavio P, Ibrahim H. Superior laryngeal nerve identification and preservation in thyroidectomy. Arch Otolaryngol Head Neck Surg. 2002; 128:296–303.

18. Lifante JC, McGill J, Murry T, Aviv JE, Inabnet WB 3rd. A prospective, randomized trial of nerve monitoring of the external branch of the superior laryngeal nerve during thyroidectomy under local/regional anesthesia and IV sedation. Surgery. 2009; 146:1167–1173.

19. Barczynski M, Konturek A, Stopa M, Honowska A, Nowak W. Randomized controlled trial of visualization versus neuromonitoring of the external branch of the superior laryngeal nerve during thyroidectomy. World J Surg. 2012; 36:1340–1347.

20. Glover AR, Norlen O, Gundara JS, Morris M, Sidhu SB. Use of the nerve integrity monitor during thyroid surgery aids identification of the external branch of the superior laryngeal nerve. Ann Surg Oncol. 2015; 22:1768–1773.

21. Ravikumar K, Sadacharan D, Muthukumar S, Mohanpriya G, Hussain Z, Suresh RV. EBSLN and factors influencing its identification and its safety in patients undergoing total thyroidectomy: a study of 456 cases. World J Surg. 2016; 40:545–550.

22. Aleksova L, Ali MM, Chakarov DI, Yozgyur ZM. Identification of the external branch of the superior laryngeal nerve during thyroid surgery. Folia Med (Plovdiv). 2018; 60:154–157.

23. Engelsman AF, Warhurst S, Fraser S, Novakovic D, Sidhu SB. Influence of neural monitoring during thyroid surgery on nerve integrity and postoperative vocal function. BJS Open. 2018; 2:135–141.

24. Lee J, Fraser S, Glover A, Sidhu S. Prospective evaluation of the utility of routine neuromonitoring for an established thyroid surgical practice. ANZ J Surg. 2017; 87:E138–E142.

25. Darr EA, Tufano RP, Ozdemir S, Kamani D, Hurwitz S, Randolph G. Superior laryngeal nerve quantitative intraoperative monitoring is possible in all thyroid surgeries. Laryngoscope. 2014; 124:1035–1041.

26. Menon RR, Murali S, Nair CG, Babu MJC, Jacob P. Correlation between the Cernea classification of external branch of superior laryngeal nerve in relation to the ultrasound-based volume of thyroid gland. Indian J Endocrinol Metab. 2017; 21:845–847.

27. Kim SJ, Lee KE, Oh BM, Oh EM, Bae DS, Choi JY, et al. Intraoperative neuromonitoring of the external branch of the superior laryngeal nerve during robotic thyroid surgery: a preliminary prospective study. Ann Surg Treat Res. 2015; 89:233–239.

28. Gavid M, Dubois MD, Larive E, Prades JM. Superior laryngeal nerve in thyroid surgery: anatomical identification and monitoring. Eur Arch Otorhinolaryngol. 2017; 274:3519–3526.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download