INTRODUCTION
Cervical cancer is a major worldwide health problem of women especially in developing countries. In Thailand, it is the second most common female cancer after breast cancer and remains the leading cause of death among women. An average age standardized incidence rate was 29.2 per 100,000 women with a death rate of 15.2 per 100,000 women or approximately half of its incidence [
1]. This is probably due to a suboptimal screening coverage of the target population, leading to a high proportion of locally advanced and advanced stage diseases and poor overall prognosis [
2].
Concurrent chemoradiation therapy (CCRT) has been used as a standard treatment for locally advanced cervical cancer (LACC) for over two decades. Despite a survival improvement with an addition of concurrent chemotherapy to radiation, high rates of local and distant failures (17% and 18%, respectively) were still encountered [
3]. A search for other treatments to improve treatment outcomes in this particular group of cervical cancer patients is important.
Many treatment modifications which have been used with CCRT were adding novel targeted agents with chemotherapy, using other chemotherapeutic regimens either alone or in combination with the standard platinum drug, modifying the dose or schedule of chemotherapy, or giving additional chemotherapy (adjuvant or consolidation chemotherapy) after CCRT.
The role of additional chemotherapy after CCRT for LACC has been explored in many studies [
4567]. Although all prospective phase II studies showed an increased response rate with adjuvant or consolidation chemotherapy with high 80%–90% survival rates [
4567], the 3 randomized controlled trials of adjuvant chemotherapy (ACT) had inconsistent data [
8910]. Two trials showed increased progression-free survival (PFS) or disease-free survival (DFS) using ACT after CCRT [
910] whereas the other trial could not demonstrate such a benefit [
8].
This trial aimed to assess the efficacy of ACT after CCRT compared to standard treatment of CCRT alone. The primary outcome was PFS whereas the secondary outcomes were response rate, overall survival (OS), quality of life and cost-utility of ACT. Quality of life and cost-utility of ACT were presented elsewhere.
DISCUSSION
Because CCRT which is the current standard treatment for LACC could yield only 60%–65% survival rate [
3], other alternative treatments were considered. One option was to give additional chemotherapy after the completion of CCRT in order to eradicate any residual tumor either inside the pelvis or beyond.
This trial gave additional chemotherapy with paclitaxel and carboplatin for 3 more cycles after CCRT. However, the results did not show any improvement of PFS or OS by ACT. On the contrary, the patients who had additional ACT had lower 3-year PFS (3.2%) and 3-year OS (10.6%) compared to those who had only standard CCRT. Although the differences were not statistically significant, these were rather unexpected. The bootstrap analysis confirmed uncertainty in outcomes, suggesting a non-significant difference of the 2 types of intervention. Further recruitment and a certain period of follow-up would be unlikely to provide a definite answer and would be inappropriate in our country setting with limited resources.
The inconclusive results from this trial added more uncertainty to the unanswered question regarding the role of ACT after CCRT. Findings from the 3 previous randomised controlled trials (RCTs) comparing CCRT to CCRT and ACT were inconsistent [
8910]. Two trials showed significant survival benefit of ACT over CCRT alone [
910]. One of which was an international collaboration reported 9% (74% vs. 65%) 3-year PFS and 11% (80% vs. 69%) 3-year OS improvement by the use of ACT [
9] whereas another trial from China reported 11% 5-year DFS improvement (71% vs. 60%) with 7% lesser deaths (26% vs. 33%) [
10]. However, there was a discrepancy of standard treatment between the 2 randomized arms of both trials. One trial gave combined chemotherapeutic drugs during CCRT (cisplatin plus gemcitabine) before ACT of the same regimen in the study arm compared to single agent (cisplatin) during CCRT before observation in the control arm [
9] whereas another trial gave neoadjuvant chemotherapy (cisplatin plus paclitaxel) prior to CCRT (cisplatin) then ACT (cisplatin plus paclitaxel) compared to CCRT alone (cisplatin) [
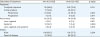
10]. These discrepancies should be taken into account when considering the benefit of ACT. Data from these previous trials and our trial are summarized in
Table 5.
Table 5
Comparison of data of our trial and previous trials of ACT after concurrent chemoradiation in locally advanced cervical cancer

|
Features/trial |
Lorvidhaya et al., 2003 [8] |
Dueñas-González et al., 2011 [9] |
Tang et al., 2012 [10] |
This trial |
|
Number |
463†
|
515 |
880 |
259 |
|
Stage*
|
IIB to IVA |
IIB to IVA |
IIB to IVA |
IIB to IVA |
|
Other pre-requisites |
Tumor in IIB >3 cm or involved >1/2 PRM (imaging not required) |
Patients with PAN >1 cm must be FNA negative |
Patients with +ve PAN from CT scan had EFRT |
Excluded patients with +ve PAN from imaging |
|
Histopathology |
SCC, ACA |
SCC, ACA, AS |
ACA only |
SCC, ACA, AS |
|
Neoadjuvant CMT |
None |
None |
Paclitaxel/cisplatin 1 cycle |
None |
|
Concurrent CMT |
Mitomycin/oral 5-FU in both arms |
Cisplatin in CCRT arm |
Cisplatin in both arms |
Cisplatin in both arms |
|
Cisplatin/gemcitabine in ACT arm |
|
Adjuvant CMT |
Oral 5-FU 3 cycles |
Cisplatin/gemcitabine 2 cycles |
Paclitaxel/cisplatin 2 cycles |
Paclitaxel/carboplatin 3 cycles |
|
Incomplete Rx |
5% in CCRT arm |
0.4% in CCRT arm (during CCRT) |
None |
4% in CCRT arm (during CCRT) |
|
8% in ACT arm (phase, NOS) |
5% (during CCRT), 24% (during ACT) in ACT arm |
6% (during CCRT), 36% (during ACT) in ACT arm |
|
Outcomes |
|
|
|
|
|
Median follow-up |
89 mo |
46.9 mo |
60 mo (range 9–120 mo) |
27.4 mo (range, 3.2–49.0 mo) |
|
Tumor response |
NA |
CCRT vs. ACT (timing after CCRT) |
CCRT vs. ACT (timing after CCRT) |
CCRT vs. ACT (timing after CCRT) |
|
93% (1 mo) vs. 96% (3 mo) |
47% vs. 71% (after CCRT ended) |
59% vs. 42% (after CCRT ended) |
|
75% vs. 86% (1 mo) |
75% vs. 58% (1 mo) |
|
75% vs. 96% (3 mo) |
88% vs. 68% (3 mo) |
|
94% vs. 87% (4 mo) |
|
Survival |
No benefit of ACT after CCRT
|
HRs=0.68 (p=0.02; 95% CI=0.49–0.95) for both PFS & OS in favor ACT arm |
5-yr DFS: 63% CCRT arm vs. 75% ACT arm (p<0.05) |
3-yr PFS: 67% CCRT vs. 63% ACT arm |
|
3-yr OS: 80% CCRT vs. 63% ACT arm |
|
Sites of failure |
Slightly higher failure at all sites in ACT arm (NS) |
Lower failure at all sites in ACT arm (sig. only distant failure) |
Lower failure at all sites in ACT arm (sig. in all differences) |
Lower only distant failure in ACT arm (sig.) |

Although the results from our study were similar to the findings of 1 trial from Thailand which showed insignificantly lower 5-year DFS (60% vs. 65%) and 5-year OS among the patients who had ACT than those who had only CCRT [
8], the underlying reasons may be different. The possible reason for negative findings in their trial was the questionable compliance of oral 5-FU which was used as an ACT [
8].
There were a few possible reasons that our study could not demonstrate the benefit of ACT in LACC patients. First, the chemotherapeutic regimen of paclitaxel and carboplatin may not be effective. Previous trials used different chemotherapy regimens in the concurrent phase with radiation and/or the adjuvant phase: mitomycin C with oral 5-FU [
8], cisplatin with paclitaxel [
10] or with gemcitabine [
9]. Instead of paclitaxel and cisplatin which showed similar efficacy with other doublets chemotherapy in a randomized controlled trial of advanced or recurrent cervical cancer [
11], our study selected paclitaxel and carboplatin as ACT because of its convenience and feasibility in administration. Furthermore, we assumed from available data of the non-inferior activity of this chemotherapeutic regimen in cervical cancer [
1213]. Upon a careful re-scrutinization, most data which showed comparable efficacy of the 2 regimens were derived from retrospective [
12] or a systemic review including only retrospective or phase II studies [
13], and only 1 randomized trial [
14]. Furthermore, data from 1 randomized trial demonstrated that paclitaxel/carboplatin was inferior to paclitaxel/cisplatin in advanced non-small cell lung cancer [
15]. More evidence-based data of this chemotherapy regimen' efficacy in cervical cancer may be needed. Second, the chemotherapy cycles may be inadequate. An example is the ACT in epithelial ovarian cancer which is generally given for 6 or more cycles to maximize the efficacy especially in advanced stages. Our group postulated that 3 cycles of additional chemotherapy should be adequate to demonstrate the efficacy of the adjuvant treatment. Furthermore, the extended duration of approximately 3 months would not be too long to burden the patients and their family, and the direct and indirect medical cost incurred would not be too high. Third, a possible selective benefit of ACT on a more advanced stage or certain histopathology (adenocarcinoma in particular) was diluted by including stage II patients or squamous cell carcinoma which comprised the major cervical cancer population whose diseases could be managed by CCRT alone. This was partly supported by findings from the study of Dueñas-González et al. [
9] which found a higher benefit of ACT in stage III–IV or adenocarcinoma. Although our subgroup analyses did not show any particular groups of patients who may have benefit from ACT, limited sample size precluded any conclusion. Another reason was that the ACT really had no benefit in LACC. This last reason was supported by data from the 2 alternative statistical means of per protocol and bootstrap analyses. Although a considerable number of patients were dropped out before treatment completion especially among those who were assigned to ACT, the results from per protocol and bootstrap analyses were consistent with those from the modified intention to treat analyses. Additionally, the insignificant findings could be due to the fact that the final sample size was lower than expected, which translated to uncertainty in findings on the impact of ACT on LACC patients.
Limitations of our study included poor compliance of the patients in the trial. The discontinuation rates during CCRT were not significantly different between 2 treatment arms. We found 17.6% of all patients who were randomized to have ACT did not have any ACT (or 18.7% among those who had complete CCRT). The main reason of the discontinuation in our study was rather from the patients' decision or lost to follow-up than from the toxicity. We postulated that the alleviation of symptoms after treatment combined with the deviation of daily lives activities coming to the hospital especially in a setting with long treatment duration of treatment might have influenced their decisions despite their consent to enter into the trial in the beginning. Furthermore, most Thai cervical cancer patients had low socioeconomic status and education, they were tempted to take herbal or alternative treatments despite non-proven efficacy. One previous study in an urban academic cancer center reported 20% non-compliance among patients who had radiation treatment [
16]. Having cervical or uterine cancer, low socioeconomic status, and a long treatment course were among several predicting factors of the non-compliance. Among the 3 previous trials, 1 trial found that all 880 cervical cancer patients in their study completed treatment [
10] whereas the other 2 trials reported the discontinuation rates [
89]. The trial of Lorvidhaya et al. [
8] reported 7% of the patients (5% in the CCRT and 8% in the ACT groups) had incomplete treatment. However, the authors did not detail the timing and reason of the discontinuation. Another trial of Dueñas-González et al. [
9] reported a significantly higher number of patients in the study arm discontinued treatment during the pre-adjuvant phase, most frequently from side effects (5% in the study arm vs. 0.4% in the control arm). This was rather predictable because their patients in the study arm had combination of chemotherapy (cisplatin with gemcitabine) in concurrent with pelvic radiation compared to those in the control arm who had only a single agent (cisplatin) [
9]. Toxicity was also a reason for the ACT omission or discontinuation in their study which was reported in 14% and 10% respectively [
9].
In an assessment of response rates, we were aware of the delayed efficacy of radiation therapy. Hence, our study explored the tumor shrinkage at 4 different time points after CCRT. This was found in our study as the tumors shrank over time in both arms. Although the rates of tumor shrinkage were observed to be significantly higher in arm A than in arm B during the first 3 months (despite a balance of characteristic features between both arms), the magnitudes of incremental response between the assessments were higher in arm B especially at the fourth evaluation (a time point in determining tumor response) leading to a non-significant difference of the response rates at 4 months after CCRT or approximately 1 month after the last cycle of ACT. This may be considered as indirect evidence for the benefit of ACT especially when all 3 cycles could be given. Among the 3 RCTs comparing standard CCRT and CCRT followed by ACT, only 2 trials which reported the response outcomes had inconsistent findings [
910]. The international trial by Dueñas-Gonzalez et al. [
9] who did not find significant differences in response rates between the patients who had only CCRT or CCRT and ACT, 93% vs. 96%. These comparable response rates were despite the disparity of concurrent chemotherapy during radiation treatment. Another study from China found significantly higher response rate in the patients who had additional chemotherapy [
10]. The response rates evaluated at 1 month after CCRT were 75% in the CCRT group and 86% in the ACT group. The rate increased to 96% in the latter group after ACT. However, the benefit of ACT in this trial was questionable because the study arm also had 1 cycle of paclitaxel and cisplatin as the neoadjuvant chemotherapy before CCRT and 2 more cycles of ACT [
10].
Theoretically, ACT after CCRT in LACC should increase local pelvic control and decrease systemic failure. A significant lower systemic failure in the patients who had ACT in our study (
Table 3) was consistent with findings in the 2 trial of Dueñas-González et al. [
9] and Tang et al. [
10] who also found significantly lower distant failure with an addition of ACT compared to only CCRT: 8%–14% vs. 16%–24%. The only trial of Lorvidhaya et al. [
8] found no benefit of ACT on the overall failure rate (29% by CCRT vs. 31% by CCRT and ACT) or the sites of failure (14% and 18% of loco-regional and 18% vs. 20% distant failures). The oral chemotherapeutic drug used in this last trial may preclude the benefit ACT if any.
Concerning the toxicity of the additional treatment, our study found higher frequency of adverse events in arm B than in arm B (
Table 4). However, some adverse events found in the ACT arm may be the prolonged effects from the CCRT and the figures may not the genuine effect for ACT itself. Anyway, grade 3–4 toxicities were infrequent in both arms with hematologic toxicity as the most common adverse events reported. The 3 previous trials of ACT which reported acute with or without long-term adverse events found slightly higher (not significant) among the patients who had ACT [
8910]. Our long-term adverse events as well as quality of life of the patients were collected and would be reported along with the long-term survival outcomes in another report.
In conclusion, no significant benefit of paclitaxel with carboplatin given for 3 cycles after a standard concurrent chemoradiation treatment for LACC was demonstrated. Future studies might reconsider recruiting the patients with certain high-risk features, adjustment of chemotherapy regimen or cycles, or other alternative treatment options to improve survival outcomes of these patients. Adaptive randomization in favor of standard treatment with CCRT may also be considered.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download