1. Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992; 17:528–540. PMID:
1621152.
2. Gertzbein SD, Khoury D, Bullington A, St John TA, Larson AI. Thoracic and lumbar fractures associated with skiing and snowboarding injuries according to the AO comprehensive classification. Am J Sports Med. 2012; 40:1750–1754. PMID:
22700890.

3. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994; 3:184–201. PMID:
7866834.

4. Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 1996; 10:541–544. PMID:
8915916.

5. Moutinho R, Tyrrell P, Cassar-Pullicino VN. Emergency and trauma imaging of the thoracolumbar spine. Semin Musculoskelet Radiol. 2017; 21:199–209. PMID:
28571085.

6. Ballock RT, Mackersie R, Abitbol JJ, Cervilla V, Resnick D, Garfin SR. Can burst fractures be predicted from plain radiographs? J Bone Joint Surg Br. 1992; 74:147–150. PMID:
1732246.

7. Hauser CJ, Visvikis G, Hinrichs C, Eber CD, Cho K, Lavery RF, et al. Prospective validation of computed tomographic screening of the thoracolumbar spine in trauma. J Trauma. 2003; 55:228–234. discussion 234–235. PMID:
12913630.

8. Wintermark M, Mouhsine E, Theumann N, Mordasini P, van Melle G, Leyvraz PF, et al. Thoracolumbar spine fractures in patients who have sustained severe trauma: depiction with multi-detector row CT. Radiology. 2003; 227:681–689. PMID:
12702827.

9. Pizones J, Zúñiga L, Sánchez-Mariscal F, Alvarez P, Gómez-Rice A, Izquierdo E. MRI study of post-traumatic incompetence of posterior ligamentous complex: importance of the supraspinous ligament. Prospective study of 74 traumatic fractures. Eur Spine J. 2012; 21:2222–2231. PMID:
22722921.

10. Pizones J, Izquierdo E, Alvarez P, Sánchez-Mariscal F, Zúñiga L, Chimeno P, et al. Impact of magnetic resonance imaging on decision making for thoracolumbar traumatic fracture diagnosis and treatment. Eur Spine J. 2011; 20(Suppl 3):390–396. PMID:
21779855.

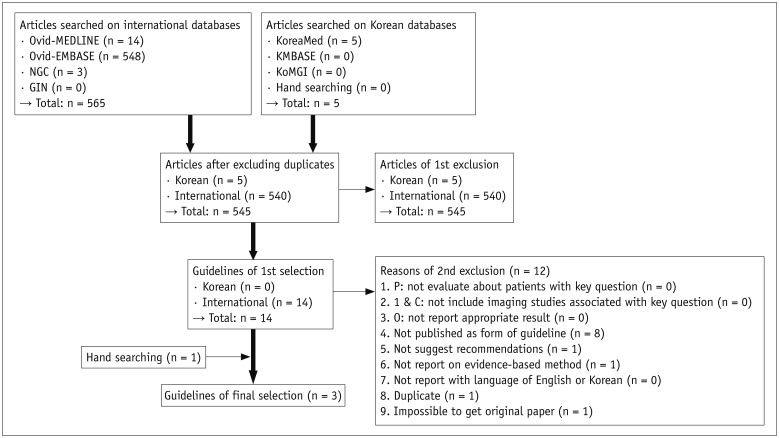
11. Choi SJ, Jeong WK, Jo AJ, Choi JA, Kim MJ, Lee M, et al. Methodology for developing evidence-based clinical imaging guidelines: joint recommendations by Korean Society of Radiology and National Evidence-based Healthcare Collaborating Agency. Korean J Radiol. 2017; 18:208–216. PMID:
28096730.

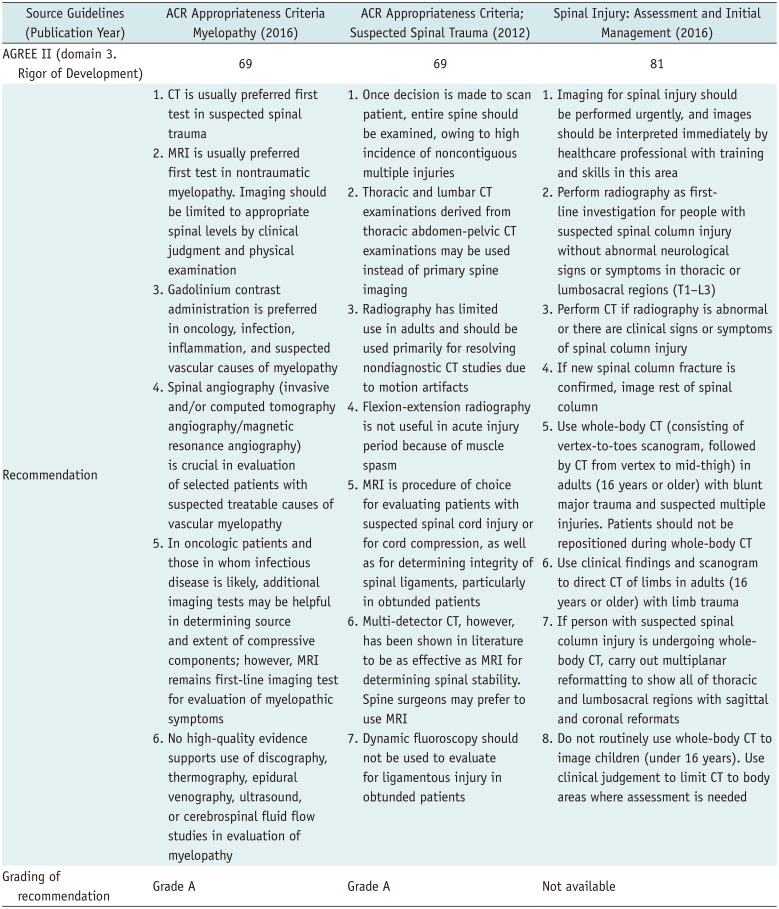
13. Roth CJ, Angevine PD, Aulino JM, Berger KL, Choudhri AF, Fries IB, et al. ACR appropriateness criteria myelopathy. J Am Coll Radiol. 2016; 13:38–44. PMID:
26653797.

14. Daffner RH, Hackney DB. ACR Appropriateness Criteria® on suspected spine trauma. J Am Coll Radiol. 2007; 4:762–775. PMID:
17964500.

15. National Clinical Guideline Centre (UK). Spinal injury: assessment and initial management. London: National Institute for Health and Care Excellence;2016.
16. Chang CH, Holmes JF, Mower WR, Panacek EA. Distracting injuries in patients with vertebral injuries. J Emerg Med. 2005; 28:147–152. PMID:
15707808.

17. Dai LY, Yao WF, Cui YM, Zhou Q. Thoracolumbar fractures in patients with multiple injuries: diagnosis and treatment-a review of 147 cases. J Trauma. 2004; 56:348–355. PMID:
14960979.

18. Hsu JM, Joseph T, Ellis AM. Thoracolumbar fracture in blunt trauma patients: guidelines for diagnosis and imaging. Injury. 2003; 34:426–433. PMID:
12767788.

19. Brown CV, Antevil JL, Sise MJ, Sack DI. Spiral computed tomography for the diagnosis of cervical, thoracic, and lumbar spine fractures: its time has come. J Trauma. 2005; 58:890–895. discussion 895–896. PMID:
15920398.

20. Berry GE, Adams S, Harris MB, Boles CA, McKernan MG, Collinson F, et al. Are plain radiographs of the spine necessary during evaluation after blunt trauma? Accuracy of screening torso computed tomography in thoracic/lumbar spine fracture diagnosis. J Trauma. 2005; 59:1410–1413. discussion 1413. PMID:
16394914.

21. Brandt MM, Wahl WL, Yeom K, Kazerooni E, Wang SC. Computed tomographic scanning reduces cost and time of complete spine evaluation. J Trauma. 2004; 56:1022–1026. discussion 1026–1028. PMID:
15179241.

22. Herzog C, Ahle H, Mack MG, Maier B, Schwarz W, Zangos S, et al. Traumatic injuries of the pelvis and thoracic and lumbar spine: does thin-slice multidetector-row CT increase diagnostic accuracy? Eur Radiol. 2004; 14:1751–1760. PMID:
15300395.

23. Lucey BC, Stuhlfaut JW, Hochberg AR, Varghese JC, Soto JA. Evaluation of blunt abdominal trauma using PACS-based 2D and 3D MDCT reformations of the lumbar spine and pelvis. AJR Am J Roentgenol. 2005; 185:1435–1440. PMID:
16303994.

24. Sheridan R, Peralta R, Rhea J, Ptak T, Novelline R. Reformatted visceral protocol helical computed tomographic scanning allows conventional radiographs of the thoracic and lumbar spine to be eliminated in the evaluation of blunt trauma patients. J Trauma. 2003; 55:665–669. PMID:
14566120.

25. van Beek EJ, Been HD, Ponsen KK, Maas M. Upper thoracic spinal fractures in trauma patients - a diagnostic pitfall. Injury. 2000; 31:219–223. PMID:
10719098.

26. Dai LY, Wang XY, Jiang LS, Jiang SD, Xu HZ. Plain radiography versus computed tomography scans in the diagnosis and management of thoracolumbar burst fractures. Spine (Phila Pa 1976). 2008; 33:E548–E552. PMID:
18628696.

27. Karul M, Bannas P, Schoennagel BP, Hoffmann A, Wedegaertner U, Adam G, et al. Fractures of the thoracic spine in patients with minor trauma: comparison of diagnostic accuracy and dose of biplane radiography and MDCT. Eur J Radiol. 2013; 82:1273–1277. PMID:
23422283.

28. Campbell SE, Phillips CD, Dubovsky E, Cail WS, Omary RA. The value of CT in determining potential instability of simple wedge-compression fractures of the lumbar spine. AJNR Am J Neuroradiol. 1995; 16:1385–1392. PMID:
7484620.
29. Krueger MA, Green DA, Hoyt D, Garfin SR. Overlooked spine injuries associated with lumbar transverse process fractures. Clin Orthop Relat Res. 1996; (327):191–195. PMID:
8641063.

30. Rhea JT, Sheridan RL, Mullins ME, Novelline RA. Can chest and abdominal trauma CT eliminate the need for plain films of the spine? - Experience with 329 multiple trauma patients. Emergency Radiology. 2001; 8:99–104.

31. Rhee PM, Bridgeman A, Acosta JA, Kennedy S, Wang DS, Sarveswaran J, et al. Lumbar fractures in adult blunt trauma: axial and single-slice helical abdominal and pelvic computed tomographic scans versus portable plain films. J Trauma. 2002; 53:663–667. discussion 667. PMID:
12394863.

32. Gestring ML, Gracias VH, Feliciano MA, Reilly PM, Shapiro MB, Johnson JW, et al. Evaluation of the lower spine after blunt trauma using abdominal computed tomographic scanning supplemented with lateral scanograms. J Trauma. 2002; 53:9–14. PMID:
12131382.

33. Inaba K, Munera F, McKenney M, Schulman C, de Moya M, Rivas L, et al. Visceral torso computed tomography for clearance of the thoracolumbar spine in trauma: a review of the literature. J Trauma. 2006; 60:915–920. PMID:
16612322.

34. Salim A, Sangthong B, Martin M, Brown C, Plurad D, Demetriades D. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: results of a prospective study. Arch Surg. 2006; 141:468–473. discussion 473–475. PMID:
16702518.
35. Mancini DJ, Burchard KW, Pekala JS. Optimal thoracic and lumbar spine imaging for trauma: are thoracic and lumbar spine reformats always indicated? J Trauma. 2010; 69:119–121. PMID:
20622586.

36. Smith MW, Reed JD, Facco R, Hlaing T, McGee A, Hicks BM, et al. The reliability of nonreconstructed computerized tomographic scans of the abdomen and pelvis in detecting thoracolumbar spine injuries in blunt trauma patients with altered mental status. J Bone Joint Surg Am. 2009; 91:2342–2349. PMID:
19797568.

37. Daffner RH, Sciulli RL, Rodriguez A, Protetch J. Imaging for evaluation of suspected cervical spine trauma: a 2-year analysis. Injury. 2006; 37:652–658. PMID:
16504194.

38. Hogan GJ, Mirvis SE, Shanmuganathan K, Scalea TM. Exclusion of unstable cervical spine injury in obtunded patients with blunt trauma: is MR imaging needed when multi-detector row CT findings are normal? Radiology. 2005; 237:106–113. PMID:
16183927.

39. Benzel EC, Hart BL, Ball PA, Baldwin NG, Orrison WW, Espinosa MC. Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. J Neurosurg. 1996; 85:824–829. PMID:
8893720.

40. Davis SJ, Khangure MS. A review of magnetic resonance imaging in spinal trauma. Australas Radiol. 1994; 38:241–253. PMID:
7993244.

41. O'Beirne J, Cassidy N, Raza K, Walsh M, Stack J, Murray P. Role of magnetic resonance imaging in the assessment of spinal injuries. Injury. 1993; 24:149–154. PMID:
8509179.
42. Silberstein M, Tress BM, Hennessy O. A comparison between M.R.I. and C.T. in acute spinal trauma. Australas Radiol. 1992; 36:192–197. PMID:
1445100.

43. Tracy PT, Wright RM, Hanigan WC. Magnetic resonance imaging of spinal injury. Spine (Phila Pa 1976). 1989; 14:292–301. PMID:
2711244.

44. Pizones J, Sánchez-Mariscal F, Zúñiga L, Álvarez P, Izquierdo E. Prospective analysis of magnetic resonance imaging accuracy in diagnosing traumatic injuries of the posterior ligamentous complex of the thoracolumbar spine. Spine (Phila Pa 1976). 2013; 38:745–775. PMID:
23089929.

45. Tarr RW, Drolshagen LF, Kerner TC, Allen JH, Partain CL, James AE Jr. MR imaging of recent spinal trauma. J Comput Assist Tomogr. 1987; 11:412–417. PMID:
3571580.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download