1. Cavallo MC, Sepe V, Conte F, Abelli M, Ticozzelli E, Bottazzi A, et al. Cost-effectiveness of kidney transplantation from DCD in Italy. Transplant Proc. 2014; 46:3289–3296. PMID:
25498039.

2. Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012; 379:815–822. PMID:
22386035.

3. Liu ZH. Nephrology in China. Nat Rev Nephrol. 2013; 9:523–528. PMID:
23877587.

4. Aubert O, Kamar N, Vernerey D, Viglietti D, Martinez F, Duong-Van-Huyen JP, et al. Long term outcomes of transplantation using kidneys from expanded criteria donors: prospective, population based cohort study. BMJ. 2015; 351:h3557. PMID:
26232393.

5. Goldberg RJ, Weng FL, Kandula P. Acute and chronic allograft dysfunction in kidney transplant recipients. Med Clin North Am. 2016; 100:487–503. PMID:
27095641.

6. Earley A, Miskulin D, Lamb EJ, Levey AS, Uhlig K. Estimating equations for glomerular filtration rate in the era of creatinine standardization: a systematic review. Ann Intern Med. 2012; 156:785–795. W-270W-271W-272W-273W-274W-275W-276W-277W-278PMID:
22312131.
7. Moreno CC, Mittal PK, Ghonge NP, Bhargava P, Heller MT. Imaging complications of renal transplantation. Radiol Clin North Am. 2016; 54:235–249. PMID:
26896222.

8. Azancot MA, Moreso F, Salcedo M, Cantarell C, Perello M, Torres IB, et al. The reproducibility and predictive value on outcome of renal biopsies from expanded criteria donors. Kidney Int. 2014; 85:1161–1168. PMID:
24284518.
9. Wang YT, Li YC, Yin LL, Pu H, Chen JY. Functional assessment of transplanted kidneys with magnetic resonance imaging. World J Radiol. 2015; 7:343–349. PMID:
26516431.

10. Ljimani A, Wittsack HJ. Functional MRI in transplanted kidneys. Abdom Radiol (NY). 2018; 43:2615–2624. PMID:
29556702.

11. Baliyan V, Das CJ, Sharma R, Gupta AK. Diffusion weighted imaging: technique and applications. World J Radiol. 2016; 8:785–798. PMID:
27721941.

12. Eisenberger U, Thoeny HC, Binser T, Gugger M, Frey FJ, Boesch C, et al. Evaluation of renal allograft function early after transplantation with diffusion-weighted MR imaging. Eur Radiol. 2010; 20:1374–1383. PMID:
20013274.

13. Kaul A, Sharma RK, Gupta RK, Lal H, Yadav A, Bhadhuria D, et al. Assessment of allograft function using diffusion-weighted magnetic resonance imaging in kidney transplant patients. Saudi J Kidney Dis Transpl. 2014; 25:1143–1147. PMID:
25394428.

14. Thoeny HC, Zumstein D, Simon-Zoula S, Eisenberger U, De Keyzer F, Hofmann L, et al. Functional evaluation of transplanted kidneys with diffusion-weighted and BOLD MR imaging: initial experience. Radiology. 2006; 241:812–821. PMID:
17114628.

15. Vermathen P, Binser T, Boesch C, Eisenberger U, Thoeny HC. Three-year follow-up of human transplanted kidneys by diffusion-weighted MRI and blood oxygenation level-dependent imaging. J Magn Reson Imaging. 2012; 35:1133–1138. PMID:
22180302.

16. Palmucci S, Mauro LA, Veroux P, Failla G, Milone P, Ettorre GC, et al. Magnetic resonance with diffusion-weighted imaging in the evaluation of transplanted kidneys: preliminary findings. Transplant Proc. 2011; 43:960–966. PMID:
21620026.

17. Palmucci S, Mauro LA, Failla G, Foti PV, Milone P, Sinagra N, et al. Magnetic resonance with diffusion-weighted imaging in the evaluation of transplanted kidneys: updating results in 35 patients. Transplant Proc. 2012; 44:1884–1888. PMID:
22974862.

18. Eisenberger U, Binser T, Thoeny HC, Boesch C, Frey FJ, Vermathen P. Living renal allograft transplantation: diffusion-weighted MR imaging in longitudinal follow-up of the donated and the remaining kidney. Radiology. 2014; 270:800–808. PMID:
24475796.

19. Kuai ZX, Liu WY, Zhu YM. Effect of multiple perfusion components on pseudo-diffusion coefficient in intravoxel incoherent motion imaging. Phys Med Biol. 2017; 62:8197–8209. PMID:
28914609.

20. Thoeny HC, De Keyzer F. Diffusion-weighted MR imaging of native and transplanted kidneys. Radiology. 2011; 259:25–38. PMID:
21436095.

21. Xie Y, Li Y, Wen J, Li X, Zhang Z, Li J, et al. Functional evaluation of transplanted kidneys with reduced field-of-view diffusion-weighted imaging at 3T. Korean J Radiol. 2018; 19:201–208. PMID:
29520177.

22. Sulkowska K, Palczewski P, Wojcik D, Ciszek M, Sanko-Resmer J, Wojtowicz J, et al. Intravoxel incoherent motion imaging in monitoring the function of kidney allograft. Acta Radiol. 2018; 9. 23. [Epub ahead of print]. DOI:
10.1177/0284185118802598.

23. Mori S, Zhang J. Principles of diffusion tensor imaging and its applications to basic neuroscience research. Neuron. 2006; 51:527–539. PMID:
16950152.

24. Morrell GR, Zhang JL, Lee VS. Magnetic resonance imaging of the fibrotic kidney. J Am Soc Nephrol. 2017; 28:2564–2570. PMID:
28784699.

25. Kido A, Kataoka M, Yamamoto A, Nakamoto Y, Umeoka S, Koyama T, et al. Diffusion tensor MRI of the kidney at 3.0 and 1.5 tesla. Acta Radiol. 2010; 51:1059–1063. PMID:
20735277.

26. Notohamiprodjo M, Dietrich O, Horger W, Horng A, Helck AD, Herrmann KA, et al. Diffusion tensor imaging (DTI) of the kidney at 3 tesla-feasibility, protocol evaluation and comparison to 1.5 tesla. Invest Radiol. 2010; 45:245–254. PMID:
20375845.

27. Cheung JS, Fan SJ, Chow AM, Zhang J, Man K, Wu EX. Diffusion tensor imaging of renal ischemia reperfusion injury in an experimental model. NMR Biomed. 2010; 23:496–502. PMID:
20175152.

28. Deger E, Celik A, Dheir H, Turunc V, Yardimci A, Torun M, et al. Rejection evaluation after renal transplantation using MR diffusion tensor imaging. Acta Radiol. 2018; 59:876–883. PMID:
28975804.

29. Hueper K, Khalifa AA, Bräsen JH, Vo Chieu VD, Gutberlet M, Wintterle S, et al. Diffusion-weighted imaging and diffusion tensor imaging detect delayed graft function and correlate with allograft fibrosis in patients early after kidney transplantation. J Magn Reson Imaging. 2016; 44:112–121. PMID:
26778459.

30. Palmucci S, Cappello G, Attinà G, Foti PV, Siverino RO, Roccasalva F, et al. Diffusion weighted imaging and diffusion tensor imaging in the evaluation of transplanted kidneys. Eur J Radiol Open. 2015; 2:71–80. PMID:
26937439.

31. Li Y, Lee MM, Worters PW, MacKenzie JD, Laszik Z, Courtier JL. Pilot study of renal diffusion tensor imaging as a correlate to histopathology in pediatric renal allografts. AJR Am J Roentgenol. 2017; 208:1358–1364. PMID:
28379715.

32. Kaimori JY, Isaka Y, Hatanaka M, Yamamoto S, Ichimaru N, Fujikawa A, et al. Diffusion tensor imaging MRI with spin-echo sequence and long-duration measurement for evaluation of renal fibrosis in a rat fibrosis model. Transplant Proc. 2017; 49:145–152. PMID:
28104123.

33. Hueper K, Gutberlet M, Rodt T, Gwinner W, Lehner F, Wacker F, et al. Diffusion tensor imaging and tractography for assessment of renal allograft dysfunction-initial results. Eur Radiol. 2011; 21:2427–2433. PMID:
21710264.

34. Lanzman RS, Ljimani A, Pentang G, Zgoura P, Zenginli H, Kropil P, et al. Kidney transplant: functional assessment with diffusion-tensor MR imaging at 3T. Radiology. 2013; 266:218–225. PMID:
23169797.

35. Fan WJ, Ren T, Li Q, Zuo PL, Long MM, Mo CB, et al. Assessment of renal allograft function early after transplantation with isotropic resolution diffusion tensor imaging. Eur Radiol. 2016; 26:567–575. PMID:
26017738.

36. Fukunaga I, Hori M, Masutani Y, Hamasaki N, Sato S, Suzuki Y, et al. Effects of diffusional kurtosis imaging parameters on diffusion quantification. Radiol Phys Technol. 2013; 6:343–348. PMID:
23536232.

37. Jensen JH, Helpern JA. MRI quantification of non-gaussian water diffusion by kurtosis analysis. NMR Biomed. 2010; 23:698–710. PMID:
20632416.

38. Raab P, Hattingen E, Franz K, Zanella FE, Lanfermann H. Cerebral gliomas: diffusional kurtosis imaging analysis of microstructural differences. Radiology. 2010; 254:876–881. PMID:
20089718.

39. Giannelli M, Toschi N. On the use of trace-weighted images in body diffusional kurtosis imaging. Magn Reson Imaging. 2016; 34:502–507. PMID:
26706136.

40. Huang Y, Chen X, Zhang Z, Yan L, Pan D, Liang C, et al. MRI quantification of non-gaussian water diffusion in normal human kidney: a diffusional kurtosis imaging study. NMR Biomed. 2015; 28:154–161. PMID:
25392938.

41. Pentang G, Lanzman RS, Heusch P, Müller-Lutz A, Blondin D, Antoch G, et al. Diffusion kurtosis imaging of the human kidney: a feasibility study. Magn Reson Imaging. 2014; 32:413–420. PMID:
24582288.

42. Kjølby BF, Khan AR, Chuhutin A, Pedersen L, Jensen JB, Jakobsen S, et al. Fast diffusion kurtosis imaging of fibrotic mouse kidneys. NMR Biomed. 2016; 29:1709–1719. PMID:
27731906.

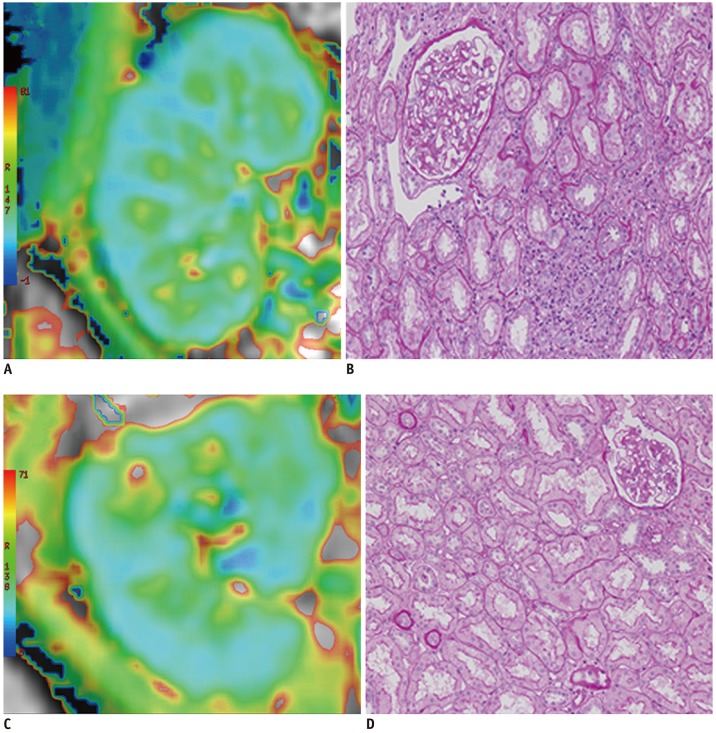
43. Liu Y, Zhang GM, Peng X, Wen Y, Ye W, Zheng K, et al. Diffusional kurtosis imaging in assessing renal function and pathology of IgA nephropathy: a preliminary clinical study. Clin Radiol. 2018; 73:818–826. PMID:
29929904.

44. Venkatachalam MA, Griffin KA, Lan R, Geng H, Saikumar P, Bidani AK. Acute kidney injury: a springboard for progression in chronic kidney disease. Am J Physiol Renal Physiol. 2010; 298:F1078–F1094. PMID:
20200097.

45. Li LP, Halter S, Prasad PV. Blood oxygen level-dependent MR imaging of the kidneys. Magn Reson Imaging Clin N Am. 2008; 16:613–625. PMID:
18926426.

46. Malvezzi P, Bricault I, Terrier N, Bayle F. Evaluation of intrarenal oxygenation by blood oxygen level-dependent magnetic resonance imaging in living kidney donors and their recipients: preliminary results. Transplant Proc. 2009; 41:641–644. PMID:
19328943.

47. Oostendorp M, de Vries EE, Slenter JM, Peutz-Kootstra CJ, Snoeijs MG, Post MJ, et al. MRI of renal oxygenation and function after normothermic ischemia-reperfusion injury. NMR Biomed. 2011; 24:194–200. PMID:
20954164.

48. Niles DJ, Artz NS, Djamali A, Sadowski EA, Grist TM, Fain SB. Longitudinal assessment of renal perfusion and oxygenation in transplant donor-recipient pairs using arterial spin labeling and blood oxygen level-dependent magnetic resonance imaging. Invest Radiol. 2016; 51:113–120. PMID:
26561047.

49. Sadowski EA, Fain SB, Alford SK, Korosec FR, Fine J, Muehrer R, et al. Assessment of acute renal transplant rejection with blood oxygen level-dependent MR imaging: initial experience. Radiology. 2005; 236:911–919. PMID:
16118170.

50. Han F, Xiao W, Xu Y, Wu J, Wang Q, Wang H, et al. The significance of BOLD MRI in differentiation between renal transplant rejection and acute tubular necrosis. Nephrol Dial Transplant. 2008; 23:2666–2672. PMID:
18308769.

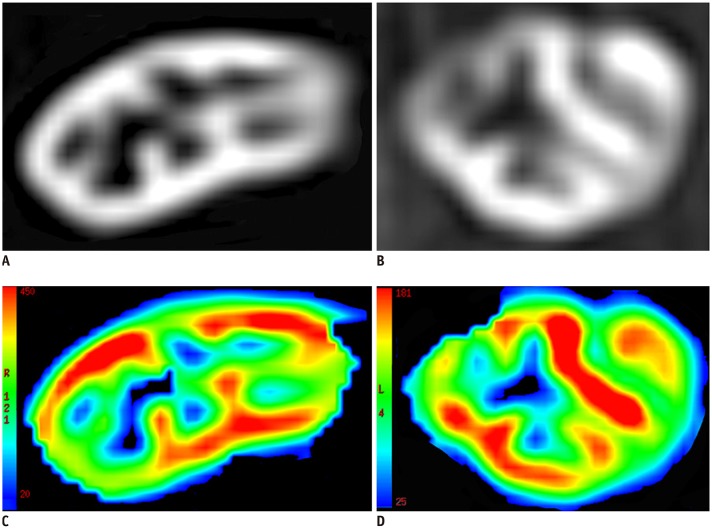
51. Park SY, Kim CK, Park BK, Huh W, Kim SJ, Kim B. Evaluation of transplanted kidneys using blood oxygenation level-dependent MRI at 3 T: a preliminary study. AJR Am J Roentgenol. 2012; 198:1108–1114. PMID:
22528900.

52. Park SY, Kim CK, Park BK, Kim SJ, Lee S, Huh W. Assessment of early renal allograft dysfunction with blood oxygenation level-dependent MRI and diffusion-weighted imaging. Eur J Radiol. 2014; 83:2114–2121. PMID:
25452096.

53. Djamali A, Sadowski EA, Muehrer RJ, Reese S, Smavatkul C, Vidyasagar A, et al. BOLD-MRI assessment of intrarenal oxygenation and oxidative stress in patients with chronic kidney allograft dysfunction. Am J Physiol Renal Physiol. 2007; 292:F513–F522. PMID:
17062846.

54. Seif M, Eisenberger U, Binser T, Thoeny HC, Krauer F, Rusch A, et al. Renal blood oxygenation level-dependent imaging in longitudinal follow-up of donated and remaining kidneys. Radiology. 2016; 279:795–804. PMID:
26744926.

55. Kuo PH, Kanal E, Abu-Alfa AK, Cowper SE. Gadolinium-based MR contrast agents and nephrogenic systemic fibrosis. Radiology. 2007; 242:647–649. PMID:
17213364.

56. Guo BJ, Yang ZL, Zhang LJ. Gadolinium deposition in brain: current scientific evidence and future perspectives. Front Mol Neurosci. 2018; 11:335. PMID:
30294259.

57. Boyken J, Niendorf T, Flemming B, Seeliger E. Gadolinium deposition in the brain after contrast-enhanced MRI: are the data valid. Radiology. 2018; 288:630–632. PMID:
29916783.
58. Ho ML. Arterial spin labeling: clinical applications. J Neuroradiol. 2018; 45:276–289. PMID:
30016705.

59. Havsteen I, Damm Nybing J, Christensen H, Christensen AF. Arterial spin labeling: a technical overview. Acta Radiol. 2018; 59:1232–1238. PMID:
29313361.

60. Sadowski EA, Djamali A, Wentland AL, Muehrer R, Becker BN, Grist TM, et al. Blood oxygen level-dependent and perfusion magnetic resonance imaging: detecting differences in oxygen bioavailability and blood flow in transplanted kidneys. Magn Reson Imaging. 2010; 28:56–64. PMID:
19577402.

61. Lanzman RS, Wittsack HJ, Martirosian P, Zgoura P, Bilk P, Kröpil P, et al. Quantification of renal allograft perfusion using arterial spin labeling MRI: initial results. Eur Radiol. 2010; 20:1485–1491. PMID:
19949799.

62. Artz NS, Sadowski EA, Wentland AL, Djamali A, Grist TM, Seo S, et al. Reproducibility of renal perfusion MR imaging in native and transplanted kidneys using non-contrast arterial spin labeling. J Magn Reson Imaging. 2011; 33:1414–1421. PMID:
21591011.

63. Artz NS, Sadowski EA, Wentland AL, Grist TM, Seo S, Djamali A, et al. Arterial spin labeling MRI for assessment of perfusion in native and transplanted kidneys. Magn Reson Imaging. 2011; 29:74–82. PMID:
20850241.

64. Heusch P, Wittsack HJ, Blondin D, Ljimani A, Nguyen-Quang M, Martirosian P, et al. Functional evaluation of transplanted kidneys using arterial spin labeling MRI. J Magn Reson Imaging. 2014; 40:84–89. PMID:
24123319.

65. Hueper K, Gueler F, Bräsen JH, Gutberlet M, Jang MS, Lehner F, et al. Functional MRI detects perfusion impairment in renal allografts with delayed graft function. Am J Physiol Renal Physiol. 2015; 308:F1444–F1451. PMID:
25925250.

66. Hueper K, Schmidbauer M, Thorenz A, Bräsen JH, Gutberlet M, Mengel M, et al. Longitudinal evaluation of perfusion changes in acute and chronic renal allograft rejection using arterial spin labeling in translational mouse models. J Magn Reson Imaging. 2017; 46:1664–1672. PMID:
28342287.

67. Heusch P, Wittsack HJ, Heusner T, Buchbender C, Quang MN, Martirosian P, et al. Correlation of biexponential diffusion parameters with arterial spin-labeling perfusion MRI: results in transplanted kidneys. Invest Radiol. 2013; 48:140–144. PMID:
23249648.
68. Ren T, Wen CL, Chen LH, Xie SS, Cheng Y, Fu YX, et al. Evaluation of renal allografts function early after transplantation using intravoxel incoherent motion and arterial spin labeling MRI. Magn Reson Imaging. 2016; 34:908–914. PMID:
27114341.

69. Strupler M, Hernest M, Fligny C, Martin JL, Tharaux PL, Schanne-Klein MC. Second harmonic microscopy to quantify renal interstitial fibrosis and arterial remodeling. J Biomed Opt. 2008; 13:054041. PMID:
19021421.

70. Park WD, Griffin MD, Cornell LD, Cosio FG, Stegall MD. Fibrosis with inflammation at one year predicts transplant functional decline. J Am Soc Nephrol. 2010; 21:1987–1997. PMID:
20813870.

71. Costa JS, Alves R, Sousa V, Marinho C, Romaozinho C, Santos L, et al. Fibrogenesis in kidney transplant: dysfunction progress biomarkers. Transplant Proc. 2017; 49:787–791. PMID:
28457395.

72. Yin M, Kolipaka A, Woodrum DA, Glaser KJ, Romano AJ, Manduca A, et al. Hepatic and splenic stiffness augmentation assessed with MR elastography in an in vivo porcine portal hypertension model. J Magn Reson Imaging. 2013; 38:809–815. PMID:
23418135.

73. Jiang X, Asbach P, Streitberger KJ, Thomas A, Hamm B, Braun J, et al. In vivo high-resolution magnetic resonance elastography of the uterine corpus and cervix. Eur Radiol. 2014; 24:3025–3033. PMID:
25038856.

74. Dittmann F, Hirsch S, Tzschätzsch H, Guo J, Braun J, Sack I. In vivo wideband multifrequency MR elastography of the human brain and liver. Magn Reson Med. 2016; 76:1116–1126. PMID:
26485494.

75. Hiscox LV, Johnson CL, Barnhill E, McGarry MD, Huston J, van Beek EJ, et al. Magnetic resonance elastography (MRE) of the human brain: technique, findings and clinical applications. Phys Med Biol. 2016; 61:R401–R437. PMID:
27845941.

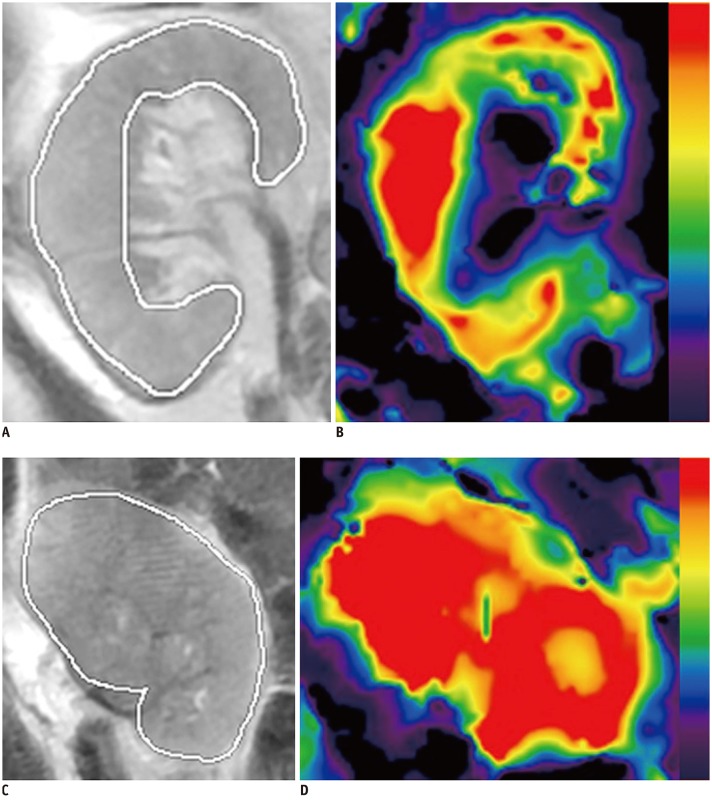
76. Lee CU, Glockner JF, Glaser KJ, Yin M, Chen J, Kawashima A, et al. MR elastography in renal transplant patients and correlation with renal allograft biopsy: a feasibility study. Acad Radiol. 2012; 19:834–841. PMID:
22503893.
77. Marticorena Garcia SR, Fischer T, Dürr M, Gültekin E, Braun J, Sack I, et al. Multifrequency magnetic resonance elastography for the assessment of renal allograft function. Invest Radiol. 2016; 51:591–595. PMID:
27504796.

78. Kirpalani A, Hashim E, Leung G, Kim JK, Krizova A, Jothy S, et al. Magnetic resonance elastography to assess fibrosis in kidney allografts. Clin J Am Soc Nephrol. 2017; 12:1671–1679. PMID:
28855238.

79. Martens MH, Lambregts DM, Papanikolaou N, Heijnen LA, Riedl RG, zur Hausen A, et al. Magnetization transfer ratio: a potential biomarker for the assessment of postradiation fibrosis in patients with rectal cancer. Invest Radiol. 2014; 49:29–34. PMID:
24002079.
80. Kline TL, Irazabal MV, Ebrahimi B, Hopp K, Udoji KN, Warner JD, et al. Utilizing magnetization transfer imaging to investigate tissue remodeling in a murine model of autosomal dominant polycystic kidney disease. Magn Reson Med. 2016; 75:1466–1473. PMID:
25974140.

81. Wang F, Jiang R, Takahashi K, Gore J, Harris RC, Takahashi T, et al. Longitudinal assessment of mouse renal injury using high-resolution anatomic and magnetization transfer MR imaging. Magn Reson Imaging. 2014; 32:1125–1132. PMID:
25093632.

82. Jiang K, Ferguson CM, Ebrahimi B, Tang H, Kline TL, Burningham TA, et al. Noninvasive assessment of renal fibrosis with magnetization transfer MR imaging: validation and evaluation in murine renal artery stenosis. Radiology. 2017; 283:77–86. PMID:
27697008.

83. Jiang K, Ferguson CM, Woollard JR, Zhu X, Lerman LO. Magnetization transfer magnetic resonance imaging noninvasively detects renal fibrosis in swine atherosclerotic renal artery stenosis at 3.0 T. Invest Radiol. 2017; 52:686–692. PMID:
28542095.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download