This article has been
cited by other articles in ScienceCentral.
Abstract
When a patient shows severe crowding, premolar extraction should be considered to provide required available space for alignment. If the third molars have already erupted and demonstrate a poor prognosis, third molar extraction and distalization of the posterior dentition can be used instead of premolar extraction to obtain space. Interproximal stripping (IPS) may also be used to gain space in cases of crowding. This case report describes the treatment of a 25-year-old man with severe crowding and mild lip protrusion. Although the crowding in the lower arch was severe enough to require first premolar extraction, distalization of the entire lower dentition with orthodontic mini-implants, extraction of the lower third molars, and IPS could successfully resolve the crowding and lip protrusion.
Keywords: Interproximal stripping, Orthodontic mini-implant, Distalization
INTRODUCTION
When a patient with malocclusion has a moderate or severe degree of crowding and a protrusive profile, premolar extraction is usually considered. Although extractions have long been used in orthodontic treatment, the decision to extract is still the most important and difficult one when planning treatment.
1 Premolar extractions can provide available space for the relief of crowding or for improving the lip profile.
23 Proffit et al.
4 mentioned that extraction is almost always required for patients with more than 10 mm of crowding; however, molar extraction is far less effective than first premolar extraction in the relief of crowding.
Interproximal stripping (IPS) is a common procedure used in orthodontics to gain space,
5 treat tooth-size discrepancies,
6 or reduce black triangle.
7 Distal retraction of the entire dentition by using orthodontic mini-implants (OMIs) has recently been introduced.
89 Moreover, current research has shown that if OMI and IPS are used together, their space-gaining effect can be synergistic because all the space created by IPS can be used to relieve crowding and improve the lip profile; it may also be a substitute for second premolar extraction.
10
When a patient with malocclusion has a missing or hopeless tooth other than a premolar, that space may be used as a treatment option instead of premolar extraction. Since the number of adult orthodontic patients has been increasing,
1112 the number of patients presenting with these circumstances seems to have been increasing as well. Because OMI can provide anchorage in any direction, the location of the available space is no longer a difficult issue to overcome.
This case report describes the treatment of severe crowding with lip protrusion by using OMIs and IPS. Upper first molar and lower third molar extractions could successfully resolve a severe arch length discrepancy and protrusive profile.
DIAGNOSIS AND ETIOLOGY
A healthy 25-year-old man sought orthodontic consultation for severe crowding (arch length discrepancy of the upper/lower arch = 9.0/11.5 mm) with a Class II profile and lip incompetency (
Figure 1). His chief complaint was anterior crowding and a retrusive chin. His upper right first molar had been extracted about 10 years ago because of severe caries, and the extracted space had almost closed because of the migration of the adjacent teeth. Panoramic radiography revealed an abnormal shape of his condyle, but he did not have any symptoms of temporomandibular joint disorder. The distal root of the lower left first molar appeared short, but there was no mobility or other symptoms. The patient had undergone pulpotomy in the upper left first molar when he was a high school student, and an oral examination revealed distal proximal caries at the margin of the prosthetic crown. His lower third molars also had caries; when he had visited a local dental clinic, the general dentist had recommended endodontic treatment for the lower third molars. Generalized gingival recession was also observed. Overbite and overjet were both shallow (1.0 and 2.0 mm, respectively).
The upper dental midline was shifted to the right side, while the lower dental midline was shifted slightly to the left. The molar relationship of the patient's right side was Class III, while that of the left side was Class II.
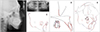
Cephalometric analysis (
Table 1) revealed a protrusive maxilla (A to N perpendicular, 4.2 mm), retrusive mandible (Pog to N perpendicular, −9.5 mm), and vertical skeletal pattern (Bjork sum, 402.6°). A frontal cephalometric radiograph (
Figure 2) showed mild mandibular asymmetry that was not obvious in facial photographs. The midline shift of his lower dentition seemed to be caused by an asymmetric mandible. He did not have any unusual medical or dental history.
TREATMENT OBJECTIVES
The treatment objectives were to resolve the crowding, obtain a Class I canine and molar relationship with a normal overbite and overjet, and improve the facial profile.
TREATMENT ALTERNATIVES
Because of the severe crowding, first premolar extraction was the first option. In the lower arch, the amount of crowding was very severe; even first premolar extraction could not provide enough space to resolve the crowding and improve the profile. OMIs were needed in the lower arch to reinforce the anchorage.
Severe caries was observed on the lower third molars, for which endodontic treatment was required. Pulpotomy had been performed on the upper left first molar several years ago, and a secondary root caries was found on the distal proximal surface. To treat this caries, a crown remake was necessary at minimum; a possible root canal was also considered necessary.
For these reasons, extraction of the lower third molars and upper left first molar was the second option. On the upper right side, second molar distalization and IPS were needed to relieve crowding because the extraction space was almost closed. A large amount of molar distalization was required in the lower arch because of the severe crowding. Additionally, IPS of the lower dentition was planned to gain more space.
After a discussion with the patient, extraction of the upper left first molar and lower third molars was chosen as the treatment modality. A large amount of space was needed on the upper left side to correct the midline, relieve the crowding, and improve the profile. On the upper right side, IPS and a small amount of molar distalization were likely adequate for tooth alignment and incisor retraction. Therefore, OMIs were placed in the upper right, lower right, and lower left buccal alveolar bone. The possibility of additional OMI placement in the upper left side was also discussed with the patient.
TREATMENT PROGRESS
After the extraction of the lower third molars and upper left first molar, 0.022-inch (in) preadjusted edgewise brackets (Clarity and Victory; 3M Unitek, Monrovia, CA, USA) were placed on the buccal surface of the lower teeth (except for the second premolars). With the help of IPS, the archwire sequence progressed from a 0.014-in nickel titanium wire to a 0.018-in stainless steel wire. OMIs (Mplant U2; BioMaterials Korea Inc., Seoul, Korea) were placed on the buccal side between the second premolar and second molar in the upper arch, as well as between the first and second molars in the lower arch. The buccal shelf area was used in the lower arch because the amount of distalization had to be larger than the interradicular space in this area.
1013 The lower archwire bypassed the second premolar until sufficient space had been acquired using IPS and molar distalization (
Figure 3). Brackets were also placed on the lingual surface of the lower second molar and first premolar to facilitate faster space gaining. The upper right second molar was uprighted and distalized using an OMI.
IPS was performed as follows. A rubber separation ring was placed for 1 week before IPS. After the removal of the separation ring, a diamond-coated stripping disk (Superflex 355-514-160; Edenta, Austenau, Austria) was used to remove the proximal enamel at the contact point. Thereafter, cone-shaped diamond burs (Komet 8833; Brasseler, Lemgo, Germany) were used for rounding the corners. The final polishing was done using Sof-Lex discs (3M, Saint Paul, MN, USA). Topical fluoride treatment was applied after the IPS procedure. In the area with severe crowding, IPS was postponed until the crowding had almost resolved.
After leveling, 0.019 × 0.025-in stainless steel working wires were placed, and retraction of the whole dentition progressed. When the upper left first molar extraction space was about 1.5 mm in size, an OMI was added to the upper left side because the profile had not changed by that time.
During the finishing stage, the patient did not visit my office regularly and showed poor compliance in wearing the interarch elastics because of a busy schedule. The total active treatment period was 36 months. Before the removal of the fixed orthodontic appliance, a canine-to-canine fixed lingual retainer was placed. After bracket removal, an upper circumferential retainer and lower Hawley retainer were given to the patient.
TREATMENT RESULTS
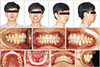
Posttreatment records (
Figure 4) indicated that the severe crowding was successfully resolved, and the patient's profile was improved. The first molar extraction space was successfully closed, and the midline deviation was corrected. Cephalometric tracing and measurements showed the retraction of the incisors and improvement of the lip profile (
Figure 5 and
Table 1). When the amount of lower molar distalization was assessed using a mesiobuccal cusp tip and the initial occlusal plane, it averaged about 4.9 mm in size.
Twenty months after debonding, the patient returned for a checkup. He did not show any noticeable changes in occlusion or profile (
Figure 6). In the cephalometric superimposition (
Figure 7), the profile of the patient remained stable except for reduced upper lip thickness.
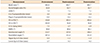
Model analysis was performed using digital calipers. All the teeth and arch dimensions were measured twice, and the average of these measurements was used. The amount of treatment change of intercanine width was small (
Table 2). Maxillary intermolar width decreased by 1.22 mm, while mandibular intermolar width increased by 0.17 mm during treatment. The amount of IPS was calculated as the difference in pretreatment and post-treatment tooth width measurements. The total amount of IPS in the upper and lower dentitions was 3.61 mm and 6.34 mm, respectively (
Table 3).
DISCUSSION
The lower third molars and upper first molars were extracted in this patient because of caries. According to conventional mechanics, additional premolar extractions would be required to correct the severe crowding and improve the patient's profile. However, OMIs could provide sufficient anchorage and overcome the problem of the position of the available space.
IPS can be used to provide a small amount of space to alleviate crowding,
14 correct interarch tooth-size discrepancy, and reduce the issue of black triangles.
15 If IPS and molar distalization using OMIs are used together, their space-gaining effect can be synergistic because all the space created by IPS can be used where it is needed without anchorage loss.
10 This case illustrated that such a synergistic effect could solve very severe crowding and lip protrusion problems, and the retention record indicated that the result was stable over time.
This impressive treatment result is largely because of the third molar extraction space. If the patient's third molar was fully impacted, or only a small portion was erupted, third molar extraction could not provide sufficient available space; hence, the utility of this treatment strategy would be limited.
Many different opinions exist about the optimal amount of IPS, but the viewpoint that is supported by most is a reduction of the proximal enamel by 50%.
1617 If we consider the average thickness of the proximal enamel,
1819 the recommended reduction maximums are 0.3 to 0.4 mm for the upper incisors, 0.2 mm for the lower incisors, 0.4 to 0.5 mm for the canines, 0.5 mm for the premolars, and 0.6 mm for the molars. If IPS is performed from the first molar to the opposite first molar, the maximum space gained through IPS would be 10.4 mm in the upper arch (0.3 × 4 + 0.4 × 2 + 0.5 × 4 + 0.6 × 2 = 5.2 mm per side) and 9.6 mm in the lower arch (0.2 × 4 + 0.4 × 2 + 0.5 × 4 + 0.6 × 2 = 4.8 mm per side). Because it is very difficult to remove exactly 50%, a smaller reduction is recommended because it is safer and easier. To ensure maximum space gaining and reduce the risk of over-reduction, IPS in the molar region is needed; however, it requires extensive experience and skill. The amount of IPS achieved in the lower arch of this patient was about 60% of the recommended maximum.
Obtaining the exact amount of space is another difficulty often encountered during IPS. Although some measuring gauges for IPS are available on the market, the measurements obtained using these are not precise. A previous study using a laser scanner showed a variation in the amount of IPS regardless of the method used.
20 Therefore, obtaining a smaller space might be better than trying to achieve the maximum amount of space possible to minimize any side effects. Gradual removal of the proximal enamel and measurement of the amount of enamel between the processes are also recommended.
The amount of crowding in the lower arch was 11.5 mm in this patient, and some degree of incisor retraction was also needed. If all the required space had been gained by molar distalization, more than 6 mm would have been needed. However, some patients do not have enough available space in the posterior region; even if there is sufficient space, such a large amount of distalization often requires too much time. In contrast, if all the required space is gained using IPS, there may be a risk of lamellae or enamel tuft exposure
21 due to excessive enamel reduction, and part of the gained space could be lost because of anchorage loss when conventional mechanics are used. Therefore, molar distalization or IPS alone without premolar extraction is not a good option to treat severe crowding in many cases. Previous research has shown that 3.6 to 3.8 mm of crowding can be resolved through 2.1 to 2.2 mm of molar distalization in conjunction with IPS. This also allows for around 3.2 to 3.8 mm of incisor retraction.
10
Many previous studies have dealt with whole-arch distalization by using buccal alveolar OMIs.
82223 When OMIs are placed in the buccal alveolar bone, the amount of molar distalization is limited because of the small interradicular space. When a large amount of distalization is needed, other places like the palate,
24 zygomatic buttress,
25 mandibular ramus,
26 or buccal shelf
27 can be used. These areas do not carry the risk of root contact, and hence, a larger amount of molar distalization than that achieved using the buccal alveolar bone is possible. In this patient, 4.7 mm of lower molar distalization was achieved using buccal-shelf OMIs.
CONCLUSION
A patient with very severe crowding can be treated with molar distalization and IPS. If sufficient posterior space is available for molar distalization, OMI and IPS can be good substitutes for first premolar extraction in cases of severe crowding.
Figures and Tables
Figure 1
Pretreatment facial and intraoral photographs.

Figure 2
Pretreatment radiographs and tracing. The numbers in the tracing indicate FDI tooth number.

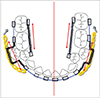
Figure 3
Schematics of space gaining in the lower arch. Bracket bonding on the lower second premolars was postponed until sufficient space was obtained using interproximal stripping and molar distalization. Double sided arrows indicate the pushing force of the spring.
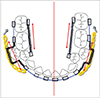
Figure 4
Posttreatment facial and intraoral photographs.
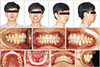
Figure 5
Posttreatment radiographs.

Figure 6
Facial and intraoral photographs acquired 20 months after debonding.

Figure 7
Radiographs (A, B) acquired 20 months after debonding and superimposition tracing (C–E); pretreatment (black), posttreatment (red), and retention (blue) lateral cephalograms. C, mandibular superimposition; D, maxillary superimposition; E, cranial base superimposition. The numbers in D and E indicate FDI tooth number.
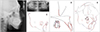
Table 1
Changes in cephalometric measurements
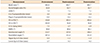
Table 2
Changes in intercanine width and intermolar width during treatment

Table 3
Measurements of tooth width and amount of interproximal stripping (IPS) (mm)






 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download