This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Fracture–dislocation of the proximal interphalangeal (PIP) joint of the finger is challenging due to the high risk of stiffness. The purpose of this study is to evaluate the clinical and radiological results of a modified transosseous wiring technique for the management of chronic fracture–dislocations of the PIP joint.
Methods
Ten patients (nine men and one woman; mean age, 38.3 years; range, 21 to 69 years) with neglected fracture–dislocation of the PIP joint were included. The mean duration from injury to operation was 14.7 weeks (range, 3 to 66 weeks). The dorsolateral approach and extension block pinning were used to reduce dislocation. After thorough debridement of the scar tissues in the dorsal dead space and the fracture site, the reduction was maintained with transosseous wiring. Radiologic evaluations of bone union and arthritic changes and clinical evaluations (range of motion of the PIP joint and Disabilities of the Arm, Shoulder and Hand [DASH] score) were performed. The mean follow-up period was 12.9 months (range, 12 to 19 months).
Results
All patients demonstrated evidence of radiographic healing within a mean healing time of 6 weeks (range, 4 to 10 weeks); however, one had a widened gap and one had an early arthritic change. The mean range of motion in the PIP joint was 81° (range, 50° to 105°). The mean DASH score was 21.6 (range, 7.5 to 35.8).
Conclusions
For chronic fracture–dislocation of the PIP joint, transosseous wiring with direct curettage and optimal bone purchase can provide satisfying outcome.
Go to :

Keywords: Fracture dislocation, Proximal interphalangeal joint, Bone wires, Extension block
Fracture–dislocation of the proximal interphalangeal (PIP) joint is a common yet challenging hand injury;
1) the fracture fragments are very small, making fixation difficult.
2) Several treatment options for acute fracture–dislocation have been introduced. Conservative treatment includes immobilization using an extension blocking splint or buddy taping and surgical fixation using a Kirschner wire,
3) dynamic external fixators,
45) mini cannulated screws,
6) or a miniplate,
7) with no treatment being superior to the others. Treatment becomes significantly more difficult when the soft tissues, which usually start to heal in 7 to 10 days after the injury, obstruct fracture reduction.
8) Therefore, fracture–dislocation of the PIP joint is often neglected, and patients would present with such conditions at a later stage in outpatient clinics. In chronic or neglected cases, the treatment is more challenging due to joint stiffness and partial union or malunion. Although some authors reported success with open reduction and internal fixation
9) or the use of a dynamic external fixator,
1) it is not uncommon for surgeons to resort to salvage surgery such as arthroplasty,
1011) arthrodesis,
12) or joint transplantation.
13)
Yabe
14) demonstrated the surgical technique of transosseous wire fixation for late-presenting fracture–dislocation of the PIP joint. We modified the transosseous wiring method by combining it with prior extension block pinning. This combination approach allows for better removal of the fibrous tissue surrounding the old fracture site with the fracture site open, and it is cost-effective because it does not require an expensive implant. Therefore, the purpose of this study is to introduce the modified transosseous wiring technique and evaluate clinical and radiologic outcomes of the technique for the management of chronic fracture–dislocation of the PIP joint.
METHODS
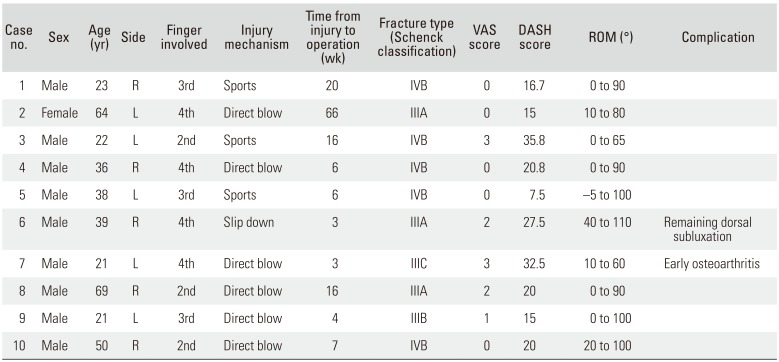
After receiving approval of Kyungpook National University Hospital Institutional Review Board (IRB No. 2016-11-013), which waived the informed consents from the patients, we retrospectively reviewed the records of 10 consecutive patients who underwent surgical treatment with transosseous wiring for neglected fracture–dislocation of the PIP joint between April 2003 and October 2013. We considered fracture–dislocation was neglected when the patient presented at least 3 weeks after the initial injury. There were nine men and one woman with a mean age of 38.3 years (range, 21 to 69 years). The mean time from injury to operation was 14.7 weeks (range, 3 to 66 weeks). Other demographic data are shown in
Table 1. All cases involved dorsal dislocation.
Table 1
Patient Demographics
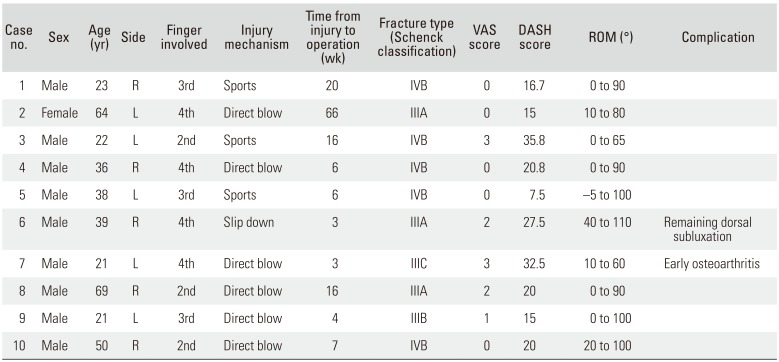
|
Case no. |
Sex |
Age (yr) |
Side |
Finger involved |
Injury mechanism |
Time from injury to operation (wk) |
Fracture type (Schenck classification) |
VAS score |
DASH score |
ROM (°) |
Complication |
|
1 |
Male |
23 |
R |
3rd |
Sports |
20 |
IVB |
0 |
16.7 |
0 to 90 |
|
|
2 |
Female |
64 |
L |
4th |
Direct blow |
66 |
IIIA |
0 |
15 |
10 to 80 |
|
|
3 |
Male |
22 |
L |
2nd |
Sports |
16 |
IVB |
3 |
35.8 |
0 to 65 |
|
|
4 |
Male |
36 |
R |
4th |
Direct blow |
6 |
IVB |
0 |
20.8 |
0 to 90 |
|
|
5 |
Male |
38 |
L |
3rd |
Sports |
6 |
IVB |
0 |
7.5 |
−5 to 100 |
|
|
6 |
Male |
39 |
R |
4th |
Slip down |
3 |
IIIA |
2 |
27.5 |
40 to 110 |
Remaining dorsal subluxation |
|
7 |
Male |
21 |
L |
4th |
Direct blow |
3 |
IIIC |
3 |
32.5 |
10 to 60 |
Early osteoarthritis |
|
8 |
Male |
69 |
R |
2nd |
Direct blow |
16 |
IIIA |
2 |
20 |
0 to 90 |
|
|
9 |
Male |
21 |
L |
3rd |
Direct blow |
4 |
IIIB |
1 |
15 |
0 to 100 |
|
|
10 |
Male |
50 |
R |
2nd |
Direct blow |
7 |
IVB |
0 |
20 |
20 to 100 |
|

We excluded any patients with an open fracture or neurovascular injury. Patients with fixed arthritic changes were also excluded. Each fracture was classified according to Schenck classification,
15) which considers both the articular side involvement and the degree of dorsal dislocation. Fracture grade was categorized as type I when the fracture was less than 10% of the surface, type II when it was 11%–20%, type III when it was 21%–40%, and type IV when it was greater than 40%. Dorsal dislocation was classified as grade A when it was less than 25%, grade B when it was 25%–50%, grade C when it was greater than 50%, and grade D when it was full.
Surgical Technique
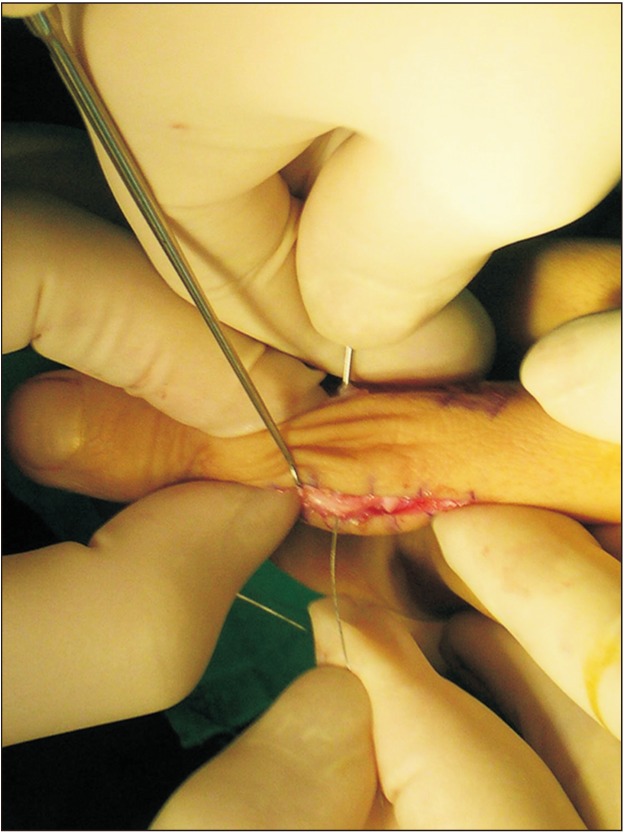
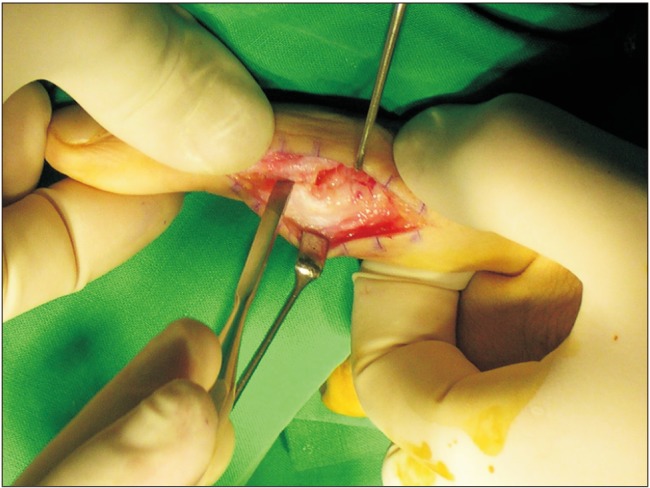
Dorsolateral skin incisions around the PIP joint were used. The extensor hood was retracted from the lateral to the medial side of the PIP joint to expose the fracture site. The extensor hood was incised as necessary. The dorsal capsule was usually hypertrophied and dorsal dislocation of the middle phalanx was observed. The hypertrophied tissue of the dorsal space was debrided. If exposure was not sufficient, we added dorsomedial approach. The volar plate and the collateral ligament were typically intact. The fibrotic tissue between the fracture fragments was thoroughly removed using a rongeur and a curette (
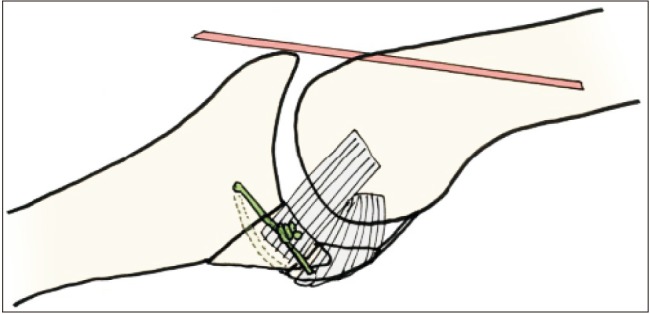
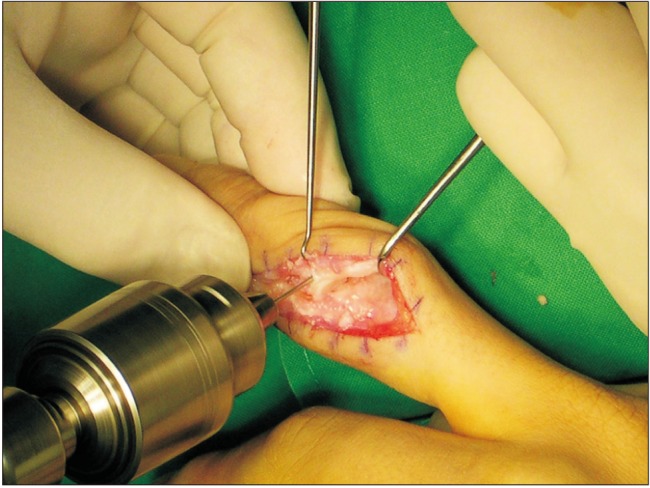
Fig. 1). When the fracture was malunited, an osteotome was used to separate the fragments (
Fig. 2). To correct the dorsal subluxation of the middle phalanx, a 1.1-mm Kirschner wire was inserted into the proximal phalanx head as an extension block in all patients except two, who underwent surgery in the relatively early period. After reduction of the dislocation, a lateral view was obtained by fluoroscopy. A bone tunnel for the metal wires parallel to the joint surface was made by drilling a 0.9-mm Kirschner wire into the base of the proximal phalanx (
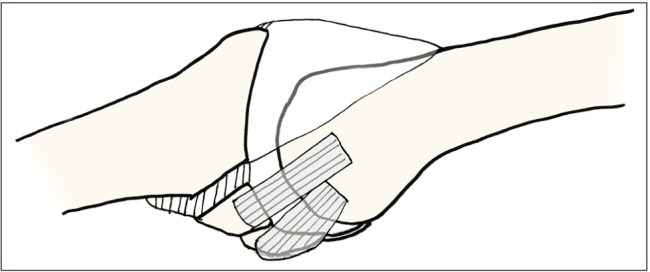
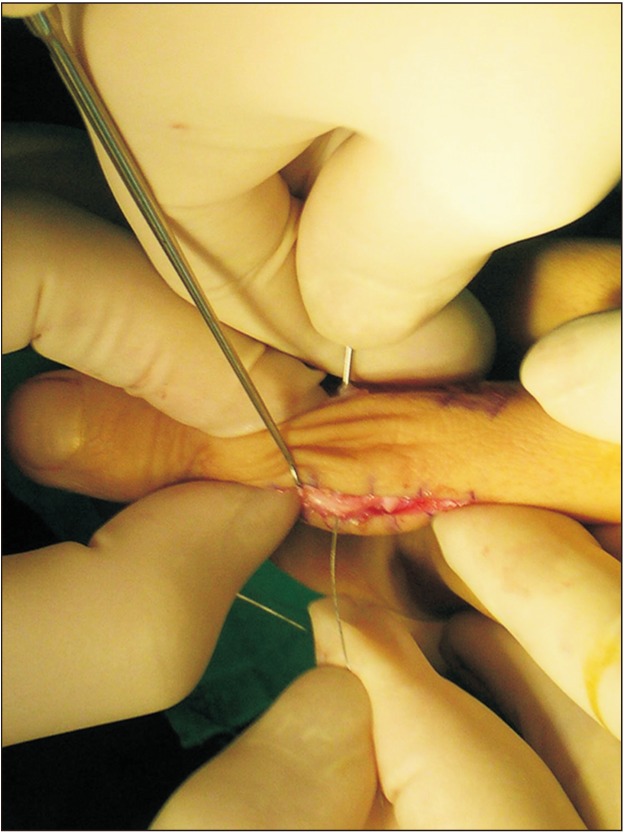
Fig. 3). The volar fracture fragment was reduced using a small periosteum elevator or forceps. A 25-gauge wire was passed through the bone tunnel in the proximal phalangeal base (
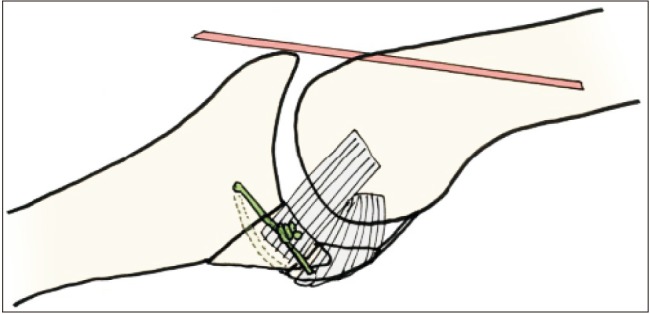
Fig. 4) and tightened and twisted to ensure that it purchased the anterior part of the volar small fragment. The volar plate can be punctured; however, the volar fragment itself should not be punctured by the wire to avoid further damage (
Fig. 5). If the fragment was large enough, two transosseous wires were used. The reduction status was checked using fluoroscopy. After range of motion (ROM) of the PIP joint was ensured, the soft tissue envelope was repaired in a layered fashion.
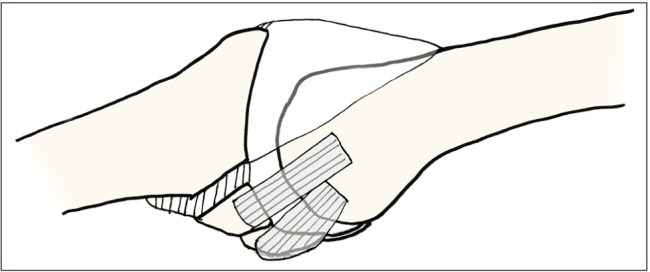 | Fig. 1The drawing shows a dorsally dislocated fracture with scar tissue in the dorsal dead space and the malunited site. The scar tissues should be debrided in such cases.
|
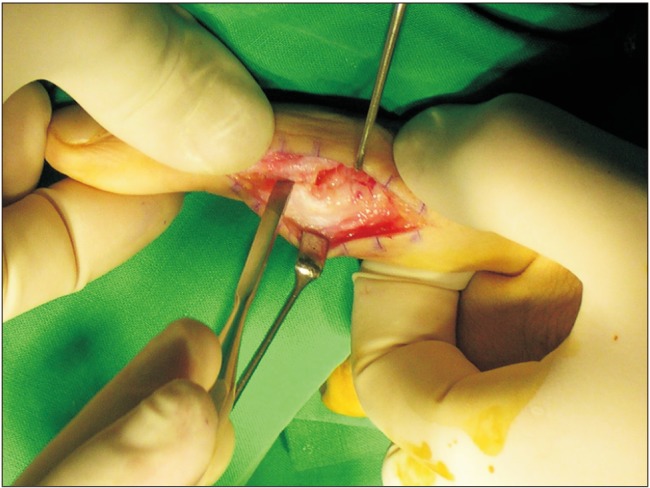 | Fig. 2Intraoperative photograph of a 36-year-old male patient. The fracture site was exposed through the dorsolateral incision. The malunited fracture was osteotomized by using an osteotome. The collateral ligament was intact from the volar fragment of the middle phalanx.
|
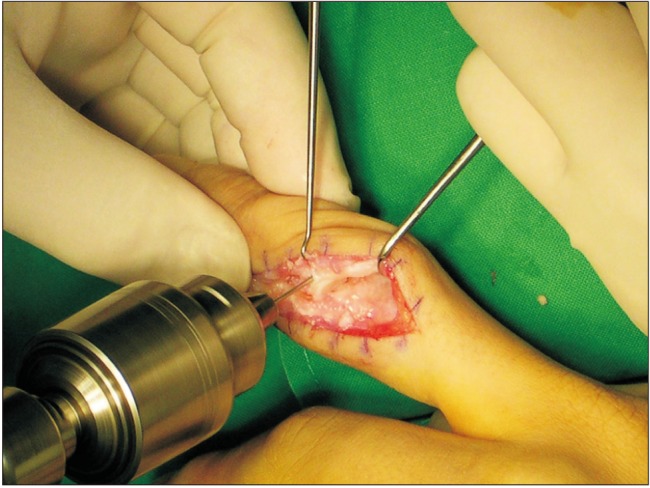 | Fig. 3After osteotomy of the malunited site, a bone tunnel was made in the dorsal fragment by drilling with a Kirschner wire.
|
 | Fig. 4The Kirschner wire was removed, and the inlet was occupied by a wire to pass the bone tunnel.
|
 | Fig. 5The wire that has passed the bone tunnel in the dorsal fragment was tightened and twisted to ensure that it purchased the anterior part of the volar small fragment. The volar plate can be punctured.
|
Postoperative Rehabilitation
Immediately after surgery, the finger was protected with a volar aluminum splint with the PIP joint in a neutral position, leaving the distal interphalangeal joint free. If the patient underwent an extension block with Kirschner wires, the wires were removed after a mean of 29 days (range, 24 to 35 days). Active ROM exercises were started immediately after removal of the extension block or 1 month after the operation.
Evaluations
Radiological evaluations were conducted using anteroposterior, lateral, and oblique views on simple radiographs. They were taken immediately after surgery, 2 weeks after surgery, and 1, 2, 6, and 12 months after surgery until bone union was achieved. Bone union and arthritic change of the PIP joints were investigated. Bone union was defined as bridging trabeculae and the absence of a radiolucent line at the fracture gap.
Clinical evaluations include measurement of active ROM of the PIP joint and pain by using visual analog scale (VAS) scores. ROM was measured using a goniometer by another surgeon who did not perform the surgery. Finally, Disabilities of the Arm, Shoulder and Hand (DASH) score at the final follow-up was measured in all patients.
Go to :

RESULTS
The mean follow-up period was 12.9 months (range, 12 to 19 months). All patients demonstrated evidence of radiographic healing within an average healing time of 6 weeks (range, 4 to 10 weeks) (
Fig. 6). However, in two cases of early loosening, the fractures healed with a widened fracture gap. Of these two patients, one showed dorsal subluxation at the final follow-up, while another patient showed an early arthritic change 1 month after surgery. Both patients refused further surgery due to the unsatisfactory results and fear of not achieving good results even after a second surgery.
 | Fig. 6(A) The lateral radiograph of a 21-year-old man who was injured by a direct blow 3 weeks before presentation shows a Schenck type IIIC fracture–dislocation of the third proximal interphalangeal joint. (B) The postoperative radiograph shows a fracture–dislocation that was reduced by transosseous wiring that purchased the volar fragment with an extension blocking Kirschner wire in the proximal phalanx. (C) One year after surgery, the wire was removed. The radiograph shows a normal joint space with bony union.
|
The mean ROM of the PIP joint was 81° (range, 50° to 105°). The mean VAS and DASH scores were 1.2 (range, 0 to 3) and 21.6 (range, 7.5 to 35.8), respectively. No cases of infection were observed. Due to implant irritation, one patient underwent removal of the transosseous wire under local anesthesia.
Go to :

DISCUSSION
Fracture–dislocation of the PIP joint is difficult to treat and often results in motion limitations, residual pain, and joint instability.
16) The treatment goals include restoration of a normal articular surface, normal ROM, and motion stability, joint reduction,
17) and clinical pain reduction.
13)
Although several treatment options such as extension block pinning,
18) closed reduction and pin fixation,
19) volar miniplate and screw fixation,
7) and dynamic traction
20) have demonstrated satisfactory results for acute fracture–dislocation of the PIP joint, few authors have reported good results for chronic fractures. Agee
2122) reported that the average arc of motion was greater in acute injuries than in chronic injuries (95° vs. 70°), and several complications were observed in acute cases. The postulated causes of such poor results were fibrotic tissues between the fracture fragments, hence poorer reduction. As with other malunion fractures, several factors require consideration in the management of chronic PIP fracture–dislocation. First, curettage of the fibrotic tissues in the malunited site must be performed thoroughly. Thus, for chronic and neglected fractures, open reduction is essential. In this study, the site was thoroughly cleaned until we confirmed new vascularization. Because exposure of the malunited site is important, we recommend both dorsomedial and dorsolateral approaches when the fracture site is not accessible in one direction. Ishida and Ikuta
9) also reported acceptable results in chronic cases after using open reduction and internal fixation.
Second, the fixation should be firm and accurate enough to enable early ROM exercises. Using the surgical technique described in this study, we achieved satisfactory results. Our technique was effective in restoration of normal anatomy as well as soft tissues. Reliable fixation provided by transosseous wiring was the key to the successful results. Based on our experience, we believe that transosseous wiring enables more secure bone purchase than cerclage wiring without associated slippage. Rehabilitation was started approximately 1 month after surgery, and there was no need to remove an implant. To ensure accurate reduction, removal of the fibrous tissues at the dorsal dead space is also needed. Further, subluxation should be corrected before fracture reduction as necessary.
However, not all patients obtained successful outcome. Accurate reduction of the joint surface and reasonable integrity of the chondral surfaces are essential to restoration of the joint and achievement of good results.
23) In our study, one patient with a relatively longer duration (6 weeks) between the injury and the surgery had poorer outcomes according to the DASH score. We assumed that the early arthritic change in this patient was caused by the predamaged articular cartilage and the widened fracture gap. Regarding the wire loosening in two patients, we think this was due to the small number of wire twists, which resulted in an untied wire. A considerable number of wire twists is mandatory to avoid early loosening. Also, one patient with preoperative arthritic changes in the PIP joints (a 64-year-old woman) had poor ROM. When the articular cartilage is severely damaged at or before the time of injury, surgeons should consider other treatment options.
The limitations of this study include the small number of cases, retrospective design, and short follow-up for the assessment of the rate of degenerative change. Moreover, the results were not compared with those of other treatment methods in a similar patient cohort. Therefore, the validity of our findings should be further investigated in studies that include a larger number of patients and a longer observation period.
Fracture–dislocation of the PIP joint, especially the chronic one, remains a challenging condition in hand surgery. The modified transosseous wiring technique might be a clinically and radiologically reliable and cost-effective treatment alternative.
Go to :

ACKNOWLEDGEMENTS
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2017R1C1B5017140).
Go to :

Notes
Go to :

References
1. Shen XF, Mi JY, Rui YJ, et al. Delayed treatment of unstable proximal interphalangeal joint fracture-dislocations with a dynamic external fixator. Injury. 2015; 46(10):1938–1944. PMID:
26144906.

2. Weiss AP. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop Relat Res. 1996; (327):21–28. PMID:
8641066.
3. Tang JB, Avanessian B. New tendon, nerve, and bone surgical methods impacting the practice of hand surgery. Clin Plast Surg. 2014; 41(3):xix–xx. PMID:
24996477.

4. Ng CY, Oliver CW. Fractures of the proximal interphalangeal joints of the fingers. J Bone Joint Surg Br. 2009; 91(6):705–712. PMID:
19483220.

5. Finsen V. Suzuki's pins and rubber traction for fractures of the base of the middle phalanx. J Plast Surg Hand Surg. 2010; 44(4-5):209–213. PMID:
21446818.

6. Bhatt RA, Schmidt S, Stang F. Methods and pitfalls in treatment of fractures in the digits. Clin Plast Surg. 2014; 41(3):429–450. PMID:
24996463.

7. Cheah AE, Tan DM, Chong AK, Chew WY. Volar plating for unstable proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2012; 37(1):28–33. PMID:
22018477.

8. Freiberg A. Management of proximal interphalangeal joint injuries. Can J Plast Surg. 2007; 15(4):199–203. PMID:
19554177.

9. Ishida O, Ikuta Y. Results of treatment of chronic dorsal fracture-dislocations of the proximal interphalangeal joints of the fingers. J Hand Surg Br. 1998; 23(6):798–801. PMID:
9888686.

10. Criner KT, Ilyas AM. Silicone arthroplasty for chronic proximal interphalangeal joint dislocations. Tech Hand Up Extrem Surg. 2011; 15(4):209–214. PMID:
22105631.

11. Calfee RP, Kiefhaber TR, Sommerkamp TG, Stern PJ. Hemihamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2009; 34(7):1232–1241. PMID:
19700071.

12. Jones BF, Stern PJ. Interphalangeal joint arthrodesis. Hand Clin. 1994; 10(2):267–275. PMID:
8040205.

13. Hierner R, Berger AK. Long-term results after vascularised joint transfer for finger joint reconstruction. J Plast Reconstr Aesthet Surg. 2008; 61(11):1338–1346. PMID:
17996505.

14. Yabe Y. Open reduction for chronic PIP joint dorsal fracture dislocation. Seikei Geka. 1976; 27:1435–1439.
15. Schenck RR. Classification of fractures and dislocations of the proximal interphalangeal joint. Hand Clin. 1994; 10(2):179–185. PMID:
8040196.

16. Stern PJ, Roman RJ, Kiefhaber TR, McDonough JJ. Pilon fractures of the proximal interphalangeal joint. J Hand Surg Am. 1991; 16(5):844–850. PMID:
1940163.

17. Liodaki E, Xing SG, Mailaender P, Stang F. Management of difficult intra-articular fractures or fracture dislocations of the proximal interphalangeal joint. J Hand Surg Eur Vol. 2015; 40(1):16–23. PMID:
25427554.

18. de Haseth KB, Neuhaus V, Mudgal CS. Dorsal fracture-dislocations of the proximal interphalangeal joint: evaluation of closed reduction and percutaneous Kirschner wire pinning. Hand (N Y). 2015; 10(1):88–93. PMID:
25767425.
19. Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011; 36(9):1453–1459. PMID:
21820818.

20. Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008; 33(1):19–25. PMID:
18261660.

21. Agee JM. Unstable fracture dislocations of the proximal interphalangeal joint: treatment with the force couple splint. Clin Orthop Relat Res. 1987; (214):101–112. PMID:
3791731.
22. Agee JM. Unstable fracture dislocations of the proximal interphalangeal joint of the fingers: a preliminary report of a new treatment technique. J Hand Surg Am. 1978; 3(4):386–389. PMID:
681726.

23. Merrell G, Slade JF. Dislocations and ligament injuries in the digits. In : Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green's operative hand surgery. New York, NY: Churchill Livingstone;2005. p. 308.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download