1. Bentohami A, Bosma J, Akkersdijk GJ, van Dijkman B, Goslings JC, Schep NW. Incidence and characteristics of distal radial fractures in an urban population in The Netherlands. Eur J Trauma Emerg Surg. 2014; 40(3):357–361. PMID:
26816072.

2. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001; 26(5):908–915. PMID:
11561245.

3. Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011; 93(23):2146–2153. PMID:
22159849.

4. McQueen MM, Hajducka C, Court-Brown CM. Redis-placed unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 1996; 78(3):404–409. PMID:
8636175.
5. Fu YC, Chien SH, Huang PJ, et al. Use of an external fixation combined with the buttress-maintain pinning method in treating comminuted distal radius fractures in osteoporotic patients. J Trauma. 2006; 60(2):330–333. PMID:
16508491.

6. Herrera M, Chapman CB, Roh M, Strauch RJ, Rosenwasser MP. Treatment of unstable distal radius fractures with cancellous allograft and external fixation. J Hand Surg Am. 1999; 24(6):1269–1278. PMID:
10584952.

7. Rizzolo SJ, Schneider LH, Stewart WG Jr. Fractures of the shaft of the radius after treatment of Colles fractures with pins and plaster or external fixation. J Orthop Trauma. 1993; 7(1):78–83. PMID:
8433205.

8. Strohm PC, Muller CA, Boll T, Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures: a randomized trial. J Bone Joint Surg Am. 2004; 86(12):2621–2628. PMID:
15590845.
9. Chung KC, Squitieri L, Kim HM. Comparative outcomes study using the volar locking plating system for distal radius fractures in both young adults and adults older than 60 years. J Hand Surg Am. 2008; 33(6):809–819. PMID:
18656749.

10. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009; 91(8):1868–1873. PMID:
19651943.

11. Fanuele J, Koval KJ, Lurie J, Zhou W, Tosteson A, Ring D. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009; 91(6):1313–1319. PMID:
19487507.

12. Mattila VM, Huttunen TT, Sillanpaa P, Niemi S, Pihlajamaki H, Kannus P. Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland. J Trauma. 2011; 71(4):939–942. PMID:
21986738.

13. Wright TW, Horodyski M, Smith DW. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am. 2005; 30(2):289–299. PMID:
15781351.

14. Williksen JH, Husby T, Hellund JC, Kvernmo HD, Rosales C, Frihagen F. External fixation and adjuvant pins versus volar locking plate fixation in unstable distal radius fractures: a randomized, controlled study with a 5-year follow-up. J Hand Surg Am. 2015; 40(7):1333–1340. PMID:
25914018.
15. Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am. 2007; 89(9):2051–2062. PMID:
17768207.

16. Jupiter JB. Fractures of the distal end of the radius. J Bone Joint Surg Am. 1991; 73(3):461–469. PMID:
2002085.

17. McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function. J Bone Joint Surg Br. 1988; 70(4):649–651. PMID:
3403617.

18. Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000; (376):229–235.

19. Mann FA, Wilson AJ, Gilula LA. Radiographic evaluation of the wrist: what does the hand surgeon want to know? Radiology. 1992; 184(1):15–24. PMID:
1609073.

20. Steyers CM, Blair WF. Measuring ulnar variance: a comparison of techniques. J Hand Surg Am. 1989; 14(4):607–612. PMID:
2754190.

21. Matullo KS, Dennison DG. Outcome following distally locked volar plating for distal radius fractures with metadiaphyseal involvement. Hand (N Y). 2015; 10(2):292–296. PMID:
26034446.

22. Wagner M. General principles for the clinical use of the LCP. Injury. 2003; 34(Suppl 2):B31–B42. PMID:
14580984.

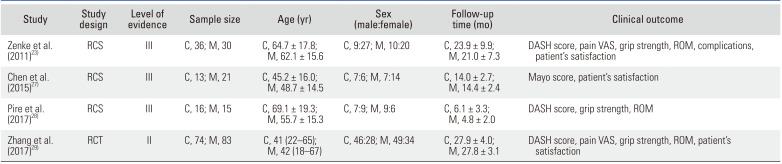
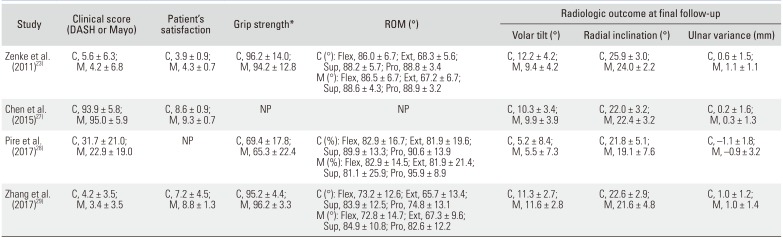
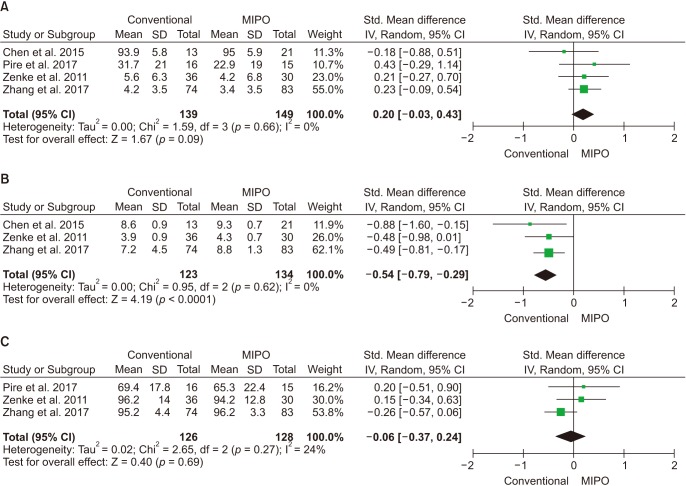
23. Zenke Y, Sakai A, Oshige T, et al. Clinical results of volar locking plate for distal radius fractures: conventional versus minimally invasive plate osteosynthesis. J Orthop Trauma. 2011; 25(7):425–431. PMID:
21464735.

24. Armangil M, Bezirgan U, Basarir K, Bilen G, Demirtas M, Bilgin SS. The pronator quadratus muscle after plating of distal radius fractures: is the muscle still working? Eur J Orthop Surg Traumatol. 2014; 24(3):335–339. PMID:
23435787.

25. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002; 84(8):1093–1110. PMID:
12463652.
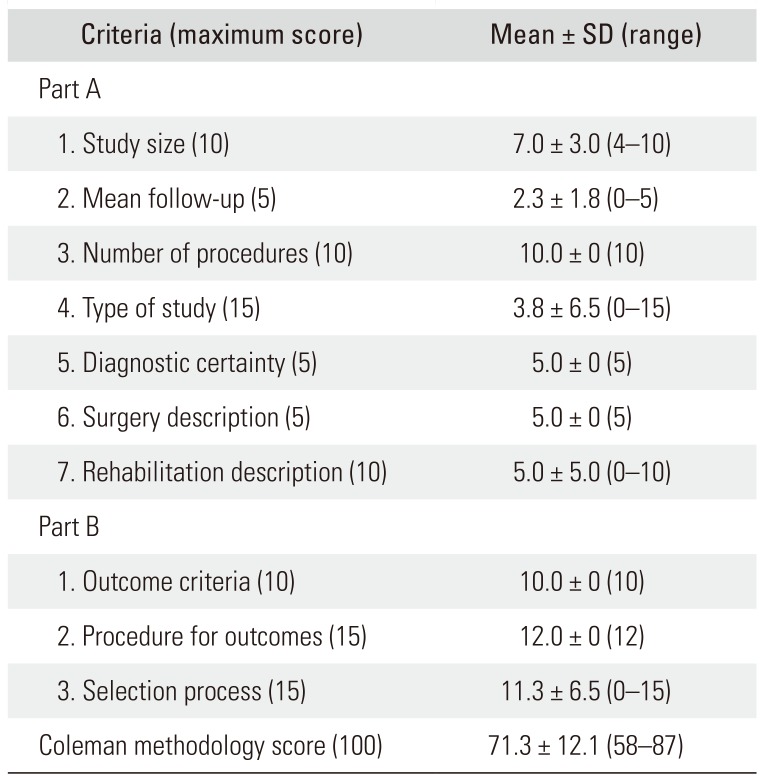
26. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000; 10(1):2–11. PMID:
10693606.
27. Chen CY, Lin KC, Yang SW, Renn JH, Tarng YW. Clinical results of using minimally invasive long plate osteosynthesis versus conventional approach for extensive comminuted metadiaphyseal fractures of the radius. Arch Orthop Trauma Surg. 2015; 135(3):361–367. PMID:
25663020.

28. Pire E, Hidalgo Diaz JJ, Salazar Botero S, Facca S, Liverneaux PA. Long volar plating for metadiaphyseal fractures of distal radius: study comparing minimally invasive plate osteosynthesis versus conventional approach. J Wrist Surg. 2017; 6(3):227–234. PMID:
28725505.

29. Zhang X, Huang X, Shao X, Zhu H, Sun J, Wang X. A comparison of minimally invasive approach vs conventional approach for volar plating of distal radial fractures. Acta Orthop Traumatol Turc. 2017; 51(2):110–117. PMID:
28246046.

30. Kapoor H, Agarwal A, Dhaon BK. Displaced intra-articular fractures of distal radius: a comparative evaluation of results following closed reduction, external fixation and open reduction with internal fixation. Injury. 2000; 31(2):75–79. PMID:
10748808.

31. Kreder HJ, Hanel DP, Agel J, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 2005; 87(6):829–836. PMID:
15911668.
32. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997; 28(Suppl 1):A42–A47. PMID:
10897286.

33. Imatani J, Noda T, Morito Y, Sato T, Hashizume H, Inoue H. Minimally invasive plate osteosynthesis for comminuted fractures of the metaphysis of the radius. J Hand Surg Br. 2005; 30(2):220–225. PMID:
15757779.

34. Sen MK, Strauss N, Harvey EJ. Minimally invasive plate osteosynthesis of distal radius fractures using a pronator sparing approach. Tech Hand Up Extrem Surg. 2008; 12(1):2–6. PMID:
18388748.

35. Wong TC, Chiu Y, Tsang WL, Leung WY, Yeung SH. A double-blind, prospective, randomised, controlled clinical trial of minimally invasive dynamic hip screw fixation of intertrochanteric fractures. Injury. 2009; 40(4):422–427. PMID:
19309606.

36. Gosens T, Bongers KJ. Neurovascular complications and functional outcome in displaced supracondylar fractures of the humerus in children. Injury. 2003; 34(4):267–273. PMID:
12667778.

37. Takada N, Otsuka T, Yamada K, et al. Minimally invasive plate osteosynthesis for distal radius fractures with a palmar locking plate. Eur J Trauma Emerg Surg. 2012; 38(6):627–632. PMID:
26814548.

38. Geissler WB, Fernandes D. Percutaneous and limited open reduction of intra-articular distal radial fractures. Hand Surg. 2000; 5(2):85–92. PMID:
11301501.

39. Porter M, Stockley I. Fractures of the distal radius: intermediate and end results in relation to radiologic parameters. Clin Orthop Relat Res. 1987; (220):241–252. PMID:
3594997.
40. Altissimi M, Antenucci R, Fiacca C, Mancini GB. Long-term results of conservative treatment of fractures of the distal radius. Clin Orthop Relat Res. 1986; (206):202–210.

41. Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand Surg Am. 1993; 18(3):492–498. PMID:
8515022.

42. Pogue DJ, Viegas SF, Patterson RM, et al. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg Am. 1990; 15(5):721–727. PMID:
2229966.

43. Short WH, Werner FW, Fortino MD, Palmer AK. Distribution of pressures and forces on the wrist after simulated intercarpal fusion and Kienbock's disease. J Hand Surg Am. 1992; 17(3):443–449. PMID:
1613217.
44. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Hoboken, NJ: John Wiley & Sons;2008. p. 256–257.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download