This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Orthopedic residents in our institute have the opportunity to participate in navigation-assisted spine surgery during their residency training. This paves the way for a new dimension of learning spine surgery, which the previous generation was not exposed to. To study this in detail, we conducted a cross-sectional descriptive survey among our residents to analyse their perception, understanding, and competency regarding pedicle screw application using spinal navigation.
Methods
We selected orthopedic residents (n = 20) who had completed 3 years of training that included at least one rotation (4–6 months) in our spine division. They were asked to respond to a four-part questionnaire that included general and Likert scale-based questions. The first two parts dealt with various parameters regarding spinal navigation and free-hand technique for applying pedicle screws. The third part dealt with residents' opinion regarding the advantages and disadvantages of spinal navigation. The final part was an objective analysis of residents' ability to identify the pedicle screw entry points in selected segments.
Results
We found that our residents were better trained to apply pedicle screws using spinal navigation. The mean Likert scale score for perception regarding their competency to apply pedicle screws using spinal navigation was 3.65 ± 0.81, compared to only 2.8 ± 0.77 when using the free-hand technique. All residents agreed that spinal navigation is an excellent teaching tool with higher accuracy and greater utility in anatomically critical cases. However, 35% of the residents were not able to identify the entry points correctly in the given segments.
Conclusions
All selected residents were perceived to be competent to apply pedicle screws using spinal navigation. However, some of them were not able to identify the entry points correctly, probably due to overreliance on spinal navigation. Therefore, we encourage residents to concentrate on surface anatomy and tactile feedback rather than completely relying on the navigation display monitor during every screw placement. In addition, incorporating cadaveric and saw bone workshops as a part of teaching program can enhance better understanding of surgical anatomy.
Go to :

Keywords: Computer-assisted surgery, Internship and residency, Neuronavigation, Pedicle screws, Spine
Spinal navigation is a relatively new technology that has revolutionised spine surgery.
1) Its fundamental purpose is to have an interactive three-dimensional real-time feedback during spine procedures to facilitate appropriate instrumentation. With the intraoperative, full-rotation, three-dimensional, O-arm-based spinal navigation, greater control and manoeuvrability is achieved, thereby allowing secure and safer implant placement in anatomically critical areas and difficult scenarios.
2) Its implications keep evolving and currently, not just limited to spinal instrumentation, but include interbody fusion, bony resection, and deformity correction of the spine.
3456)
Even though spinal navigation is not universally available, some institutions have opted for its use by trained spine surgeons. In such institutions, young surgeons, especially orthopedic residents, have the opportunity to participate in navigation-assisted spine surgery during their residency training. This paves way for a new dimension of learning spine surgery, which will definitely have an influence on their practice; however, it was not previously studied whether this would positively affect their understanding and competency to perform spinal instrumentation. Therefore, we conducted an anonymised survey among orthopedic residents to study their perception about learning spinal navigation during their residency training and its influence on their competency.
METHODS
A cross-sectional descriptive survey was formulated to assess the perception of spinal navigation among orthopedic residents who had the opportunity to participate and learn navigation-assisted pedicle screw application during their residency training. We selected residents who had completed 3 years of training with at least one rotation in our spine division and were actively involved in applying pedicle screws under supervision using spinal navigation during their rotation. We excluded the residents with under 3 years of training and those who were yet to be posted for a rotation in our spine division.
Our selected sample represents a unique set of young orthopedic surgeons who start their spine career by learning navigation-assisted spine surgery. A four-part questionnaire was formulated and distributed among the selected sample through an online portal to maintain anonymity. Responding to the questionnaire was voluntary and submission of response was interpreted as residents' implied consent to participate. The first part of the questionnaire is Likert scale-based and contains statements and questions dealing with resident's perception regarding spinal navigation. The residents had to give their level of agreement to the provided positive statements on a 5-point Likert scale, where 1, strongly disagree; 2, disagree; 3, neutral; 4, agree; and 5, strongly agree.
The first part deals with perception of understanding the concepts, level of exposure, instrumentation, confidence about screw placements, intraoperative stress anxiety, and overall satisfaction of the procedure. In addition, residents had to scale their perception of competency to apply pedicle screws on their own using spinal navigation on a scale of 5. With this data, the mean Likert scale score for all statements included in part 1 was calculated. In addition, we studied the correlation between resident's perception regarding various aspects of spinal navigation and their competency to apply pedicle screws at the end of their training by using the Spearman's correlation coefficient (ρ).
The second part of the questionnaire was drafted to learn about each resident's understanding of the entry point and trajectory during free-hand pedicle screw insertion and whether they believe that they were competent to apply pedicle screws on their own using free-hand technique. If the residents felt that they were not competent, the reason for such lack of competency was recorded.
In the third part of the questionnaire, residents were asked whether they believe that spinal navigation has advantages as a teaching tool. They were also asked to state two advantages and disadvantages of spinal navigation. In addition, residents were asked to choose one of the methods of pedicle screw application, either the free-hand technique or the navigation-assisted pedicle screw application, as the best according to their personal opinion.
In the final part of our questionnaire, images of the posterior aspect of the lumbosacral and thoracic spine models were provided, and the residents had to identify the most appropriate pedicle screw entry points for right L4, right S1, and left T8 pedicles. Responses were then reviewed by a senior spine surgeon to check if they were correct. This was done to assess each resident's understanding about the surface anatomy of the entry points.
All statistical analyses were done using Graph Pad Prism 5 (Graphpad software Inc., San Diego, CA, USA). The study was performed in accordance with the ethical standards laid down in the most recent version of the 1964 Declaration of Helsinki, or comparable ethical standards. This study (ref. No. 2018/00699) was reviewed by the National Healthcare Group (NHG) Domain Specific Review Board (DSRB), Singapore, and an exemption was granted.
Go to :

RESULTS
Orthopedic residents (n = 20) who had completed 3 years of training that included at least one rotation (4–6 months) in our spine division constituted our sample. During their spine postings, all included residents actively participated in spine procedures and had real-time experience in applying navigation-assisted pedicle screws under supervision. Even though all residents were aware about both navigation-assisted and free-hand pedicle screw application, sixteen of them (80%) were more familiar with pedicle screw application using spinal navigation. The remaining four residents (20%) were familiar with both spinal navigation and free-hand pedicle screw application.
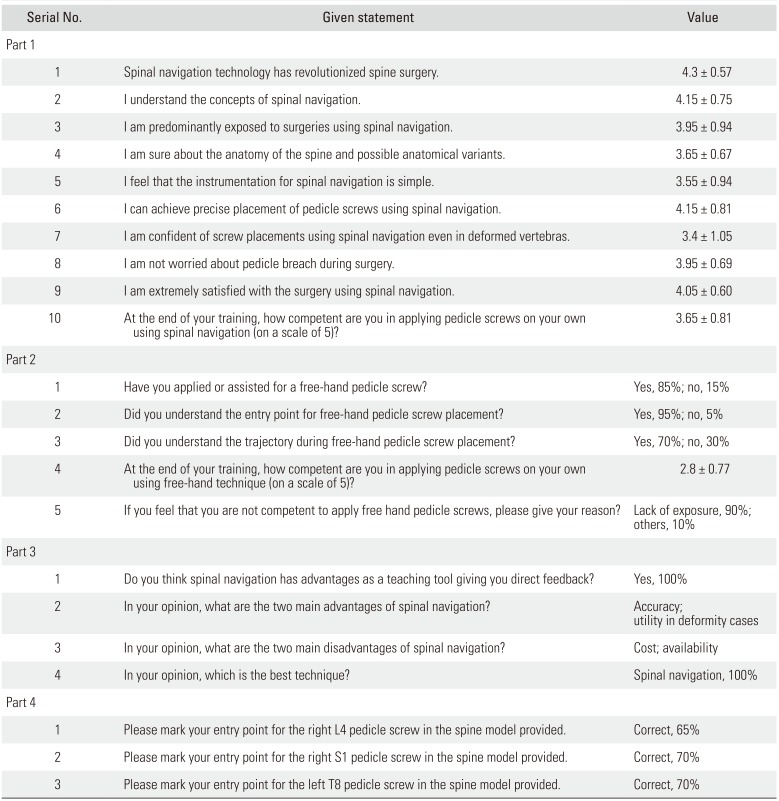
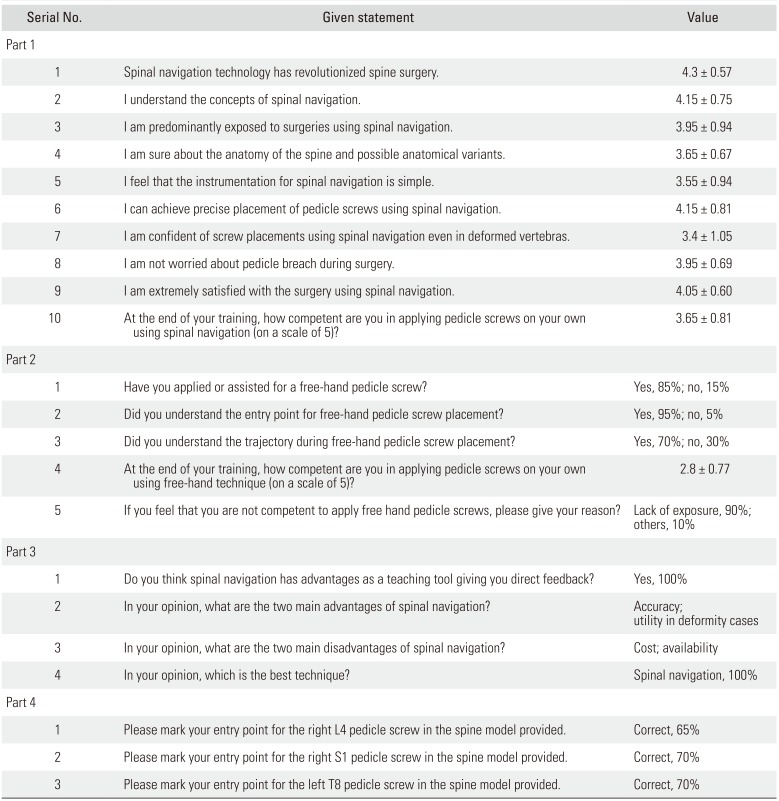
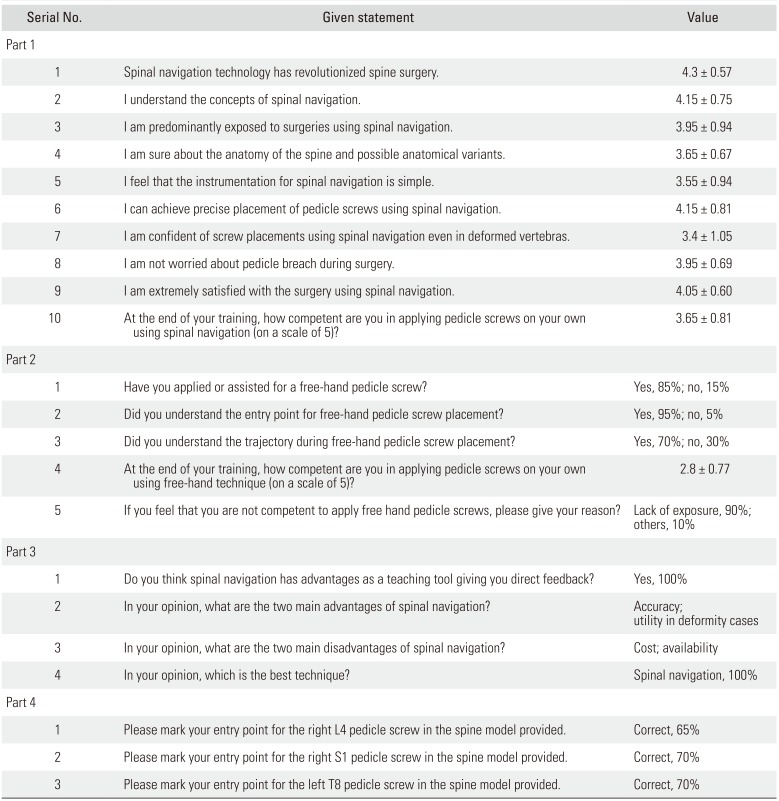
The mean Likert scale score for statements included in the first part of the questionnaire reveals a positive agreement for all included statements (
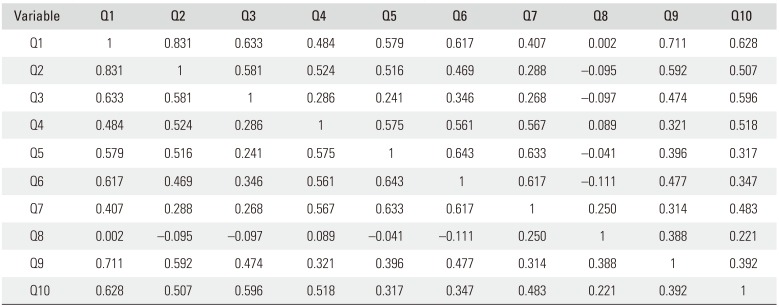
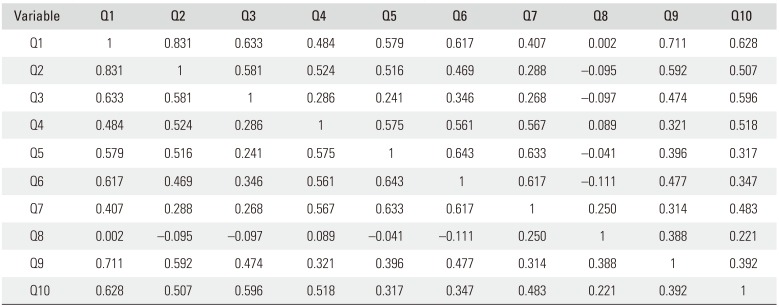
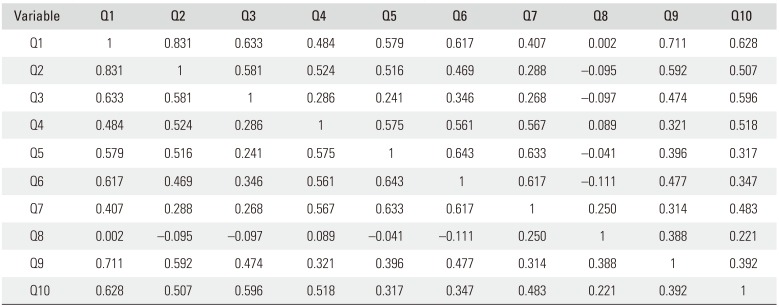
Table 1). The overall residents' perception regarding their competency to apply pedicle screws on their own using spinal navigation was 3.65 ± 0.81 on a 5-point Likert scale. Their perception of understanding the concepts, level of exposure, knowledge of instrumentation, confidence about screw placements, feeling of decreased anxiety, and overall satisfaction of the procedure positively correlated with their competency at the end of their training (
Table 2).
Table 1
Questionnaire Responses with Mean Likert Scale Scores and Percentages
|
Serial No. |
Given statement |
Value |
|
Part 1 |
|
|
|
1 |
Spinal navigation technology has revolutionized spine surgery. |
4.3 ± 0.57 |
|
2 |
I understand the concepts of spinal navigation. |
4.15 ± 0.75 |
|
3 |
I am predominantly exposed to surgeries using spinal navigation. |
3.95 ± 0.94 |
|
4 |
I am sure about the anatomy of the spine and possible anatomical variants. |
3.65 ± 0.67 |
|
5 |
I feel that the instrumentation for spinal navigation is simple. |
3.55 ± 0.94 |
|
6 |
I can achieve precise placement of pedicle screws using spinal navigation. |
4.15 ± 0.81 |
|
7 |
I am confident of screw placements using spinal navigation even in deformed vertebras. |
3.4 ± 1.05 |
|
8 |
I am not worried about pedicle breach during surgery. |
3.95 ± 0.69 |
|
9 |
I am extremely satisfied with the surgery using spinal navigation. |
4.05 ± 0.60 |
|
10 |
At the end of your training, how competent are you in applying pedicle screws on your own using spinal navigation (on a scale of 5)? |
3.65 ± 0.81 |
|
Part 2 |
|
|
|
1 |
Have you applied or assisted for a free-hand pedicle screw? |
Yes, 85%; no, 15% |
|
2 |
Did you understand the entry point for free-hand pedicle screw placement? |
Yes, 95%; no, 5% |
|
3 |
Did you understand the trajectory during free-hand pedicle screw placement? |
Yes, 70%; no, 30% |
|
4 |
At the end of your training, how competent are you in applying pedicle screws on your own using free-hand technique (on a scale of 5)? |
2.8 ± 0.77 |
|
5 |
If you feel that you are not competent to apply free hand pedicle screws, please give your reason? |
Lack of exposure, 90%; others, 10% |
|
Part 3 |
|
|
|
1 |
Do you think spinal navigation has advantages as a teaching tool giving you direct feedback? |
Yes, 100% |
|
2 |
In your opinion, what are the two main advantages of spinal navigation? |
Accuracy; utility in deformity cases |
|
3 |
In your opinion, what are the two main disadvantages of spinal navigation? |
Cost; availability |
|
4 |
In your opinion, which is the best technique? |
Spinal navigation, 100% |
|
Part 4 |
|
|
|
1 |
Please mark your entry point for the right L4 pedicle screw in the spine model provided. |
Correct, 65% |
|
2 |
Please mark your entry point for the right S1 pedicle screw in the spine model provided. |
Correct, 70% |
|
3 |
Please mark your entry point for the left T8 pedicle screw in the spine model provided. |
Correct, 70% |

Table 2
Correlation Matrix for Resident's Responses to Questionnaire's Part 1 Components
|
Variable |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
Q9 |
Q10 |
|
Q1 |
1 |
0.831 |
0.633 |
0.484 |
0.579 |
0.617 |
0.407 |
0.002 |
0.711 |
0.628 |
|
Q2 |
0.831 |
1 |
0.581 |
0.524 |
0.516 |
0.469 |
0.288 |
−0.095 |
0.592 |
0.507 |
|
Q3 |
0.633 |
0.581 |
1 |
0.286 |
0.241 |
0.346 |
0.268 |
−0.097 |
0.474 |
0.596 |
|
Q4 |
0.484 |
0.524 |
0.286 |
1 |
0.575 |
0.561 |
0.567 |
0.089 |
0.321 |
0.518 |
|
Q5 |
0.579 |
0.516 |
0.241 |
0.575 |
1 |
0.643 |
0.633 |
−0.041 |
0.396 |
0.317 |
|
Q6 |
0.617 |
0.469 |
0.346 |
0.561 |
0.643 |
1 |
0.617 |
−0.111 |
0.477 |
0.347 |
|
Q7 |
0.407 |
0.288 |
0.268 |
0.567 |
0.633 |
0.617 |
1 |
0.250 |
0.314 |
0.483 |
|
Q8 |
0.002 |
−0.095 |
−0.097 |
0.089 |
−0.041 |
−0.111 |
0.250 |
1 |
0.388 |
0.221 |
|
Q9 |
0.711 |
0.592 |
0.474 |
0.321 |
0.396 |
0.477 |
0.314 |
0.388 |
1 |
0.392 |
|
Q10 |
0.628 |
0.507 |
0.596 |
0.518 |
0.317 |
0.347 |
0.483 |
0.221 |
0.392 |
1 |

Only 17 residents (85%) had assisted for a free-hand pedicle screw application. However, 19 residents (95%) admitted that they are aware about the entry point, and 14 (70%) understood the trajectory during free-hand pedicle screw application. Even so, their overall perception regarding their competency to apply pedicle screws on their own using free-hand technique was only 2.8 ± 0.77 on a 5-point Likert scale. A majority of the residents denoted lack of exposure as the main reason for their perception of incompetency.
All residents agreed that spinal navigation is an excellent teaching tool giving direct feedback during pedicle screw application. Accuracy and utility in difficult or deformed cases were the top two advantages of spinal navigation mentioned by the residents. Cost and availability were the top two disadvantages mentioned. When asked for their personal opinion regarding which technique among the two was the best, all of them unanimously chose navigation-assisted pedicle screw application as the best technique.
Objective analysis of their efficiency to identify the most appropriate entry point for L4, S1, and T8 showed that only 65% of residents were correct with their entry point for L4 and 70% of residents were correct with their entry points for S1 and T8.
Go to :

DISCUSSION
Since the advent of pedicle screws, spine surgery has grown rapidly with technological advancements to reduce the risks associated with surgery.
7) Today, navigation-assisted spine surgery is gaining popularity for its precision, safety, and reduced radiation exposure for the surgeon.
891011) It has made complex procedures relatively easier and risk-free.
1213) Due to its increasing availability, young orthopaedic and neuro surgeons are starting to grow up with spinal navigation as a critical tool to aid spine surgery.
During residency, they usually get the opportunity to participate and obtain real-time experience in applying navigation-assisted pedicle screws. Guiding them to achieve perfect placement of every screw they perform is extremely important. For this reason, the real-time feedback visualized in the navigation display monitor itself is the guide. Moreover, the surgeon can also manipulate as required and take over if necessary.
From our survey, it was evident that almost all our orthopedic residents felt easy to use the navigation system and even agreed that the instrumentation is relatively simple. They perceived to understand the concepts of spinal navigation and be competent to apply pedicle screws on their own under supervision at the end of their training. We also noticed that our residents took only a short time to understand, learn, and be confident about navigation-assisted pedicle screw application. This implies that navigation-assisted pedicle screw application is simple, straightforward, and easy to learn.
Some would argue that overreliance on such technology will make budding spine surgeons to lose their skill in conventional techniques like the free-hand pedicle screw application. It requires a lot of precalculations to achieve flawless placement of screws using the free-hand technique.
14) Precise knowledge of the surface anatomy and probable trajectory is mandatory;
15) however, this is not always as predefined and needs modifications according to intraoperative circumstances, tactile feedback, and surgeons' perception.
1416) Repeated intraoperative imaging may be required at times, which could increase the radiation exposure to the surgeon.
1718) Yet, the procedure is not risk-free and potential pedicle breaches still remain a possibility.
19)
However, all the above said difficulties of free-hand technique of applying pedicle screws can be overcome when the procedure becomes navigation-assisted. On using the O-arm spinal navigation technology, the most important axial cut is visualized in addition to the other three-dimensional real-time views. This makes screw placements accurate and the entire procedure become stress-free.
20) This could make young surgeons increasingly dependent on spinal navigation as they grow up to be a spine surgeon. Moreover, they completely rely on the navigation display monitor rather than surface anatomy and tactile feedback.
It should be remembered that accuracy of navigation needs to be checked once in a while considering that the spine is mobile and the trackers may have moved. In that situation, if an additional spin of computed tomography scan must be avoided, the free-hand technique is the only rescue. From our survey, we noticed that our residents were neither adequately trained nor confident with the free-hand technique. Therefore, their perception of competency using spinal navigation for pedicle screw application was higher than using free-hand technique.
Furthermore, only 65% of residents identified the entry point correctly in the given segments and 35% could not do so; this was in spite of everyone admitting that they were aware about the entry points. We believe that this is due to overreliance on the navigation display monitor. With growing use of spinal navigation, it is vital to prevent this overreliance by adequately training young surgeons on free-hand technique, so that they better understand the entry point and trajectory.
For this, spinal navigation itself could be a better pedagogical tool compared to other methods of teaching as the residents get to visualize in real time of what happens exactly during pedicle screw application. Considering spinal navigation as a key demonstration tool, learning free-hand technique becomes much easier; this is because those exposed to navigation-assisted surgery not only know the exact anatomy of the spine but also are familiar with the possible anatomical variants. Therefore, it becomes easy to judge the trajectory of the pedicle screw. The only thing that they need to be familiar with is the surface anatomy for the entry point. Once that is done, surgical dexterity will significantly increase, and potential complications can be avoided.
Even though this study is first of its kind, there are certain limitations that could not be overcome. We could only select a small cohort who were adequately trained with spinal navigation during residency. Most of their learning was done during surgery and an intraoperative objective assessment of their individual ability to use spinal navigation was not possible as the surgery is of high risk and potential complications cannot be tolerated. We also did not assess individual performance in silent mentors (cadavers) or saw bone models. Despite these drawbacks, our study highlights the overreliance of spinal navigation among a selective group of residents who start using advanced technology early in their career. This may not be favorable under circumstances where technology fails. Therefore, we believe it is necessary to incorporate saw bone or silent mentor workshops to achieve comprehensive learning. In addition, we also encourage residents to concentrate on surface anatomy, tactile feedback, and finally the navigation display monitor during every screw placement.
In summary, a survey was conducted to assess orthopedic residents' perception regarding navigation-assisted pedicle screw application. All residents invariably agreed that they understood the concepts and instrumentation related to spinal navigation. They perceived to be competent to apply pedicle screws on their own using navigation by the end of their training. They believed that the advantages certainly outweigh the disadvantages. However, we noticed that they were over reliant on spinal navigation. This may not be favorable under circumstances where technology fails. Therefore, we believe it is necessary to incorporate saw bone or silent mentor workshops to enhance understanding of anatomy. In addition, we also encourage residents to concentrate on surface anatomy, tactile feedback, and finally the navigation display monitor during every screw placement. This will improve their skill, performance and overall satisfaction in growing up as a spine surgeon.
Go to :

ACKNOWLEDGEMENTS
We sincerely thank Miss Novifandona, co-ordinator of Spine Service, Department of Orthopedic Surgery, Tan Tock Seng Hospital, Singapore, for her administrative support. We also thank all the Orthopedic residents who took part in this survey.
Go to :

Notes
Go to :

References
1. Fehlings MG, Ahuja CS, Mroz T, Hsu W, Harrop J. Future advances in spine surgery: the AOSpine North America perspective. Neurosurgery. 2017; 80(3S):S1–S8.

2. Overley SC, Cho SK, Mehta AI, Arnold PM. Navigation and robotics in spinal surgery: where are we now? Neurosurgery. 2017; 80(3S):S86–S99. PMID:
28350944.

3. DiGiorgio AM, Edwards CS, Virk MS, Mummaneni PV, Chou D. Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: technical note and case series. Neurosurg Focus. 2017; 43(2):E14.

4. Zhu W, Sun W, Xu L, et al. Minimally invasive scoliosis surgery assisted by O-arm navigation for Lenke Type 5C adolescent idiopathic scoliosis: a comparison with standard open approach spinal instrumentation. J Neurosurg Pediatr. 2017; 19(4):472–478. PMID:
28186473.

5. Kosterhon M, Gutenberg A, Kantelhardt SR, Archavlis E, Giese A. Navigation and image injection for control of bone removal and osteotomy planes in spine surgery. Oper Neurosurg (Hagerstown). 2017; 13(2):297–304. PMID:
28927210.

6. Nasser R, Drazin D, Nakhla J, et al. Resection of spinal column tumors utilizing image-guided navigation: a multicenter analysis. Neurosurg Focus. 2016; 41(2):E15.

7. Mohan AL, Das K. History of surgery for the correction of spinal deformity. Neurosurg Focus. 2003; 14(1):e1.

8. Fan Chiang CY, Tsai TT, Chen LH, et al. Computed tomography-based navigation-assisted pedicle screw insertion for thoracic and lumbar spine fractures. Chang Gung Med J. 2012; 35(4):332–338. PMID:
22913860.
9. Liu Z, Jin M, Qiu Y, Yan H, Han X, Zhu Z. The superiority of intraoperative O-arm navigation-assisted surgery in instrumenting extremely small thoracic pedicles of adolescent idiopathic scoliosis: a case-control study. Medicine (Baltimore). 2016; 95(18):e3581. PMID:
27149486.
10. Navarro-Ramirez R, Lang G, Lian X, et al. Total navigation in spine surgery: a concise guide to eliminate fluoroscopy using a portable intraoperative computed tomography 3-dimensional navigation system. World Neurosurg. 2017; 100:325–335. PMID:
28104526.

11. Feng SW, Yang YJ, Li CZ, Lin MC, Chung TT, Chen YH. Accuracy of spinal screw fixation using intraoperative O-arm navigation: consecutive series of 118 screws. J Med Sci. 2016; 36(1):6–13.

12. Jaiswal A, Shetty AP, Rajasekaran S. Role of intraoperative Iso-C based navigation in challenging spine trauma. Indian J Orthop. 2007; 41(4):312–317. PMID:
21139784.

13. Kotani T, Akazawa T, Sakuma T, et al. Accuracy of pedicle screw placement in scoliosis surgery: a comparison between conventional computed tomography-based and O-arm-based navigation techniques. Asian Spine J. 2014; 8(3):331–338. PMID:
24967047.

14. Avila MJ, Baaj AA. Freehand thoracic pedicle screw placement: review of existing strategies and a step-by-step guide using uniform landmarks for all levels. Cureus. 2016; 8(2):e501. PMID:
27014535.

15. Chung KJ, Suh SW, Desai S, Song HR. Ideal entry point for the thoracic pedicle screw during the free hand technique. Int Orthop. 2008; 32(5):657–662. PMID:
17437109.

16. Puvanesarajah V, Liauw JA, Lo SF, Lina IA, Witham TF. Techniques and accuracy of thoracolumbar pedicle screw placement. World J Orthop. 2014; 5(2):112–123. PMID:
24829874.

17. Villard J, Ryang YM, Demetriades AK, et al. Radiation exposure to the surgeon and the patient during posterior lumbar spinal instrumentation: a prospective randomized comparison of navigated versus non-navigated freehand techniques. Spine (Phila Pa 1976). 2014; 39(13):1004–1009. PMID:
24732833.
18. Fransen P. Fluoroscopic exposure in modern spinal surgery. Acta Orthop Belg. 2011; 77(3):386–389. PMID:
21846009.
19. Gang C, Haibo L, Fancai L, Weishan C, Qixin C. Learning curve of thoracic pedicle screw placement using the free-hand technique in scoliosis: how many screws needed for an apprentice? Eur Spine J. 2012; 21(6):1151–1156. PMID:
22081239.

20. Choo AD, Regev G, Garfin SR, Kim CW. Surgeons' perceptions of spinal navigation: analysis of key factors affecting the lack of adoption of spinal navigation technology. SAS J. 2008; 2(4):189–194. PMID:
25802621.

Go to :