1. Chang H, Zhu Y, Zheng Z, et al. Meta-analysis shows that highly comminuted bicondylar tibial plateau fractures treated by single lateral locking plate give similar outcomes as dual plate fixation. Int Orthop. 2016; 40(10):2129–2141. PMID:
27008456.

2. Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P. Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. 2010; 34(4):565–570. PMID:
19440710.

3. Watson JT. Tibia: proximal. In : Ruedi TP, Murphy WM, editors. AO principles of fracture management. Stuttgart: Thieme;2000. p. 499–517.
4. Lee TC, Huang HT, Lin YC, Chen CH, Cheng YM, Chen JC. Bicondylar tibial plateau fracture treated by open reduction and fixation with unilateral locked plating. Kaohsiung J Med Sci. 2013; 29(10):568–577. PMID:
24099112.

5. Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010; 24(11):683–692. PMID:
20881634.

6. Nikolaou VS, Tan HB, Haidukewych G, Kanakaris N, Giannoudis PV. Proximal tibial fractures: early experience using polyaxial locking-plate technology. Int Orthop. 2011; 35(8):1215–1221. PMID:
21107983.

7. Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures: results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006; 88(12):2613–2623. PMID:
17142411.
8. Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987; 1(2):97–119. PMID:
3333518.
9. Yao Y, Lv H, Zan J, et al. A comparison of lateral fixation versus dual plating for simple bicondylar fractures. Knee. 2015; 22(3):225–229. PMID:
25747747.

10. Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop Relat Res. 2003; (412):189–195.

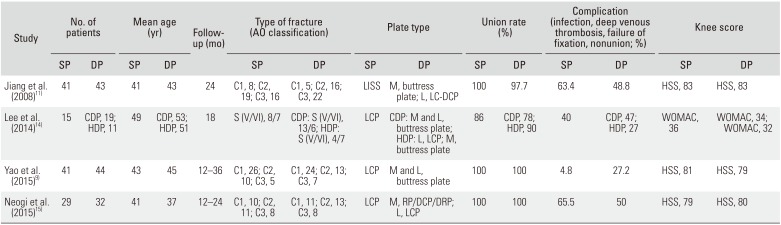
11. Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF. A comparative study of Less Invasive Stabilization System (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. Knee. 2008; 15(2):139–143. PMID:
18215801.

12. Weaver MJ, Harris MB, Strom AC, et al. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury. 2012; 43(6):864–869. PMID:
22169068.

13. Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma. 2004; 57(2):340–346. PMID:
15345983.

14. Lee MH, Hsu CJ, Lin KC, Renn JH. Comparison of outcome of unilateral locking plate and dual plating in the treatment of bicondylar tibial plateau fractures. J Orthop Surg Res. 2014; 9:62. PMID:
25038620.

15. Neogi DS, Trikha V, Mishra KK, Bandekar SM, Yadav CS. Comparative study of single lateral locked plating versus double plating in type C bicondylar tibial plateau fractures. Indian J Orthop. 2015; 49(2):193–198. PMID:
26015609.

16. Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma. 1999; 13(8):545–549. PMID:
10714780.

17. Gosling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C. Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma. 2004; 18(8):546–551. PMID:
15475851.
18. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248):13–14. PMID:
2805470.

19. Rasmussen PS. Tibial condylar fractures: impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973; 55(7):1331–1350. PMID:
4586086.
20. Whelan DB, Bhandari M, McKee MD, et al. Interobserver and intraobserver variation in the assessment of the healing of tibial fractures after intramedullary fixation. J Bone Joint Surg Br. 2002; 84(1):15–18. PMID:
11837825.

21. Ariffin HM, Mahdi NM, Rhani SA, Baharudin A, Shukur MH. Modified hybrid fixator for high-energy Schatzker V and VI tibial plateau fractures. Strategies Trauma Limb Reconstr. 2011; 6(1):21–26. PMID:
21589678.

22. El-Gafary K, El-adly W, Farouk O, Khaled M, Abdelaziz MM. Management of high-energy tibial plateau fractures by Ilizarov external fixator. Eur Orthop Traumatol. 2014; 5(1):9–14.

23. Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape HC. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. J Bone Joint Surg Br. 2009; 91(4):426–433. PMID:
19336799.

24. Barei DP, O'Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma. 2008; 22(3):176–182. PMID:
18317051.

25. Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007; 21(5):301–306. PMID:
17485994.

26. Yoo BJ, Beingessner DM, Barei DP. Stabilization of the posteromedial fragment in bicondylar tibial plateau fractures: a mechanical comparison of locking and nonlocking single and dual plating methods. J Trauma. 2010; 69(1):148–155. PMID:
20622588.

27. Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007; 21(2):83–91. PMID:
17304060.

28. Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma. 2005; 19(7):448–455. PMID:
16056075.
29. Spagnolo R, Pace F. Management of the Schatzker VI fractures with lateral locked screw plating. Musculoskelet Surg. 2012; 96(2):75–80. PMID:
22120784.

30. Kayali C, Citak C, Altay T, Kement Z. Subchondral raft construction with locking plates for the treatment of Schatzker type II fractures. Acta Ortop Bras. 2017; 25(3):99–102.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download