1. Abdel MP, Morrey ME, Jensen MR, Morrey BF. Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Joint Surg Am. 2011; 93(22):2072–2078. PMID:
22262378.

2. Jiang C, Liu Z, Wang Y, Bian Y, Feng B, Weng X. Posterior cruciate ligament retention versus posterior stabilization for total knee arthroplasty: a meta-analysis. PLoS One. 2016; 11(1):e0147865. PMID:
26824368.

3. Chalidis BE, Sachinis NP, Papadopoulos P, Petsatodis E, Christodoulou AG, Petsatodis G. Long-term results of posterior-cruciate-retaining Genesis I total knee arthroplasty. J Orthop Sci. 2011; 16(6):726–731. PMID:
21909722.

4. D'Anchise R, Andreata M, Balbino C, Manta N. Posterior cruciate ligament-retaining and posterior-stabilized total knee arthroplasty: differences in surgical technique. Joints. 2013; 1(1):5–9.
5. In Y, Kim JM, Woo YK, Choi NY, Sohn JM, Koh HS. Factors affecting flexion gap tightness in cruciate-retaining total knee arthroplasty. J Arthroplasty. 2009; 24(2):317–321. PMID:
18951761.

6. Mikulak SA, Mahoney OM, dela Rosa MA, Schmalzried TP. Loosening and osteolysis with the press-fit condylar posterior-cruciate-substituting total knee replacement. J Bone Joint Surg Am. 2001; 83(3):398–403. PMID:
11263644.

7. Rossi R, Bruzzone M, Bonasia DE, Marmotti A, Castoldi F. Evaluation of tibial rotational alignment in total knee arthroplasty: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2010; 18(7):889–893. PMID:
20057997.

8. Buechel FF Sr, Buechel FF Jr, Pappas MJ, D'Alessio J. Twenty-year evaluation of meniscal bearing and rotating platform knee replacements. Clin Orthop Relat Res. 2001; (388):41–50.

9. Laskin RS. The Genesis total knee prosthesis: a 10-year followup study. Clin Orthop Relat Res. 2001; (388):95–102.
10. Bae DK, Song SJ, Kim KI, Hur D, Lee HH. Intraoperative factors affecting conversion from cruciate retaining to cruciate substituting in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016; 24(10):3247–3253. PMID:
26733275.

11. Laskin RS, O'Flynn HM. The Insall Award. Total knee replacement with posterior cruciate ligament retention in rheumatoid arthritis: problems and complications. Clin Orthop Relat Res. 1997; (345):24–28.
12. Archibeck MJ, Berger RA, Barden RM, et al. Posterior cruciate ligament-retaining total knee arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2001; 83(8):1231–1236. PMID:
11507132.

13. Dennis DA, Clayton ML, O'Donnell S, Mack RP, Stringer EA. Posterior cruciate condylar total knee arthroplasty: average 11-year follow-up evaluation. Clin Orthop Relat Res. 1992; (281):168–176. PMID:
1499205.
14. Reinhardt KR, Huffaker SJ, Thornhill TS, Scott RD. Cruciate-retaining TKA is an option in patients with prior patellectomy. Clin Orthop Relat Res. 2015; 473(1):111–114. PMID:
25002212.

15. Scott WN. Insall & Scott surgery of the knee. 6th ed. Philadelphia, PA: Elsevier;2018. p. 1502–1508.
16. Bae DK, Song SJ, Yoon KH, Noh JH, Moon SC. Comparative study of tibial posterior slope angle following cruciate-retaining total knee arthroplasty using one of three implants. Int Orthop. 2012; 36(4):755–760. PMID:
22143313.

17. Mihalko WM, Miller C, Krackow KA. Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop (Belle Mead NJ). 2000; 29(8):610–616. PMID:
10955465.
18. Baldini A, Castellani L, Traverso F, Balatri A, Balato G, Franceschini V. The difficult primary total knee arthroplasty: a review. Bone Joint J. 2015; 97(10 Suppl A):30–39. PMID:
26430084.
19. Su EP. Fixed flexion deformity and total knee arthroplasty. J Bone Joint Surg Br. 2012; 94(11 Suppl A):112–115. PMID:
23118396.

20. Lombardi AV Jr, Berend KR. Posterior cruciate ligament-retaining, posterior stabilized, and varus/valgus posterior stabilized constrained articulations in total knee arthroplasty. Instr Course Lect. 2006; 55:419–427. PMID:
16958477.
21. Berend KR, Lombardi AV Jr, Adams JB. Total knee arthroplasty in patients with greater than 20 degrees flexion contracture. Clin Orthop Relat Res. 2006; 452:83–87. PMID:
16957650.

22. Lombardi AV Jr, Mallory TH, Fada RA, et al. An algorithm for the posterior cruciate ligament in total knee arthroplasty. Clin Orthop Relat Res. 2001; (392):75–87.

23. Chiu YS, Chen WM, Huang CK, Chiang CC, Chen TH. Fracture of the polyethylene tibial post in a NexGen posterior-stabilized knee prosthesis. J Arthroplasty. 2004; 19(8):1045–1049. PMID:
15586342.

24. Cheng FB, Ji XF, Lai Y, et al. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee. 2009; 16(5):341–347. PMID:
19230678.

25. Hitt K, Shurman JR 2nd, Greene K, et al. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003; 85-A(Suppl 4):115–122. PMID:
12533581.
26. Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty. 2000; 15(1):79–85. PMID:
10654467.

27. Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E. Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc. 2013; 21(10):2314–2324. PMID:
23404515.

28. Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010; 92(5):1115–1121. PMID:
20439656.

29. Dai Y, Scuderi GR, Penninger C, Bischoff JE, Rosenberg A. Increased shape and size offerings of femoral components improve fit during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014; 22(12):2931–2940. PMID:
25026932.

30. Ji SJ, Zhou YX, Jiang X, et al. Effect of joint line elevation after posterior-stabilized and cruciate-retaining total knee arthroplasty on clinical function and kinematics. Chin Med J (Engl). 2015; 128(21):2866–2872. PMID:
26521783.

31. Aglietti P, Buzzi R, Gaudenzi A. Patellofemoral functional results and complications with the posterior stabilized total condylar knee prosthesis. J Arthroplasty. 1988; 3(1):17–25. PMID:
3361317.

32. Sierra RJ, Berry DJ. Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty. 2008; 23(7 Suppl):20–23.

33. Aoki M, Shishido T, Takahashi Y, et al. Functional evaluation in cruciate-retaining-type TKA: anatomical relationship between tibial osteotomy level and PCL attachment. Eur J Orthop Surg Traumatol. 2014; 24(8):1531–1537. PMID:
24442384.

34. Sessa P, Fioravanti G, Giannicola G, Cinotti G. The risk of sacrificing the PCL in cruciate retaining total knee arthroplasty and the relationship to the sagittal inclination of the tibial plateau. Knee. 2015; 22(1):51–55. PMID:
25487301.

35. Van Opstal N, Feyen H, Luyckx JP, Bellemans J. Mean tensile strength of the PCL in TKA depends on the preservation of the tibial insertion site. Knee Surg Sports Traumatol Arthrosc. 2016; 24(1):273–278. PMID:
25308158.

36. Okazaki K, Tashiro Y, Mizu-uchi H, Hamai S, Doi T, Iwamoto Y. Influence of the posterior tibial slope on the flexion gap in total knee arthroplasty. Knee. 2014; 21(4):806–809. PMID:
24856090.

37. Takayama K, Matsumoto T, Kubo S, et al. Influence of intraoperative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012; 20(3):532–537. PMID:
21720891.

38. Dennis DA, Komistek RD, Colwell CE Jr, et al. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res. 1998; (356):47–57.
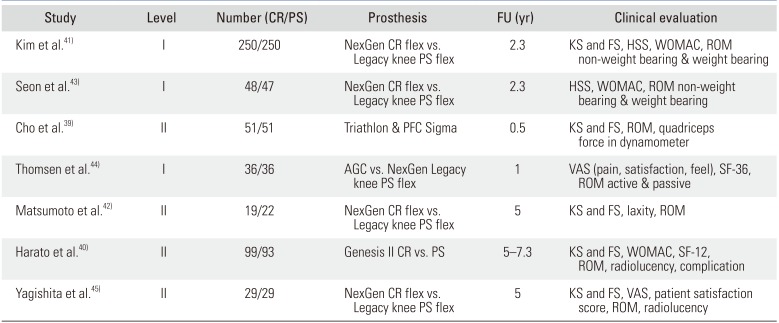
39. Cho KY, Kim KI, Song SJ, Bae DK. Does cruciate-retaining total knee arthroplasty show better quadriceps recovery than posterior-stabilized total knee arthroplasty? Objective measurement with a dynamometer in 102 knees. Clin Orthop Surg. 2016; 8(4):379–385. PMID:
27904719.
40. Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD. Midterm comparison of posterior cruciate-retaining versus-substituting total knee arthroplasty using the Genesis II prosthesis: a multicenter prospective randomized clinical trial. Knee. 2008; 15(3):217–221. PMID:
18325770.
41. Kim YH, Choi Y, Kwon OR, Kim JS. Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses: a prospective, randomized study. J Bone Joint Surg Am. 2009; 91(4):753–760. PMID:
19339558.
42. Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R. Intraoperative soft tissue balance reflects minimum 5-year midterm outcomes in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Arthroplasty. 2012; 27(9):1723–1730. PMID:
22554731.

43. Seon JK, Park JK, Shin YJ, Seo HY, Lee KB, Song EK. Comparisons of kinematics and range of motion in high-flexion total knee arthroplasty: cruciate retaining vs. substituting designs. Knee Surg Sports Traumatol Arthrosc. 2011; 19(12):2016–2022. PMID:
21331651.

44. Thomsen MG, Husted H, Otte KS, Holm G, Troelsen A. Do patients care about higher flexion in total knee arthroplasty? A randomized, controlled, double-blinded trial. BMC Musculoskelet Disord. 2013; 14:127. PMID:
23565578.

45. Yagishita K, Muneta T, Ju YJ, Morito T, Yamazaki J, Sekiya I. High-flex posterior cruciate-retaining vs posterior cruciate-substituting designs in simultaneous bilateral total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2012; 27(3):368–374. PMID:
21680139.
46. Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M. In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty. 2005; 20(6):777–783. PMID:
16139716.

47. Hamai S, Okazaki K, Shimoto T, Nakahara H, Higaki H, Iwamoto Y. Continuous sagittal radiological evaluation of stair-climbing in cruciate-retaining and posterior-stabilized total knee arthroplasties using image-matching techniques. J Arthroplasty. 2015; 30(5):864–869. PMID:
25618811.

48. Murakami K, Hamai S, Okazaki K, et al. Kinematic analysis of stair climbing in rotating platform cruciate-retaining and posterior-stabilized mobile-bearing total knee arthroplasties. Arch Orthop Trauma Surg. 2017; 137(5):701–711. PMID:
28289890.

49. Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003; 85(2):259–265. PMID:
12571303.

50. Kremers HM, Sierra RJ, Schleck CD, et al. Comparative survivorship of different tibial designs in primary total knee arthroplasty. J Bone Joint Surg Am. 2014; 96(14):e121. PMID:
25031383.

51. Dennis DA, Kim RH, Johnson DR, Springer BD, Fehring TK, Sharma A. The John Insall Award: control-matched evaluation of painful patellar Crepitus after total knee arthroplasty. Clin Orthop Relat Res. 2011; 469(1):10–17. PMID:
20706813.

52. Nam D, Barrack T, Nunley RM, Barrack RL. What is the frequency of noise generation in modern knee arthroplasty and is it associated with residual symptoms? Clin Orthop Relat Res. 2017; 475(1):83–90. PMID:
26762299.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download