Abstract
Purpose
We report a case of postoperative endophthalmitis in the cataract patient, associated with removal of an intralenticular foreign body that had remained in place without symptoms for 20 years.
Case summary
A 45-year-old male visited our outpatient clinic complaining of gradual visual loss in his right eye over the past 3 months. In slit-lamp examinations, anterior capsular opacification, nuclear sclerosis, and posterior subcapsular opacity were observed in the right eye. Twenty years before, a tiny metallic projectile had hit his right eye, but slit-lamp examination at the time of injury did not reveal any intraocular foreign body. We decided to undergo cataract surgery. During phacoemulsification, a metallic foreign body was found in the lens and safely removed; then an intraocular lens was implanted. As hypopyon was evident 3 days later, we injected intravitreal antibiotics and applied fortified antibiotic eye drops to the right eye. The anterior chamber inflammation improved and the best-corrected visual acuity recovered to 1.0.
Figures and Tables
Figure 1
Anterior segment photographs of the patients at the first visit. Anterior capsular opacification and nuclear sclerosis were found in the right eye (A) and a small corneal opacity was observed in the center of the right cornea, which was considered to be a sign of previous penetration (B).
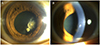
Figure 2
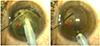
Intraoperative photographs. An intralenticular metallic foreign body found during phacoemulsification (red arrow) (A) and the posterior capsule was intact (B).
Notes
This study was supported in part by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (2018R1C1B6002794), by a Korea University Ansan Hospital Grant (K1811051), and by Alumni of department of ophthalmology, Korea University College of Medicine in 2018. This work was presented in part at the 118th Meeting of the Korean Ophthalmological Society, Seoul, South Korea, November 3-5, 2017.
References
1. De Juan E Jr, Sternberg P Jr, Michels RG. Penetrating ocular injuries. Types of injuries and visual results. Ophthalmology. 1983; 90:1318–1322.
2. Ahn M. Noninfectious endophthalmitis caused by an intraocular foreign body retained for 16 years. J Korean Ophthalmol Soc. 2001; 42:793–796.
3. Coleman DJ, Lucas BC, Rondeau MJ, Chang S. Management of intraocular foreign bodies. Ophthalmology. 1987; 94:1647–1653.

4. Cazabon S, Dabbs TR. Intralenticular metallic foreign body. J Cataract Refract Surg. 2002; 28:2233–2234.

5. Chang YS, Jeong YC, Ko BY. A case of an asymptomatic intralenticular foreign body. Korean J Ophthalmol. 2008; 22:272–275.

6. Dhawahir-Scala FE, Kamal A. Intralenticular foreign body: a D-Day reminder. Clin Exp Ophthalmol. 2005; 33:659–660.

7. Arora R, Sanga L, Kumar M, Taneja M. Intralenticular foreign bodies: report of eight cases and review of management. Indian J Ophthalmol. 2000; 48:119–122.
8. Berrocal AM, Davis JL. Uveitis following intraocular surgery. Ophthalmol Clin North Am. 2002; 15:357–364. vii.

9. Hinkelmann L, Struck HG, Lautenschläger C. Inflammatory reaction of the anterior eye segment. Cataract extraction in patients with and without diabetes mellitus. Ophthalmologe. 1998; 95:213–218.
10. Trocme SD, Li H. Effect of heparin-surface-modified intraocular lenses on postoperative inflammation after phacoemulsification: a randomized trial in a United States patient population. Heparin-Surface-Modified Lens Study Group. Ophthalmology. 2000; 107:1031–1037.
11. Irvine WD, Flynn HW Jr, Murray TG, Rubsamen PE. Retained lens fragments after phacoemulsification manifesting as marked intraocular inflammation with hypopyon. Am J Ophthalmol. 1992; 114:610–614.
12. Choi SC, Cho HJ, Kim HS, et al. Analysis of referred 113 patients with endophthalmitis after cataract surgery and associated prognostic factors. J Korean Ophthalmol Soc. 2016; 57:420–428.

13. Lapira M, Karl D, Murgatroyd H. Siderosis bulbi as a consequence of a missed intraocular foreign body. BMJ Case Rep. 2014; 2014:pii: bcr2013202904.

14. Mamas N, Andreanos K, Brouzas D, et al. Acute ocular pain during magnetic resonance imaging due to retained intraocular metallic foreign body: the role of ultrasonography and ultrasound biomicroscopy in diagnosis and management of this condition. J Ultrasound. 2018; 21:159–163.

15. Endophthalmitis Study Group. European Society of Cataract & Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007; 33:978–988.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download